Pain control in dental hygiene
by Margaret J. Fehrenbach, RDH, MS
Pain control should be an integral part of nonsurgical periodontal therapies. This is true whether the dental hygienist can directly administer local anesthesia or the supervising dentist performs this procedure. This article will explore the pain control option of local anesthesia and how it can be used with the “Velvet Touch” technique during dental hygiene treatment (see table 1).
Local anesthesia should be a standard procedure performed before nonsurgical periodontal therapies. It is important that the clinician let the patient know of the standard at the initial examination appointment as well as when scheduling future appointments. The objective is to discuss the procedure before the actual administration of local anesthesia. This allows the patient to say at an early juncture that they do not want local anesthesia, at which point the clinician should explore the patient’s concerns. The clinician can inform the patient that most patients need it for comfort and to allow for the best treatment. Keep in mind that the short amount of time for local anesthesia allows much more time for the actual treatment on a patient.
State laws at this time still vary as to what pain control procedures can be performed by the dental hygienist. However, all states require education and possibly certification if local anesthesia is allowed by the state’s practice acts. If there are any questions about a specific state’s practice acts, one can check with the state’s dental board. The states of Arizona, California, Oklahoma, Oregon, and Washington have allowed dental hygienists to administer local anesthetics for more than 25 years. Many other states have followed suit and now allow this important procedure to be performed by dental hygienists.
Dental hygienists who have completed required continuing education course work in local anesthesia administration have provided safe, effective injections. They have reported this service to be of value to the practice, and have had very few complications.1
The Velvet Touch concept
Certain procedural methods should be incorporated by the clinician when injecting local anesthetics to achieve the Velvet Touch (a concept promoted by the author) (see figure 1). Basically, this method uses both vocal sedation and the therapeutic touch that an experienced, quality clinician would use during dental treatment, but also places emphasis on how the injection is given.2 Patients tend to relax and even smile slightly as the clinician relates that he or she will be using the “Velvet Touch” when giving them pain control, since by those very words - similar to the phrase “summer afternoon” - relaxation becomes the mode of thought.3
With the Velvet Touch, the syringe and its separate tray are kept out of sight of the patient, and other patient-centered considerations are practiced. The tray for the local anesthetic procedure is placed behind the patient, separate from the front-delivery periodontal instrument tray. In addition, patients should, in most cases, close their eyes during the injection. There is no need to show patients the needle; however, if they insist on seeing it, the clinician should show the syringe with the cap on. The clinician should assemble the syringe out of the patient’s view to reduce unnecessary patient apprehension. Passing the syringe in and out of the oral cavity should also be accomplished outside the view of the patient.
The patient is supine during the injection procedure, with the clinician seated, to promote comfort.4 This also avoids problems with patient syncope, which is the most common dental emergency and most common side effect of local anesthesia. Finally, having the patient supine helps the clinician easily view the landmarks necessary for safe and effective injections.
The tissue in the area of the injection is gently dried before the needle enters to reduce contamination from the oral cavity into deeper tissues. There should also be consideration for the use of an antimicrobial preprocedural oral rinse to sanitize the oral cavity as recommended by the latest Centers for Disease Control Guidelines for Infection Control in Dental Health-Care Settings (2003).5 Antimicrobial oral rinses (for example, chlorhexidine gluconate, essential oils, or povidone-iodine) used by patients before a dental procedure are intended “to reduce the number of microorganisms the patient might release in the form of aerosols or spatter that subsequently can contaminate dental health-care personnel and equipment operatory surfaces.” In addition, “preprocedural rinsing can decrease the number of microorganisms introduced in the patient’s bloodstream during invasive dental procedures such as nonsurgical periodontal therapies.” It is important to never inject in areas in the oral cavity with infection so as to prevent the spread of infection to deeper tissues (by way of needletrack infections).6
When using injected local anesthetics, topical anesthetic is placed for at least one minute, preferably for two to three minutes (as per the package insert for all presently marketed topical anesthetics), on the soft tissue to increase comfort.7 Topical anesthetics actually do penetrate mucous membranes of the oral cavity two to three millimeters below the surface to reach free nerve endings. Achieving comfort during the puncture of the tissue by the needle is especially important for maxillary facial injections. The clinician should inform the patient: “I am using this surface anesthetic to make the rest of the procedure more comfortable for you.” The injection will need to be performed within one to two minutes after removal of the topical anesthetic for maximum effectiveness.8
The clinician should not use an excessive amount of topical anesthetic which may cause an increased risk of toxicity and an increase of uncomfortable soft tissue anesthesia (see figure 2).9 In order to control these side effects, in preparation of tray set-up, the clinician should place a small amount of topical anesthetic in the inner rim from the bottom of the bottle. Roll the cotton tip applicator in the inner rim of the mouth of the bottle to imbed topical (see figure 3). Then place the cotton tip applicator with the topical anesthetic lightly on the tissue and only on the area of puncture; surface anesthesia is by contact and not by pressure! Topical anesthetic sprays can make it difficult to control the amount of anesthetic and location of application and, thus, are not usually recommended for prepuncture soft tissue anesthesia in the oral cavity.
Additionally, to promote the Velvet Touch, pressure anesthesia is used after the placement of topical anesthetics with palatal injections to help in this location with its unusual histology.10 Because the overlying palatal tissues are very dense and adhere firmly to the underlying palatal bone, the use of pressure anesthesia to the injection site before and during the injection to blanch the tissues will reduce patient discomfort by producing a dull ache to block pain impulses arising from needle penetration (see figures 4 A and B).11 Mirror handles are not recommended for pressure anesthesia; instead cotton tip applicators are used due to their gentle and round structure.
To further facilitate the Velvet Touch, during the injection of the facial alveolar mucosa, the soft tissue should be kept taut by strong and steady retraction with two fingers and not a mirror (see figure 5). This will allow the needle to easily and comfortably penetrate the tissue, and the tissue will not have a chance to possibly reflect over the needle tip at the last minute. The index finger is used on the dominant side intraorally and the thumb extraorally. On the nondominant side, the thumb is used intraorally and the index finger extraorally. With this level of retraction, a safe zone of 10 to 15 millimeters is created around the needle tip to prevent needlestick injuries. In cases where slippage of tissue is anticipated, a small gauze square is effectively used to help retract the tissue during the injection (see figure 6). This occurs mainly when administering the anterior superior alveolar nerve block or any maxillary anterior infiltration as the clinician retracts the upper lip. It is important, though, to not allow the gauze to interfere with the injection. Using the same two-finger retraction with the inferior alveolar, incisive, and buccal (long) blocks is also helpful in maintaining control during the injection.
Administration techniques
The bevel of the needle is always placed toward the bone, deep within the tissue.12 To easily check the bevel position, the drip of the solution is noted off the bevel surface of the needle. If the bevel is not toward bone and bone is touched, there may be tearing of the periosteum covering the bone and resultant discomfort.
Newer needles are available having a colored graphic on the hub of the needle located on the same side as the bevel that can easily help the clinician with the determination of the bevel position (see figure 7). This is especially helpful when performing the inferior alveolar block due to its deep tissue penetration (average depth of the needle is 25 millimeters).
The clinician should not move the needle horizontally deep within the tissue, because it can tear the tissue and also can cause needle deflection. With deflection, the clinician does not know the exact position of the needle tip or bevel hidden in the tissue. If the position of the needle is not correct with initial placement, the needle should be removed from the tissue completely or most of the way by the clinician before re-entering the tissue. The discomfort may not be felt at the time of the injection, but the area will feel sore to the patient later due to tissue tears.
The author has noted an increase in the occurrence of movement of the needle in the tissues by some clinicians when she has viewed the administration of the posterior superior alveolar nerve block. The uncontrolled movement of the needle in this case can lead to the complication of an extraoral hematoma if the maxillary artery or pterygoid plexus of veins is inadvertently punctured. In addition, bending the needle is also to be avoided with this maxillary block for the same reason. At other times, the author has noted horizontal needle movement when viewing clinicians administering the inferior alveolar nerve block, which is problematic due to its deep tissue penetration as noted earlier.
Extra needle deflection can also be avoided by the use of a proper gauge for the needle depending on the injection given. The use of a smaller gauge needle for patient comfort is unwarranted since studies show that patients cannot feel the difference between needle 13 A 25-gauge long needle (inferior alveolar block and long buccal block by default) and a 27-gauge short needle (all other injections) are recommended due to their ability to decrease deflection, provide accuracy, and allow for safety when aspirating.14,15 Studies using human tissue and radiography have demonstrated that a 30-gauge needle inserted to a depth of 25 millimeters deflects four millimeters, a 27-gauge needle deflects two millimeters, and a 25-gauge needle deflects one millimeter.16
This use of a larger gauge of needle is especially important for the inferior alveolar block injection with its considerable depth of penetration when accuracy and aspiration ability are key to success. With this injection, the needle tip must be within one millimeter of the landmark of the mandibular foramen for accurate deposition. This block also has the highest risk for positive aspiration.
The differences in deflection between needles with varying needle gauges as the needle enters tissue can be noted using glycerin soap (see figures 8 A and B). The differences with aspiration between the different needle gauges can also be noted using colored water in a cup. Aspiration is important; if the local anesthetic agent is deposited into a blood vessel, no anesthesia is obtained and serious complications can occur.
The main factor for pain control during an injection, though, is the slow dispensing of the local anesthetic agents. Each full cartridge should be dispensed over one minute. The needle entering the tissue is not the major cause of discomfort, contrary to popular thought; it is rather the pressure and the volume of the fluids being injected into the tissues that causes the most distress to the patient. Even when the patient has received an initial dose of agent, he or she may not immediately feel the pressure of the added agent if given too quickly, but will later feel tissue soreness. The clinician should use this time dispensing to talk softly, assuring the patient of comfortable treatment. The clinician can communicate with the patient: “I am depositing solution slowly so it will be more comfortable, but you are not receiving any more than usual.”
The clinician may want to check the usual rate of deposition of the agent outside the patient sphere by using a cup. First, the clinician can observe to make sure that the rate does not produce a stream but a constant drip when dispensing the agent; later the clinician should cover the tip and just watch the rubber stopper move at a constant rate and have a partner check the actual rate of deposition of the agent, thus simulating the actual situation where the agent enters blindly into the tissue of the patient (see figure 9).
The newer computer-controlled anesthetic devices automatically incorporate this pain reduction strategy since they deliver the local anesthetic agent more slowly than any clinician can. Data from clinical studies indicate that patients generally find the computer-controlled local anesthetic injections to be less painful than those delivered by traditional syringe, even in the palatal area.17,18,19 In addition, the newly discovered block, the anterior middle superior alveolar (AMSA) block, is only accomplished with these newer technological advances.20
Current concepts in local anesthesia are reviewed.
Key to the Velvet Touch technique is that the injection is given in the correct manner.21,22 One common reason for anesthetic failure is due to an inaccurate injection; the local anesthetic is not delivered near enough to the relevant nerve or bony area and thus it is either totally ineffective or only partial anesthesia is attained. Injection into muscle and not close to bone will usually prevent the local anesthetic from working and may lead to excessive muscle soreness afterwards.
Another common reason for anesthetic failure is that too little local anesthetic agent is used. The patient may have large teeth with unusually long roots or the bone surrounding the roots may be excessively thick.
The final common reason for anesthetic failure in patients is that treatment is started before the local anesthetic can take effect; usually three to five minutes is required for most local anesthetic agents to take effect in average situations. This time period allows the nerve to be fully bathed in the local anesthetic agent.
This particular problem is especially noted with injections for the procedures involving the mandibular arch due to its density and anatomical variations. Placing the patient in an upright position for 20 seconds after the injection series has been shown to promote deeper anesthesia in most mandibular arch cases.23 It is important to note that all these common reasons for failure just discussed are based on anatomical considerations. Management of pain through local anesthesia requires a thorough knowledge of the anatomy of the skull, trigeminal nerve, and related tissues, and how those are presented in each individual patient. A review of a textbook on local anesthetics by the clinician may be considered or a continuing education course in the subject may be necessary to reinforce the needed basic anatomical information.24
Vasoconstrictor discussion
Dental hygiene procedures usually involve varying levels of bleeding during instrumentation without utilization of local anesthesia with vasoconstrictor, hampering effective treatment by the clinician. This is especially true in the areas of periodontal furcations or deep periodontal pockets. Obtaining hemorrhage control using vasoconstrictor with the local anesthetic agent is one of the key ways to increase the effectiveness of basic local anesthetic procedures, which again can facilitate the Velvet Touch. Additionally, the vasoconstrictor makes the injection safer: there is slower absorption into general circulation and over a longer period of time, so there is a lower chance of overdose from the local anesthetic agent. As an added bonus, the patient experiences a longer duration of anesthesia, possibly until a postoperative analgesic can take effect after instrumentation.
Most contraindications to the use of vasoconstrictor during elective dental procedures are relative and not absolute. An absolute contraindication indicates that under no circumstance should this drug be administered to this patient because the possibility of potentially toxic or lethal reactions is increased. With a relative contraindication, the drug in question may be administered to the patient after carefully weighing the risk of using the drug against its potential benefit, and if an alternative drug is not available. Most of these relative contraindications due to medical history complications recommend a reduction of the vasoconstrictor but not a complete lack of it (see table 2 for some common situations in the dental office).
This overall reduction of vasoconstrictor can be accomplished by the use of more than one type of local anesthetic agent, giving a series of injections (“cocktail approach”).25 Half of the amount of agent with vasoconstrictor is administered initially in the specific areas according to the patient’s needs and staying within the maximum recommended dosage. Then later, the other half of the amount needed is administered in the same region using a plain agent. Thus, the overall amount of agent is not reduced; the patient responds with an adequate depth and length of anesthesia, and hemorrhage control is assured, while using less vasoconstrictor.
All types of agents can be used together without any anticipated problems. A series of injections with different agents to reduce vasoconstrictor level has been used for many years in dentistry with success. However, there is no formula for the correct degree of reduction and it is important to use the smallest dose of vasoconstrictor that still will allow dental treatment.26 Another method to reduce the amount of the vasoconstrictor would be to reduce the procedures to be accomplished during the appointment (sextant instead of quadrant, quadrant instead of half-mouth).
The American Dental Association (ADA) recommends the use of a reduced amount of vasoconstrictor in controlled cases of cardiovascular disease (CVD) to allow these patients much needed profound anesthesia.27 This use of smaller amounts of vasoconstrictor with the agent also minimizes the risk of direct vascular injection, which could be dangerous in these patients.
Regional block vs. infiltration method
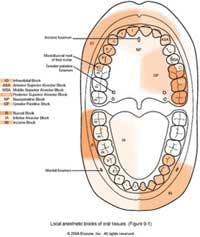
It is recommended that pain control in dentistry be performed using regional block anesthesia instead of infiltration methods. Stanley F. Malamed, DDS, professor of anesthesia and medicine at the University of Southern California in Los Angeles, states, “Fewer penetrations of mucous membrane and smaller volume of local anesthesia is administered (with regional blocks) to provide adequate anesthesia.”28
This use of regional block anesthesia works well with the standard dental hygiene protocol of performing quadrant or half-mouth procedures during nonsurgical periodontal therapy (see figure 10).29 There is a move to the use of sextants for nonsurgical periodontal therapy, especially in medically compromised cases, to improve quality of procedures performed, reduce systemic complications in the patients, and increase local healing. In most cases, it is important to perform regional block anesthesia on the mandibular arch, since infiltration is not as effective in the mandibular arch due to the increased density of the bone, especially in the posterior region of the arch.30
Assurance of pulpal anesthesia for nonsurgical periodontal therapy is important, and it is more easily obtained for a longer length of time with regional block anesthesia, in addition to soft tissue anesthesia. Pulpal anesthesia allows more comfortable instrumentation on possibly sensitive dentin-covered root surfaces.
The clinician should inform the patient that more anesthetic is available if needed, and always add more local anesthetic agent as needed, if requested. However, the clinician should always keep below the recommended maximum dosage for that individual patient.
Patients need an additional amount over the suggested amounts in local anesthesia textbooks if they have extreme root length and density of bone or increased levels of inflammation that promotes acidity in the tissues. The clinician should let the patient know that when agent is added, it is usually not even felt if given properly, since the surface tissues still have a significant amount of anesthesia.
Aligning with dental hygiene procedures
When using regional block anesthesia, it is important to inject from posterior to anterior based on increased levels of sensitivity of the tissues as one moves from posterior to anterior in the oral cavity.31 The clinician should then perform most instrumentation from the posterior to the anterior of the oral cavity after the injection series.
The clinician should consider periodontal probing of each quadrant with anesthesia after the regions are instrumented. Probing patients during an initial examination with inflammation and without anesthesia can be very uncomfortable to the patient, and associated bleeding and deposits may reduce accuracy.32 Both the ADA and the American Academy of Periodontology recommend that the Periodontal Screening and Recording (PSR) System® be used during the initial examination to screen for periodontal disease instead of a full-mouth periodontal probing.33,34 This system takes only a few minutes and tells the clinician immediately the level of periodontal involvement and treatment options needed by the patient. The PSR also summarizes necessary information with minimum documentation for submission to third party payers. However, the PSR is not intended to replace a comprehensive periodontal examination when indicated.
If the clinician is individualizing the use of local anesthetic agents, as should be the case, each tray will have to be prepared after the patient is seated; the universal use of one type of local anesthetic agent is not in the best interest of the patient since medical and dental histories can vary per patient. It is important that the dental practice keep supplies for local anesthesia nearby where it is used and not in another treatment room or lowest drawer, so that the clinician does not have to get up to assemble the local anesthetic tray.
As an example of individualizing the approach to the use of local anesthetic agents, only a few of the agents are more highly recommended for pregnant patients than others (see table 2).
Click here to view Table 2.
Most local anesthetics have not been shown to be teratogenic in humans and are considered relatively safe for use during pregnancy.35 The recommendation for caution (Category C) relates primarily to limited data collected in animal studies. Other agents are not at full caution; instead adverse drug effects to humans cannot be ruled out for all these agents (Category B). Because all local anesthetics can cross the placenta and cause fetal depression, limiting the dose to the minimum required for effective pain control is obviously advisable. Epinephrine, a naturally occurring hormone, is generally considered to have no teratogenic effects when administered with dental anesthetics. There are also a few drug interactions to keep in mind when using local anesthetics and vasoconstrictors (table 2). A review of a textbook on local anesthetics by the clinician may be considered or a continuing education course in the subject may be necessary to have the updated information when considering the use of various agents. No local anesthetic agent should be given to a pregnant patient without the consideration of her physician’s desires and her wishes.
Care with armamentarium
The clinician should make sure to change the needle after three to four injections or when the patient is sensitive, so that they are always sharp and can easily enter the tissue. Dental practices should be wary of low cost or old local anesthesia supplies. Hard rubber stoppers in the cartridges that do not easily allow engagement by the harpoon - forcing the clinician to slam them on a countertop to engage the needle - do not promote a very friendly way to introduce the patient to a gentle local anesthetic technique. Needles that are hard to open and remove from the syringes (one has to use a rheostat) may increase needlestick risk for the clinician. Harpoons on syringes that are bent, dull, or even rusty do not allow for effective use of local anesthesia. Traditional syringes do not have an unlimited lifetime and should regularly be checked with colored water in a cup to make sure they can aspirate (see figure 11).
The clinician needs to keep current in pain control. A new topical anesthetic for the oral cavity has been developed containing low levels of lidocaine, prilocaine, and a thermosetting agent. This new formulation is similar to the eutectic mixture of local anesthetics (EMLA) that is commonly used on the skin prior to needle puncture, since the present formulation is only recommended for dermatological use by the Food and Drug Administration.32,36 It appears that it can be used within the pocket and with or without injected local anesthetics, depending on the case type presented.
Pain control should be an integral part of dental hygiene nonsurgical periodontal therapies. Clinicians involved in these therapies should consider use of the Velvet Touch when utilizing local anesthesia during dental hygiene treatment. This is true whether the dental hygienist can directly administer local anesthesia or the supervising dentist performs this procedure.
Margaret J. Fehrenbach, RDH, MS, is an adjunct instructor at Marquette University in Milwaukee where she received her bachelor of science degree in dental hygiene. Fehrenbach also received her master of science in oral biology and certificate in clinical research methods from the University of Washington in Seattle, where she now lives. Margaret has extensive clinical experience, as well as a background as an educator, writer, and speaker on pain control with Julienne Strasser, RDH, BS, of Canyon Dental Seminars. Fehrenbach can be reached at [email protected] or visit her Web site, www.dhed.net.
Author’s note: The information provided is designed to support, not replace, the relationship that exists between a patient/reader and his/her existing physician/dentist.The information is provided “as-is” and without warranty, expressed or implied.
References1 Anderson JM. Use of local anesthesia by dental hygienists who completed a Minnesota CE course. Journal of Dental Hygiene. 2002 Winter;76(1):35-46.
2 Fehrenbach MJ. Stress Reduction for the Oral Health Care Patient at High Risk for Medical Emergency. Access (ADHA), July 2004.
3 James H. “Summer afternoon-summer afternoon; to me those have always been the two most beautiful words in the English language.”
4 Malamed SF. Handbook of Local Anesthesia, 5th ed. St. Louis: Mosby; 2004.
5 Centers for Disease Control, Guidelines for Infection Control in Dental Health-Care Settings. Available at: www.cdc.gov/mmwr/preview/mmwrhtml/rr5217a1.htm. Accessed April 5, 2004.
6 Fehrenbach MJ, Herring SW. Illustrated Head and Neck Anatomy, 2nd ed. Philadelphia: W.B. Saunders; 2002.
7 Nusstein JM, Beck M. Effectiveness of 20% benzocaine as a topical anesthetic for intraoral injections. Anesthesia Progress. 2003 ; 50(4): 159-63.
8 Feugate AD. Topical Anesthetics: An Important Pain Control Technique. Proctor and Gamble. Available after registration at: www.dentalcare.com/soap/pr_forum/dhygiene/top-anes.htm. Accessed April 5, 2004.
11 Sloss D. Pain control and the apprehensive patient. Dentistry Today. 2001 Jun;20(6):68-71.
12 Malamed SF. Handbook of Local Anesthesia, 5th ed. St. Louis: Mosby; 2004.
13 Mollen AJ, et al. Needles - 25-gauge versus 27-gauge - can patients really tell? General Dentistry 1981 29:417-418.
14 Cooley RL, Robison SF. Comparative evaluation of the 30-gauge dental needle. Oral Surgery, Oral Medicine, Oral Pathology. 1979 Nov;48(5):400-4.
15 Aldous JA. Needle deflection: a factor in the administration of local anesthetics.
Journal of the American Dental Association 1968 Sep;77(3):602-4.
16 Isen DA. Local Anaesthetic technique. Septodont. Available at: www.septodont.ca/Septodont/english/other/cea_di01.html. Accessed April 5, 2004.
Overview of the Velvet Touch* with local anesthesia
• Making local anesthesia a standard operating procedure
• Using vocal sedation and therapeutic touch
• Placing tray and syringe out of patient’s sight
• Putting patient supine and clinician seated
• Using a preprocedural oral rinse and drying tissue
• Placing topical anesthesia and keeping tissue taut
• Placing bevel of needle toward bone and using no horizontal movement
• Using the correct gauge of needle and slowly dispensing the agent
• Giving injection in correct manner: proper location, proper agent amount, and allowing time for agent to take effect
• Using a vasoconstrictor in correct amount in most cases
• Using regional blocks and assuring pulpal anesthesia
• Periodontal probing after instrumentation with local anesthesia
• Keeping supplies nearby and individualizing agent used
• Using local anesthesia supplies that support the procedure: changing needles for sharpness, checking for quality in needles, cartridges, and syringes
• Concept promoted by author that places emphasis on how the injection is given.