Unraveling Restorations
An Overview of Restorative Materials and Their Relationship to Dental Hygiene Treatment
by Lois N. Dreyer, RDH, MS
The process of assessment, evaluation, and documentation of a patient’s restorative portrait is a necessary component of comprehensive dental hygiene care. If existing dental work has failed or was poorly constructed, it can undermine the outcome of periodontal treatment or necessitate longer, less comfortable hygiene appointments.
Assessment of the existing landscape - through direct observation and radiographs - not only helps the hygienist to effectively plan, it also identifies conditions that might require professional intervention or reveal conditions under which materials may succeed or fail.
Future operative needs impact periodontal debridement, maintenance plans, patient self-care plans, and appointment experiences. New dental work may require a more extensive home-care routine, and a patient’s willingness or ability to comply may affect the success of the restorations.
Understanding restorative choices offered by the dental plan can be challenging to the patient. Questions relating to material safety, cost, esthetic preferences, longevity, professional and patient care of the materials used may arise during hygiene treatment, and the dental hygienist is in a unique position to respond.
Historically, the use of artificial materials to replace lost tooth structure dates back to before the Christian era. Early Chinese dynasties used materials as complex as today’s amalgams to replace lost tooth structure and restore function. The aim of contemporary restorative dentistry is not only to replace the lost tooth structure to it original function, but to do so in the most natural looking manner possible.1
The integrity of restorative margins and contours is of concern to the hygienist. Marginal irregularities can interfere with plaque control, decrease the life expectancy of a restoration, and necessitate modifications in the choice of treatment armamentarium.
Fabricated anatomical contours such as contact areas, embrasure spaces, and margins should mimic sound tooth anatomy. They should be smooth to support home care and retard plaque retention. The surrounding soft tissue should not suffer from pinching or displacement interproximally or at the gingival margin. Depending upon the materials used, irregularities may be corrected in situ with the use of hand or power-driven instruments. Other defects may necessitate the total replacement of the restoration.
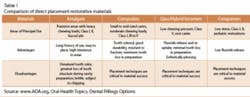
Current materials have properties that allow the dentist to individualize restoration choices for their patients. Generally speaking, restorations can be divided into two broad restorative categories:
- Direct, which can be placed in a cavity preparation in one visit, such as amalgams
- Indirect, which are fabricated outside the oral cavity prior to placement, such as porcelain and metal alloys
Direct Restorative Materials
Amalgam has been in use for more than 100 years. It is durable, easy to use, highly resistant to wear, and relatively inexpensive in comparison to other materials. A stable alloy made by combining elemental mercury, silver, tin, copper, and possibly other metallic elements, dental amalgam is a safe restorative material. It is biocompatible and well tolerated by patients with only rare occurrences of allergic response.
Despite patient concerns about its mercury content, major U.S. and international scientific and health bodies (the National Institutes of Health, the U.S. Public Health Service, the Centers for Disease Control and Prevention, the Food and Drug Administration, and the World Health Organization, among others) have deemed dental amalgam a safe, reliable and effective restorative material.2
The strength and durability of this traditional dental material continues to make it the material of choice in posterior teeth where masticatory forces are greatest. This material can be used in many clinical applications, as it is moderately tolerant of moisture during placement.3
The disadvantages of amalgam include possible short-term sensitivity to hot or cold after placement and an unnatural looking color. Because amalgam does not bond to the tooth, undercuts in the tooth structure are necessary in order to mechanically lock the material in place.
This purely physical attachment between tooth and material leaves a space, known as ditching, which may allow for microleakage of bacteria into the area. Over time, corrosion seals the space, but the lack of a bond leaves the tooth weaker then before the tooth was prepped. Due to the nature of this material, the hygienist must be on the lookout for the slow, continual degradation of the margins of the restoration. Other marginal irregularities can be identified during assessment. Although they may be a direct result of faulty material placement and not material failure, they must be addressed.1
Recent products have been introduced to attempt to bond dental amalgam to the tooth. These products do appear to strengthen the attraction between the tooth and the restoration, thus reducing leakage. Their routine use in practice is promising.
Direct Esthetic Restorative Materials
In 1960, tooth-colored restorative materials known as direct esthetic dental restorative materials (DERM) began to replace amalgam as the material of choice. Four types of DERM are in use today. Selection criteria is dependent upon a need for esthetics, fluoride release properties, wear resistance, strength, and ease of use.5
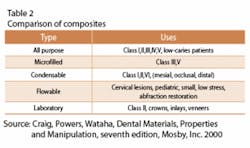
Composites, which were introduced in 1960, are the dominant member of the group. These materials are made of a resin matrix into which an inorganic filler material is dispersed. It is held together by a silicone coupling agent that produces a bond between the matrix and the filler. Depending upon the diameter of the fillers used, the composite is considered either a microhybrid (containing a blend of fine and microfine filler particles) or a microfilled composite (microfine fillers only).
Clinically, they are strong, wear-resistant, and useful in the treatment of small to mid-sized caries in areas that need to withstand moderate chewing pressure. They provide good durability, resistance to fracture, and less tooth structure is removed when preparing the tooth. In comparison to amalgam. composites can also be “bonded” or adhesively held in a cavity prep, often allowing a more conservative repair to the tooth. In the laboratory, indirect composites are processed to increase polymerization and wear resistance.
The cost is moderate and depends on the size of the restoration and the placement technique.4 It is generally more difficult to place a composite than an amalgam, and marginal adaptation can be faulty. However, recurrent decay is low and color change is minimal. They are subject to stain and discoloration over time, and loss of surface contour is seen due to wear from toothbrushing and chewing. If used posteriorly, there is wear at the contact area where stresses are the greatest.
Postoperatively, sensitivity has been reported in about 10 percent of cases. This has been linked to bacterial microleakage and induced internal stress. If used occlusally opposite a porcelain restoration, the composite restoration will abrade it.
In areas not subject to heavy chewing pressure, such as Class Vs, glass ionomers are used. Introduced in 1972, glass ionomers are ideal for high-risk caries patients since they release the greatest amount of fluoride over a two-year period.3 The preparation site requires the removal of less tooth structure than for amalgams.4 These materials have a coefficient of expansion similar to tooth structure and have proven to have a better retention rate as compared to composites when used in areas of cervical erosion.3
Although these resins mimic natural tooth color, they do not have the same degree of translucency as composites. Some glass ionomers require a delay of 24 hours before polishing.3 This material is well tolerated by patients, and only rare incidences of allergic responses are reported.4
Hybrid ionomers have been in use since the early 1990s and are also used for high-risk caries patients in low stress-bearing areas. Because they are a resin-modified material, they are even more esthetically pleasing than glass ionomers. Both of these filling materials can be “recharged” with fluoride, either through the use of a fluoride toothpaste or professional treatments.6
The latest addition to the DERM family is the compomers that arrived on the market in 1995. These modified composites are recommended for medium-risk caries patients, because their duration and release of fluoride is lower than glass and hybrid ionomers. However, they cannot be recharged. Usually placed in areas of low stress, the manufacturer of a recent product, (Dyract AP), has advocated its use in Class I and II restorations.
Indirect Restorative Materials
As our population continues to age, an era of conservative dentistry has emerged. As with direct restorations, patients are requesting natural-looking tooth replacements. Preserving bone and tooth structure through the use of innovative materials and techniques has become a commitment to our patients who can expect to maintain a functional dentition for a lifetime.7
Inlays and onlays are necessary when intermediate or moderate breakdown results in teeth that can no longer structurally support a restoration. If neither of these options are available to the patient, crowns are necessary. In anterior teeth, where severe staining or enamel defects have occurred, veneers are indicated. Restorations of this type, which are fabricated in the lab, are called indirect and generally require two or more visits. They are created from an impression, cemented or bonded into the prepared cavity, and adjusted as needed.8 Materials used for the fabrication of these restorations include composites, metals, porcelain, and ceramics.
Gold, in the form of an alloy, has been the most widely used material for the fabrication of restorations of this kind. Highly resistant to corrosion and tarnishing, gold alloys have high strength and resist fracture and wear. Because of its toughness, tooth structure can be preserved during the preparation. Gold alloys are extremely biocompatible and do not abrade opposing tooth structure.
Today, new indirect composite restorative systems, such as Tescera ATL, produce materials that can be fabricated into crowns, inlays, and onlays, replacing traditional cast gold. These materials satisfy the patient’s esthetic desires and reinforce remaining tooth structure, thereby preserving as much tooth structure as possible.8
Base metal alloys (non-noble metals) have a silver appearance and are used in crowns, bridges, and partial dentures. Resistant to corrosion and tarnish, they are tough, high strength, and resistant to fracture and wear. Some patient may be allergic to base metals, and there may be initial sensitivity to temperature swings.4
Porcelain, a type of dental ceramic, has been used as a replacement material since the 1700s. Completely insoluble in oral fluids, it is highly compatible with soft tissue and resistant to wear. However, because it is inherently brittle, porcelain is traditionally fused to a metal base when used to fabricate a crown. This metal framework supports the porcelain and makes it more durable under the load of oral stresses.3
Porcelain is a translucent material with surface reflectance and fluorescence that mimics natural tooth structure. It is, therefore, an exceptional esthetic choice. However, its construction and placement is exacting. Unless this material is cared for, it may become rough on the occlusal and incisal surfaces, which can abrade opposing tooth enamel.
As an alternative, an all-ceramic crown offers excellent esthetics. Because they do not rely on a metal framework, the entire thickness of the material allows for a natural, life-like look. Originally introduced in the early 1900s, ceramics today are often fabricated over an all porcelain core, increasing strength while preserving esthetics. They can be used in select posterior areas but they are still not as strong as the traditional porcelain fused-to-metal restoration. Ceramics are also used extensively for veneers which are intended to replace only facial and incisal portions of anterior teeth.3
Patients and providers want restorations to last as long as possible, both esthetically and functionally. When assessing patients, the dental hygienist documents the functional effectiveness of existing restorations. This, coupled with an understanding of restorative options and an assessment of the patient’s self-care abilities, will support the success of both the operative dental treatment plan and continued professional dental hygiene care.
About the Author
Lois N. Dreyer, RDH, MS, is an associate professor in the Department of Dental Hygiene, New York City College of Technology.
References
1. Philips R. , Moore B. , Elements of Dental Materials for Dental Hygienists and Dental Assistants, 5th edition, Saunders 1994
2. “Dental Amalgam: Update on Safety Concerns” Association Report, JADA, Vol.129, April 1998.
3. Craig, Powers, Wataha, Dental Materials, Properties and Manipulation, seventh edition, Mosby, Inc. 2000
4. www.ADA.org, Oral Health Topics; Dental Fillings Options
5. “The Need for Caries-Preventive Restorative Materials”, Christensen, G., J Am Dent Assoc, Vol 131, No 9, 1347-1349.
6. Weidlich, Patricia; Miranda, Leticia, Algraves; Maltz, Marisa and Samuel, Suzanna Matria Werner; Fluoride Release and Uptake from Glass Ionomer Cements and Composite Resins, Brazilian Dental Journal (2000( 11(2): 89-96.
7. Graham, L “Accomplishing the Parameters of Long-Term Tooth Preservation”, Contemporary Esthetics and Restorative Practice, December 2004.
8. Jackson, R., Restorative Quarterly, Vol 5, No 3, November, 2002.
9. Wilkins, E. “ Clinical Practice of the Dental Hygienist”, Ninth Edition, Lippincott, Williams and Williams, 2005
Treatment Considerations
Restorative materials are relevant to dental hygienists during all phases of care. During the treatment assessment phase, exploration and identification of restorations - as well as the surrounding tissue - may be hampered by well-matched tooth materials, faulty margins, or poorly fabricated restorations. Patients’ recollections of past treatment can help in the identification of restorative materials. Notations concerning the type of materials used should be made in the patient record. Documentation of marginal irregularities through exploration and use of radiographs will allow the clinician to modify probing and scaling angulations, instrument selection (as well as stroke direction and lateral pressure), and home care instruction.
Generally speaking, composites feel softer than enamel or porcelain when exploring and scaling. Also, a black line may appear when exploring across a composite.9 Most microhybrid composites are radiopaque when compared to dentin and radiolucent when compared to enamel. Helimolar, which is a microfilled composite, is radiolucent because of an added material.3 DERMs may also appear chalky when subjected to a stream of air.
When scaling porcelain and composites, the use of an ultrasonic scaler is contraindicated. Porcelain may fracture or lose marginal integrity. Composites have shown surface alterations, and amalgams have shown a loss of marginal integrity and surface damage.9
Overhanging margins can occur either sub- or supragingivally on any tooth surface with both amalgam and composites. It is the direct result of improper matrix band or wedge placement, incorrect manipulation of the material, or inadequate finishing techniques. Viewed interproximally on a radiograph, it can be seen just above or below where the margin of the matrix band would have been seated. A thin veneer of material found on the occlusal or proximal/gingival surfaces and extending over the cavity prep margin is called flash.
When exploring interproximally, this mass will resemble a calculus deposit but will not respond to simple scaling techniques. It may fill an embrasure space, hindering access to the sulcus or pocket during treatment. Dense amalgam overhangs have been know to fracture instruments during scaling. Both flash and overhang can cause home care problems for the patient. Dental floss can fray and tear rendering it ineffective, or it can become lodged interproximally.
It is possible to correct the overhang if it is small to moderate in size, it is not fractured at the cavity margin, the proximal contact is intact, there is no secondary decay, and instrument access to the area will not damage an adjacent tooth. If these parameters are not met, replacement is warranted.
If the restoration is able to be saved by recontouring, the following techniques are suggested:
- When using hand instruments, use only a rigid scaler to get the strong lateral pressure needed. A universal curet is activated in an oblique direction across the junction of the material and tooth.
- Narrow, fine, or medium finishing strips can be used after gross amalgam is removed. Maintenance of the contact point is achieved by cutting the edge of the strip diagonally and passing through the embrasure space. Be sure to avoid contact with adjacent tooth as the cementum is vulnerable to wear.
- Periodontal files, which are used to crush or roughen the surface of a deposit in preparation to scaling with either a scaler or a curet, may be used with limited success on an overhanging filling. Tissue displacement is usually more severe with files, and their design limits the placement depth within the sulcus.
- Power-driven instruments create heat that may cause pulpal damage or an alteration of chemical structure of the material. Tooth sensitivity may occur. If used, light, intermittent strokes in a multidirectional motion are preferable.
Be cautious when using a disclosing agent on DERMs, as the coloring agent may be absorbed. Tobacco will also stain composites. Acidulated phosphate fluoride or stannous fluoride may cause an alteration of the filler material as well as staining. These fluorides should not be used if the patient has porcelain restorative work. Alcohol-containing mouth rinses may act as a solvent that might soften composite material, rendering it rougher and more easily stained.