'Oops!' happens
Dear Dianne,
I have been a hygienist for 20 years. I love the profession of dental hygiene, and I take pride in the quality of care I deliver.
However, a few days ago, an unfortunate incident occurred with one of my patients. I forgot to put the lead apron on her when I took an X-ray. Actually, I was taking four bitewings. After the first film, the patient asked me why I had not put the lead shield on her. I was both shocked and embarrassed at my momentary lack of diligence. I placed the shield on her for the remaining films, and I apologized for my forgetfulness. I finished her appointment without further incident.
After the patient left, the doctor called me aside to inform me that this patient had requested not to be scheduled with me for future appointments. I was very hurt and troubled over this patient's lack of trust in me. In an effort to do some 'damage control,' I composed a letter apologizing for my error. I showed the doctor the letter, and he said not to send it. However, I'd like your input on this situation. I just want to do the right thing.
Any patient's lack of trust in me is something I take very seriously. Because of this, I will strive with even more effort to guarantee I do not cause a breach of confidence with any other patient.
Feeling Bad in Baltimore
Dear Feeling Bad,
Whether we want to admit it or not, we all forget things from time to time. There is not a hygienist or doctor alive that hasn't committed an "oops" at some time. I shudder to think of some of the "oops" I've committed over the years — forgetting to record in the patient chart; spilling disclosing solution on my patient; dislodging restorations with my curettes; charting incorrectly; inadvertently squirting water in my patient's ear or nose; and, yes, forgetting the lead shield.
Your particular situation prompted me to do some research into the use of lead shielding. Before 1980, X-ray machines were not required to have lead-lined cones that collimated (direct in a straight line) the primary beam. Consequently, when the exposure was made, radiation scattered throughout the room. Those of us who graduated before 1980 remember the pointed plastic cones. It was very hard for some doctors to give up their pointed cones. In my first dental hygiene position, the doctor and I were always changing the cone. He would unscrew my collimating cone and place the pointed cone on the machine. When I needed an X-ray, I would unscrew his pointed cone and replace it with the collimating cone. One day, I accidentally dropped the pointed cone and broke it. Unfortunately (or fortunately!), that brought an end to the "changing the cone" routine!
The use of lead-lined cones limits the beam to the diameter of the collimating device. This significantly reduces the amount of scatter radiation. The primary beam is confined to the small space on the face where it is directed.
Recently, I was in an office and observed an assistant take several panoramic films on a very modern panoramic machine. When I asked why none of the patients were shielded, the assistant told me that the company rep told them not to use a shield, as it would affect the quality of the film. I spoke with a company rep at a major dental meeting a few days later and asked about this issue. He said that the company does recommend shielding with a full upper torso shield.
When I queried my astute colleagues on the Internet Dental Forum about shielding, I received some surprising replies. Here are some examples:
• "The only time we use lead aprons in our office is on pregnant patients."
• "It is extremely remote that anyone would even listen to someone claiming that this one exposure led to an injury."
• "Some places are actually requiring that shielding not be used. I'd tell the patient that it's a formality stemming from old equipment that had much more scatter and was not collimated like our current versions."
• "Most state boards know that something like this is nonsense. We all have skeletons in our closets, and I wish mine were as minor as this one."
• "The doctor has to step up and take responsibility here. The patient should be contacted by the doctor and told that the error was fortunately minor and does not reflect on the office policy concerning radiation hygiene nor on the quality of the care delivered by the hygienist. It was a definitely a mistake, the hygienist acknowledges it and feels very bad about it and thankfully no harm will come to the patient because of it. (I once filled the wrong tooth!)"
• "We don't use aprons with panoramic films. We do use them for PAs and BWs, probably out of expectation more so than need since patients expect it. However, I doubt the need exists with digital, but expectation is still there. So why not supply it?"
• From an Australian doctor: "We used to use a thyroid guard before digital and a lead apron only if the patient was pregnant. With digital we don't bother with the thyroid guard but probably would still use the lead apron on a pregnant woman (although I think it would be a waste of time)."
• "Have you had your gonads or thyroid covered at the MDs or ER when you have had an ankle or knee or chest X rayed? I have not! The patient is uneducated. Show her how you have your 'machines' tested each year and then ask her about other X-rays. And, of course, she is not a smoker, overeater, or, God forbid, eats in restaurants with second-hand smoke."
• "I can't see where a lead shield has ever been indicated for panoramic radiography as most of the scatter would be occurring from behind the lead shield anyway. Much of the shot occurs with the tube head behind the patient as well. The lead absorbs rather than reflects for the most part though, so I doubt it causes an increase. Just doesn't really make a positive difference."
Several doctors made some interesting "relative risk" comparisons. For example, one doctor said: "57 dental X-rays = an afternoon at the beach." Another doctor quoted an Australian radiology instructor as saying: "1 BWX = 1 cigarette." One of my former bosses used to tell patients that they get significantly more radiation exposure from their color televisions than dental X-rays.
While possibly true, such statements are hard to support, since we can't accurately quantify the risks of one cigarette or one BWX as an isolated event. We know the risks of exposure to much larger quantities, but it might not be possible to extrapolate downward to near-trivial amounts. Also, the radiation absorbed from an "afternoon at the beach" is different in overall spectrum to that from a dental X-ray. Is it really directly comparable?
In the United Kingdom, the lead apron has not been recommended for many years. In fact, one British doctor stated that lead aprons actually cause more exposure, because the scatter radiation can become trapped under the shield and be absorbed into the abdomen.
One of the most interesting comments came from another British doctor: "I am going to quote from paragraph 102 of Guidelines on Radiological Standards for Primary Dental Care, published by the National Radiological Protection Board in 1994. 'There is no mandatory requirement for the routine use of lead aprons for patients in dental radiography. Lead aprons do not protect against radiation scattered internally within the body, and only provide a practicable degree of protection in the case of the infrequently used vertex occlusal projection. Even in the latter case, the use of a lead apron could only be regarded as prudent for a female patient who is, or may be pregnant.'
"In other words unless you are taking a vertex occlusal film in a pregnant patient you don't use one, even if using processed film. Just think for a moment. The beam these days is collimated. How can radiation get to the abdomen? I have a lead apron and I only use it on those rare occasions when it is worn by a carer who is supporting a patient's head.
"So my advice is don't bother. I hate lead aprons. They are heavy and a nuisance. On the other hand if any of you are sued, I am willing to come as an expert witness. I should enjoy the expenses-paid trip!"
My next step was to contact Dr. Dale Miles, a professional speaker and radiology professor at the University of Kentucky School of Dentistry. I consider him the American guru of radiology. Here are his comments about the issue of shielding:
"There is no real consensus (on shielding), but I still feel it advisable for all patients to have a leaded apron for all X-ray procedures, and children should additionally have a thyroid collar for all intraoral X-ray procedures. On all patients, the thyroid collar can interfere with the beam and is probably not necessary.
"As always the judicious selection/prescription of all necessary X-rays is the best way to reduce/minimize patient X-ray dose. This is called 'Selection Criteria' and guidelines should be followed in all North American dental offices. The dentist must see the patient prior to ordering any films of any type to determine if the benefit outweighs the risk. There are many reasons for ordering radiographs, but the need must be determined first. Gone are the days when the dentist can say, 'Just take a full-mouth or bitewings before I see the patient in the chair.' That's just asking for trouble, and totally indefensible in a court of law. And, yes, for safety and for patient reassurance, offices should use all of the ways possible to reduce patient X-ray exposure, even with digital."
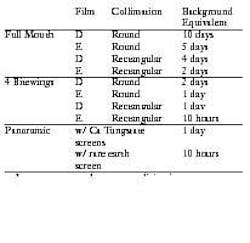
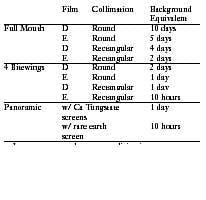
The text used by many dental schools, Oral Radiology Principles and Interpretation, (3rd edition by Goaz & White), states equivalent background exposure from dental radiography. I found it interesting that rectangular collimators allow significantly less radiation exposure than round collimators.
It went on to say that a person living in an average area of the United States who had one full-mouth and one panoramic film with optimized technique every year would incur 1/6th the risk of a person living in Denver with no exposure to dental radiography.
Whew! As you can see, there are many differing opinions, even downright confusion, about the value of shielding.
From an idea posted on the Internet Dental Forum, here's an experiment I conducted. I taped a penny to an unexposed film and placed it under the lead apron. I also placed a second film with a penny taped to it on the top of the shield. After exposing two films on my patient, I developed both the test films. Guess what I found out? There wasn't an image of a penny on either one! So my conclusion is that there was no detectable radiation anywhere but at the site on the face where the beam was directed.
This investigation took me a long way from your original question. Sometimes, the more you dig, the more you find. The consensus is that shielding may cause the patient to fear X-rays. However, since radiation dosage is accumulative over a lifetime, we should continue to use shielding until we have more substantial proof that there is no benefit. Further, as technology increases, I anticipate that shielding will be proven totally unnecessary due to safer and better techniques.
However, my advice to you would be to drop the whole issue and move on. I think it would be counter-productive to attempt to reconcile this patient. In this case, sending the patient a letter of apology only serves to confirm in the mind of the patient that your omission was "serious" — serious enough to warrant a letter. We who are educated in radiation hygiene know that this error was extremely minor. The bottom line is that this patient's expectations were not met, and she was vociferous enough to let the doctor know about it. I submit that most patients wouldn't even give it a second thought.
It is time to stop beating yourself up over this incident. Since it is impossible to please everyone, continue to do your best everyday with every patient. And when you commit an occasional "oops," just remember you are human just like all the rest of us on the planet.
Dianne
Dianne D. Glasscoe, RDH, BS, is a professional speaker, writer, and consultant to dental practices across the United States. She is CEO of Professional Dental Management, based in Lexington, N.C. To contact Glasscoe for speaking or consulting, call (336) 472-3515, fax (336) 472-5567, or email [email protected]. Visit her Web site at www.profession aldentalmgmt.com.