Despite diligent staff, infective endocarditis surfaces during periodontal treatment
Cynthia R. Biron, RDH
When we take thorough medical histories and treat patients several times with no post-operative complications, we feel quite certain that infective endocarditis is the least of our concerns. The following case actually occurred in a periodontal office where the patient was treated by a very experienced dental hygienist.
The dental hygienist practiced in the periodontal office every summer while on break from her full-time position as an instructor at a dental hygiene school. The office staff teased Mrs. Thorough (all names in this article have been changed to provide confidentiality) for her extreme methods of assuring that patient medical histories were complete and accurate. If you remember the seemingly overkill of instructors in patient assessment, you still sigh in exasperation. What happened to Mrs. Thorough`s patient is so surprising that everyone in the office was astounded.
When all goes well...
Jane, a 38-year-old female patient, presented with moderate periodontitis at Dr. Healey`s office during a periodontal examination and consultation. The hygienist, Mary Thorough, reviewed Jane`s unremarkable medical history. Mary further questioned Jane with pointed questions.
"Are you sure you have never had any heart problems and that no doctor has ever said you had a heart murmur?" Jane answered, " I`m sure."
"Have you taken any medications at all in the past two years?" Jane answered, "Tylenol and Trimox, three times in the last year for a periodontal abscess on this tooth (pointing to #14)."
"Are you sure you haven`t had any illnesses, surgeries, or medical problems in the last two years?" Jane answered, "I`m sure."
Afterwards, Mary took Jane`s vital signs and documented them as: "B.P. 110/70, Pulse 72, regular + bounding; Respirations 18; Temp. 98.4; Weight Patient slightly overweight - approximately 20 lbs."
Mary completed her patient assessment, and Dr. Healey examined Jane`s mouth. Jane was provided with a treatment plan that included presurgical scalings by quadrants on four separate appointments, followed by full flap surgery, and a free-gingival graft. The maxillary and mandibular right quadrants were thoroughly scaled and debrided on two separate occasions, two weeks apart. There were no adverse reactions after either scaling procedures.
Two weeks later, Jane returned for the scaling of the maxillary left quadrant. Mary completed the procedure without any problems and complimented Jane on the improvement in her oral hygiene. Mary showed her the improvements in the gingiva on the two right quadrants, which had been previously scaled.
At about 8 p.m. that night, Jane began having chest pains and palpitations of the heart, and she had a fever of 102 degrees. She was rushed to the hospital where the emergency room doctor, Dr. Fine, began questioning her on what she had done that day.
"Nothing strenuous," Jane replied, "I went to the periodontist and had these upper teeth scaled, but it was no problem."
Immediately, Dr. Fine explained the possibility of infective endocarditis and the need for tests and IV antibiotic. Laboratory tests for active infection were positive, leukocytosis, elevated sed. rate, positive C-reactive protein, and elevated serum immunoglobulins confirmed Dr. Fines`s suspicions. Samples of venous blood were taken for blood cultures but waiting for the results before beginning IV antibiotic was too risky, Dr. Fine thought. Dr. Fine asked Jane if she had ever had penicillin and if so, did she ever experience a rash or any allergic reaction of any kind from it.
Jane replied, "No. In fact, I have taken Trimox for a periodontal abscess three times in the last year, and I never had any reactions. Each time it cured the abscess."
Having that information, Dr. Fine immediately began IV administration of Penicillin G, 4 million units. He ordered a repeat of the regimen every six hours for two weeks, as well as administration of Gentamicin 1 mg/kg, IV every 12 hours. Echocardiography showed mitral valvular vegetations and a mitral valve prolapse with regurgitation.
The next day, Dr. Fine called Dr. Healey and informed him that Jane was hospitalized with infective endocarditis. Dr. Fine further explained that Jane had a prolapsed mitral valve with regurgitation that had never been diagnosed. He felt the infection was the result of a transient bacteremia from an invasive dental procedure. Dr. Fine also indicated that the symptoms of endocarditis may only have occurred on the day of the third appointment by coincidence and that it could have resulted from a transient bacteremia during the second scaling appointment two weeks ago.
Needless to say, Dr. Healey, Mary Thorough, and the entire office staff were shocked and dumbfounded. How could this happen when Mary was an extremist when it came to the risk management of patients who were, in any way, medically compromised. In actuality, the probability of this happening is extremely remote.
But the case places emphasis on several issues which confirm the improbability of this type of case:
- Hard to detect - Mitral valve prolapse, even with regurgitation, can be seemingly asymptomatic and not discovered unless there is reason to evaluate a patient`s heart with echocardiography. A doctor would not hear an associated murmur unless there was an alteration in heart function.
A patient with an undiagnosed mitral valve prolapse may receive invasive dental treatment annually for years and have transient bacteremias from the procedure and/or self-inflicted bacteremias (toothpicking, tooth brushing, etc.) and never experience infective endocarditis.
- Rare occurrences - Hospital admissions reveal that only three out of every 1,000 patients are admitted for treatment of infective endocarditis. Statistically speaking, less than 1 percent of the population will ever contract infective endocarditis.
Is it because a major portion of the population never receives dental treatment? No! Less than one in five patients with subacute bacterial endocarditis (SBE) contracted the disease from dental or medical invasive procedures. Between 17 to 51 percent of patients in a random study had oral transient bacteremias from chewing alone. Some smaller studies (24 to 300 patients) have shown as many as 15 to 20 percent of cases of infective endocarditis occurred within 12 weeks of dental treatment. Could this be mere coincidence with self-inflicted transient bacteremias that occurred from improvement in interdental cleaning after seeing their dental hygienist?
More research needs to be conducted to provide conclusive information. As many as 5 to 10 percent of the whole population is at high risk for endocarditis as they have acquired or congenital cardiac defects, prosthetic valves, etc. But studies also clearly show that, even when many high-risk individuals have had transient bacteremias, they still did not contract endocarditis.
There are other factors that medical science has still not uncovered about why some high-risk individuals do contract endocarditis and many do not. The answers probably lie in the complexities of man`s immune system.
- Role of interdental aids - Jane had been using a Perio-Aid and sometimes Stimudents, flossing faithfully from the first appointment at Dr. Healey`s office. Mary gave her the interdental cleaning aids and instructed her on how to use them.
Wooden cleaning devices used in a study caused transient bacteremias in 20 to 40 percent of patients tested. Not having knowledge of Jane`s MVP, Mary certainly couldn`t be faulted for providing such instruction.
But Jane, too, could have caused a self-inflicted transient bacteremia with her new found regime of interdental cleaning and papillary stimulation. Knowing this, it would be unwise to instruct high-risk patients (cardiac defects, prosthetics) to begin using interdental aids, especially when active periodontal disease becomes evident by bleeding on probing.
What is the right response?
What should our reaction be to Jane`s case? Start using prophylactic antibiotic more frequently? By all means, no! Anaphylactic reactions to penicillin result in as many as 800 deaths per year in our country alone. And, even as you read this, resistant strains of bacteria are being produced by the overuse and misuse of bactericidal antibiotics such as amoxicillin.
All dental professionals who have practiced many years have seen at least one highly improbable case of something and it occurred regardless of even the strictest protocols. The best reaction is to continue to follow American Heart Association guidelines and maintain malpractice insurance coverage at all times.
Just when you think you know all the disease entities which require prophylactic antibiotic, somebody, or some journal article, informs you about another one that is not on the common list. Most cases that require prophylactic antibiotic are for prevention of infective endocarditis. Other cases, however, require it to prevent an infection from getting out of control that requires hospitalization, prompts even septicemia and death, or an infection of a prosthesis.
Prosthetic hips, joints, heart valves, in-dwelling shunts, stints, and prosthetic vessels are findings that will readily be described to you by your patients. Any disease process that causes a patient to be immunocompromised (or drug therapy involving corticosteroids, anticancer therapy, or organ-transplant antirejection drugs) justifies providing patients with prophylactic antibiotic coverage during and after dental procedures.
For an updated list of reasons for prophylactic antibiotic, refer to the reference book, "Risk Management of the Medically Compromised Patient," by Little & Falace.
Antibiotic treatment
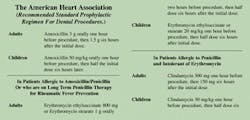
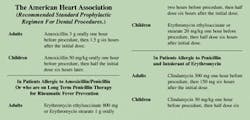
A clip chart of the American Heart Association`s (AHA) regimen for prevention of endocarditis is provided for you. Other important information needs to be emphasized. The AHA regimen is based on treatment of Alpha-hemolytic streptococci and may not be effective against other causative agents.
A decrease in cases of endocarditis caused by streptococci has been reported, even though it is the most common causative agent (80 percent). There has been an increase in endocarditis caused by gram-negative bacilli, staphylococci, and fungi. About 30 percent of IV drug abusers, even those without cardiac defects, contract endocarditis after two years of drug abuse. The causative agent of their infection is Staphylococcus aureus due to contaminated needles.
Other species of bacteria that may cause endocarditis are not affected by Amoxicillin. Consequently, even though patients have been compliant with the AHA regimen, they still can get endocarditis.
In many cases, the patient has not been given the current AHA regimen. Or there is a misinterpretation of the regimen. The confusion is usually over when to take the dose after treatment. It is not six hours after the dental procedure is completed. It is six hours after the initial dose. Please post the clip chart on your office bulletin board.
To prevent resistant strains from developing, it is very important to do as much dental treatment under one regimen of the antibiotic as possible. Appointments should never be closer than one week apart as frequent exposure to the antibiotic within a short time frame is likely to produce resistant strains of the bacteria and could result in a case of endocarditis in the future.
Such patients should be treated by experienced dental hygienists who can complete a significant amount of scaling (at least 2 quadrants) in one appointment. It should be contraindicated for dental hygiene students to take four to six appointments to complete a prophylactically premedicated patient that an experienced RDH could complete in one to two appointments.
We need to find a way to explain, in a simple manner, how resistant strains are produced. Patients don`t want to hear complicated gibberish about mutant strains. One simple line could be, "If you take an antibiotic too often or not long enough to kill a whole family of bacteria, all you do is vaccinate the bacteria against the antibiotic. Then the antibiotic doesn`t work anymore."
The objective of the explanation is to get patients to finish all of the antibiotics, even after symptoms have subsided. Although the prescription reads, "Take all of the medication," patients frequently forget to take it when the discomfort of their infection no longer reminds them. And, if a superinfection such as a vaginal yeast infection occurs, patients discontinue the medication without consulting their physician, or replacing the antibiotic for the original infection.
The AHA regimen is not the proper regimen or antibiotic for preventing other infections such as those involving prostheses in other areas of the body and other disease processes that render patients immunocompromised. Always consult the patient`s physician for the proper antibiotic regimen for the patient`s condition.
Endocarditis can affect patients with no risk factors. It is important to know the signs and symptoms of the infection. Some patients, like Jane, may not have all of the signs and symptoms.
In SBE, the initial symptoms may be so mild that they go unnoticed. Within two weeks, the manifestations usually are quite pronounced. Flu-like symptoms dramatized by chest pain, abdominal pain, and heart palpitations alarm the patient enough to get them to the hospital. Petechiae of skin and mucosal tissues may appear, while a pale complexion occurs due to anemia. In more advanced stages other blue to purplish lesions of the skin appear, along with cardiac complications and splenohepatomegally.
Dental precautions
Before any invasive dental procedure, have patients rinse thoroughly with an antimicrobial rinse. Some currently recommended rinses include clorhexidine, Listerine, and a 1 percent povodine-iodine solution. Sulcular irrigation with any of those rinses after the procedure is also recommended.
Studies have not substantiated the effectivenes of pre-rinses and sulcular irrigation, but there are no disadvantages to their use. It is conceivable that they may make a difference in reducing numbers of bacteria and prevent transient bacteremias.
Have you seen a patient who presented with a rare medical situation or an adverse reaction to dental treatment? Do two things:
- Tell us about it so we may share to spare others.
- Get malpractice insurance coverage.
Cynthia R. Biron, RDH, is director of the dental health programs at Tallahassee Community College. She is also a certified emergency medical technician.
Interesting case?
The Medical Alert column contains actual cases which involved a need for a medical consultation, management of a medical emergency, or a post-op complication. If you know of an interesting and informative case for your readers, please send a brief description of the case to:
Cynthia R. Biron, director, dental health programs, 1964 Gina Drive, Tallahassee, FL 32303.
Ms. Biron will contact you for a personal telephone interview. All cases will remain strictly confidential unless a dental team is in agreement with being given recognition for a livesaving medical situation.