Trends In Dental Hygiene
Clinical Results And Profitability Of A Caries-Management Program In Private Practice
By Pamela M. Maragliano-Muniz, BSDH, DMD; Dona R. Roberts, RDH; and Robert J. Chapman, DMD
It is well established that dental caries is increasing in prevalence in the adult population.1 This the result of having one or more risk factors that predispose a patient to caries, which can be potentially debilitating, especially for the population of people who are at a high or extremely high risk for developing new caries.2 These patients tend to have frequent or severe caries and experience a negative perception of comfort, function, appearance, and perception of biologic health3,4,5 — factors that relate directly to a person’s quality of life.6
Related articles
Resin infiltration of incipient smooth surface lesions" is now covered by a 2013 CDT Code classification
Preoperative case assessment strategies to avoid clinical dental shortcomings in endodontic treatment
And you thought dental plaque was bad: preventing evolution of biofilms
In late 2007, the California Dental Association introduced specific strategies for the practice of CAMBRA (Caries Management by Risk Assessment)7 to assess the risk factors associated with each patient on an individual basis, assign them to a risk category, and treat them with risk reduction therapy and minimally invasive dentistry.8,9,10,11,12 Since 2008, our practice has used a modification of this approach13 to patient care, and we have experienced excellent patient compliance, a dramatic reduction in new carious lesions, increased new patient referrals, and enhanced productivity within the practice. This prompted a chart review of our patients. The purpose of this article is to discuss how CAMBRA was tailored for the private practice, the results of the chart review, and the impact that implementing a caries-management program has on clinical results and productivity within the dental hygiene department and new patient referrals in a private practice.
Methods and Materials
We completed a chart review of 132 patients who were offered the caries-management protocols in our private practice. The computer generated a list of all patients who were assigned to a risk category and were recommended to follow the protocols since early 2008. We randomly selected every third chart for our review. To preserve anonymity, we assigned a code to each patient record that corresponded to a code on the data sheet. The patient list and data sheets were kept in separate locations within the office. We collected and evaluated the following information from our chart review: Patient demographic (sex/age), number of newly diagnosed early carious surfaces (clinical or radiographic), severity and location of plaque, calculus, stain, sensitivity, presence/absence of gingival bleeding on probing, risk category, risk factors, acceptance of the recommended risk reduction therapy, completed risk reduction therapies provided in the office, charting, radiographs, and case notes. We measured the clinical changes and discussed the quality of life indicators at each recall over a two-year period (April 2008 to May 2010). Profitability and new patient referrals were recorded through 2011. We entered results into a database and evaluated trends within the dental practice. Small sample size and lack of standardization of the data will indicate trends within the dental practice and, therefore, statistical significance was not determined.
CAMBRA Tailored For Private Practice
We modified the CAMBRA protocols to minimize cost for the patient, increase efficiency for the dental practice, and maximize patient compliance. It is the experience of the authors that the dental hygienist is the ideal practitioner to initiate a caries-management program. The dental hygienist has regularly scheduled appointments to provide direct patient care and education. When given adequate time for recare appointments (45 to 60 minutes are recommended), the dental hygienist can provide risk assessment and risk management strategies for the patient. The dental hygienist can often monitor changes in the patient’s home-care practices and oral condition. In addition, the dental hygienist is usually one of the most trusted practitioners in a dental office, and patients are most commonly receptive to the recommendations of the dental hygienist.
Additional modifications included the following:
Elimination of the risk assessment questionnaire — Although a risk assessment questionnaire14 is very thorough, the dental hygienist can assess a patient’s caries risk during the recare appointment without the added time and paperwork of a risk assessment document. The dental hygienist routinely evaluates caries risk (see Table 1), including the patient’s medical history, medical conditions, and medications that have oral side effects, and assesses oral hygiene and the condition of the periodontium and dentition. In addition, the dental hygienist can discuss the role of the patient’s diet as it relates to dental caries.
Alternatives to salivary flow and bacterial testing — Although specific salivary flow tests are available and useful,14 it may be time-consuming and costly for the dental hygienist to utilize these tests on all patients. As an alternative, the dental hygienist can estimate the patient’s salivary flow without adding additional time and cost to the recare visit by remaining cognizant of the amount of time the saliva ejector is necessary during the recare visit. If the saliva ejector is necessary throughout the entire visit, it can be estimated that the patient has adequate salivary flow. Conversely, if the oral environment remains dry throughout the visit, the dental hygienist can estimate that, coupled with additional risk factors (e.g., medical conditions or medications that are linked to xerostomia), the patient may be suffering from xerostomia. In addition, the dental hygienist is the ideal practitioner to evaluate the condition of the saliva. Normal salivary flow has serous, mucus, and mixed components, and a water-like presentation clinically.15 Patients who have inadequate salivary flow may have saliva that appears foamy, stringy, or absent16,17 or may report other oral side effects, including a fissured tongue or burning sensation in the oral cavity.18
Bacterial testing is also available to test for the presence of Streptococcus mutans and Lactobacillus.19 Although these tests are useful, it may also be time-consuming for a dental hygienist to implement this type of testing on every patient. The dental hygienist is the ideal dental practitioner to evaluate the presence, location, and amount of plaque and calculus on the teeth. In addition, a disclosing agent (see Fig. 1) designed to detect acidogenic dental plaque (see Fig. 2)20 may be an efficient, cost-effective alternative.
Classification of risk category — Once risk has been evaluated, the dental hygienist can assign a patient into a caries risk category: low, moderate, high, or extreme-high.21 An alternative to calculating the number that corresponds to the list of protective vs. disease factors from a risk assessment questionnaire, as mentioned earlier, the dental hygienist can easily identify the risk factors through patient interaction and oral examination. If a patient presents with any high-risk factor (see Table 2), the patient is classified as high risk. If a patient has multiple high-risk factors or severe xerostomia, the patient can be assigned to extreme-risk. Conversely, a low-risk patient has the absence of disease or risk factors. A moderate-risk patient may have risk factors that are conducive to the development of dental caries, without establishing an immediate high risk.
Minimization of antimicrobial therapy — Antimicrobial therapy is currently used to minimize bacteria that cause dental caries.22 However, research has demonstrated that the consistent use of chlorhexidine rinses does not have a significant impact on caries risk.23,24 In addition, it is the experience of the authors that implementing a caries-management program that includes the monthly use of chlorhexidine rinses results in difficulty in patient compliance. The routine recommendation of chlorhexidine rinses for one week each month for all high-risk or extreme-high-risk patients was eliminated.
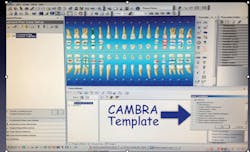
Documentation — It is essential for a dental hygienist to identify and document caries risk factors and risk management strategies. However, it would be nearly impossible to maintain standardized documentation if a dental office relied solely on improvised written text. Moreover, it would be expected that the documentation between different clinicians would differ greatly. This became clearly evident during the chart review that was conducted to evaluate the results of the caries-management program within the office. The use of a standardized chart document (for paper dental records) or templates (for electronic records) should be utilized to maintain a complete, concise, and standard entry for each dental hygiene recare visit.
Documentation should include the identification of the present risk factors, caries risk classification category in which the patient was assigned, risk management recommendations, and whether or not the patient was receptive to the recommendations (see Fig. 3).
Results
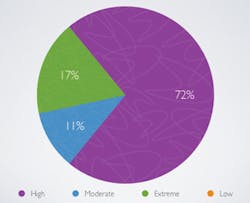
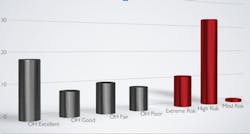
Clinical results — The chart review of 132 patients generated records from 62 men and 70 women, with a mean age of 63 years old. Fifty-two patients exhibited excellent, 28 good, 27 fair, and 13 poor oral hygiene. The caries risk category assignments include 21 extremely high, 87 high, 13 moderate, and 0 low risk (see Fig. 4). Forty-nine of these patients exhibited newly diagnosed early carious lesions. Two hundred fifty-four new carious surfaces were diagnosed either clinically (coronal smooth surface, occlusal, or root surface lesions) or radiographically (on a bitewing radiograph). Nearly 94% of the patients who presented with new carious lesions accepted the decay prevention protocols. Of these 254 carious surfaces, 215 were reversed clinically or abated radiographically. Additional encouraging results included a majority of patients with exposed root surfaces experienced a reduction of plaque, calculus, extrinsic stain, and dentinal hypersensitivity (nearly 62%), improvement of oral-health-related quality of life (nearly 70%), and changes to root surfaces.25
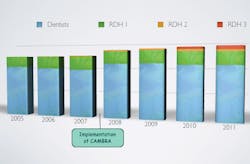
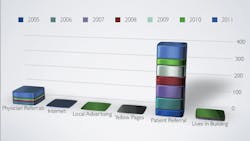
Profitability and new patient referrals — Since the addition of a formal caries-management program, office productivity increased significantly (see Fig. 5) as well as patient referrals (see Fig. 6).
Discussion
The trends that were generated from this record review indicate that the implementation of caries risk reduction therapies will improve clinical outcomes and oral-health-related quality of life. This dental practice has been established for 37 years, specializes in prosthodontics, and limits its practice to adult patients. Consequently, the results may not be generalizable to general or family dental practices. Moreover, this may contribute to a higher mean age of our patients and assignment to a higher risk category due to the presence of many risk factors. In addition, most of the patient records we studied were for patients of record prior to 2008; however, information was collected from April 2008 to May 2010 in an attempt to standardize and limit the clinical results to directly reflect the implementation of a caries-management program.
The positive outcomes of a caries-management program that are tailored to a private practice supports the significance of the dental hygienist’s role in the implementation and consistent execution of a caries-management program. It is suggested that the information extrapolated from assessment and risk management recommendations are documented in a uniform manner for the most favorable results. This can be accomplished by a standardized charting document in a written record or a template within an electronic record.
This record review describes the efficacy of managing and lowering the risk of our patient demographic. Caries management (either via reversal or stabilization) was exhibited in patients despite risk category or oral hygiene status (See Fig. 7). This encourages practitioners to consider utilizing the caries-management protocols for patients of all risk categories and oral hygiene status. It is suggested that assessment is performed at each dental hygiene recare visit, as the patient’s status may change between visits. Generally, a patient’s risk for caries will remain constant or escalate. A patient’s risk may diminish in the rare instance of the elimination of offending risk factors that were present at one time. Furthermore, risk management strategies should be reinforced at each recare visit.
This dental practice began implementing various marketing efforts, including a presence on the Internet and social networking approximately the same time as the caries-management program. Initially, it was not clear as to the source of what seemed like enhanced profitability and patient referrals. Evaluation of the origin of the referral of new patients reinforces that improving patient care is the most favorable marketing tool for a dental practice.
Conclusions
Although further and more detailed research is necessary to significantly substantiate the findings from this record review, the results indicate that the implementation of a caries management program will enhance patient care, profitability, and new patient referrals. The dental hygienist is the ideal individual in the dental practice to implement, execute, and manage a caries-management program. RDH
Acknowledgements
We appreciate Dr. William Maness and Lewis Wharf Dental Associates, Boston, Mass., for the permission to use information related to his patients and dental practice.
References
1. Centers for Disease Control and Prevention. Oral Health: Preventing Cavities, Gum Disease and Tooth Loss. www.cdc.gov/nccdphp/publications/aag/pdf/doh.pdf . Accessed Oct. 27, 2010.
2. Roberts DR, Maragliano PM, Chapman RJ. Put the plan into action: how to implement a successful and efficient caries prevention program. Dimensions of Dental Hygiene. Jun 2011; 9(6):70-73.
3. Low W, Tan S, Schwartz S. The effect of severe caries on the quality of life in young children. Pediatr Dent Sept.-Oct. 1999; 21(6):325-326. (www.ncbi.nlm.nih.gov/pubmed/10509332)
4. http://www.surgeongeneral.gov/topics/oralhealth/nationalcalltoaction.html (Surgeon General “Call to Action”)
5. http://www.surgeongeneral.gov/news/testimony/ageism09222003.htm
6. MacEntee M. Quality of life as an indicator of oral health in older people. JADA, Sept 2007; 138:47S-52S.
7. Journal of the California Dental Association. Oct. & Nov. 2007.
8. Kidd EA. Caries management. Dent Clin North Am. Oct. 1999; 43(4):743-764.
9. Jenson L, Budenz AW, Featherstone JD, Ramos-Gomez FJ, Spolsky VW, Young DA. Oct. 2007; 35(10):714-723.
10. Steinberg S. Adding caries diagnosis to caries risk assessment: the next step in caries management by risk assessment (CAMBRA). Compend Contin Educ Dent. Oct. 2009; 30(8):522, 524-526.
11. Fontana M, Young DA, Wolff MS. Evidence-based caries, risk assessment, and treatment. Dent Clin North Am. Jan. 2009; 53(1):149-161.
12. Featherstone JD. The caries balance: the basis for caries management by risk assessment. Oral Health Prev Dent. 2004; 2 Suppl 1:259-264.
13. Roberts DR, Maragliano PM, Chapman RJ. Put the plan into action: how to implement a successful and efficient caries prevention program. Dimensions of Dental Hygiene. Jun 2011; 9(6):70-73.
14. Featherstone JDB, Domejean-Orliaguet S, Jenson L, Wolff M, Young DA. Caries risk assessment in practice for age 6 through adult. J Calif Dent Assoc. Oct 2007; 35(10):703-713.
15. Humphrey SP, Williamson RT. A review of saliva: normal composition, flow and function. J Prosthet Dent. Feb 2001; 85(2):162-169.
16. Navazesh M, Kumar SK. Xerostomia: prevalence, diagnosis and management. Compend Contin Educ Dent. Jul.-Aug. 2008; 30(6):326-334.
17. Glore RJ, Spiteri-Staines K, Paleri V. A patient with dry mouth. Clinical Otolaryngology. Aug. 2009; 34(4):358-363.
18. Guggenheimer J, Moore PA. Xerostomia: Etiology, recognition and treatment. JADA. Jan. 2003; 134:61-69.
19. Jenson L, Budenz AW, Featherstone JDB, Ramos-Gomez J, Spolsky VW, Young DA. Clinical Protocols for Caries Management by Risk Assessent. J Calif Dent Assoc. Oct. 2007; 35(10):714-723.
20. http://www.gcamerica.com/products/preventive/GC_Tri_Plaque_ID/index.php
21. Featherstone JDB, Domejean-Orliaguet S, Jenson L, Wolff M, Young DA. Caries risk assessment in practice for age 6 through adult. J Calif Dent Assoc. Oct 2007; 35(10):703-713.
22. Jenson L, Budenz AW, Featherstone JDB, Ramos-Gomez J, Spolsky VW, Young DA. Clinical protocols for caries management by risk assessment. J Calif Dent Assoc. Oct. 2007; 35(10):714-723.
23. Twetman S. Antimicrobials in future caries control? A review with special reference to chlorhexidine treatment. Caries Res. 2004; 38:223–229.
24. Duarte AR, Peres MA, Vieira RS, Ramos-Jorge ML, Modesto A. Effectiveness of two mouth rinse solutions in arresting caries lesions: a short-term clinical trial. Oral Health Prev Dent. 2008; 6:231–238.
25. Maragliano-Muniz PM, Roberts DR, Chapman RJ. Classification system for root surface quality. Inside Dentistry, Jan. 2012.
Table 1: Caries Risk Factors
- Xerostomia
- Caries within 3 years
- Incipient caries/ demineralization
- Orthodontics
- Recreational drug use
- Gingival recession
- Diet high in sugar/carbs/acids
- Deep pits and fissures
- Growing up without access to fluoride
- Extensive restorations (10+ surfaces)
- Removable partial dentures
- Fixed partial dentures
- 60+ years of age
- Smoking
- Infectious contact
- Inadequate oral hygiene
Table 2: Caries High-Risk Factors
- Xerostomia
- Caries within 3 years
- Incipient caries/ demineralization
- Orthodontics
- Recreational drug use
- Extensive restorations (10+ surfaces)
- Removable partial dentures
- Fixed partial dentures
- Smoking
- Infectious contact
DR. PAMELA M. MARAGLIANO-MUNIZ is a board-eligible prosthodontist. She earned her certificate from the UCLA School of Dentistry after obtaining her DMD from Tufts University School of Dental Medicine. She is also a former dental hygienist who earned her BSDH degree from Northeastern University and the Forsyth School for Dental Hygienists, AAS in dental hygiene, and AS degree in math and science from SUNY Orange. Since being awarded the 2010 Adult Preventive Care Practice of the Year by the American Dental Association, Dr. Maragliano-Muniz lectures nationally. She has recent publications that discuss implementing CAMBRA in the private practice and the clinical effects of CAMBRA on root surfaces. Dr. Maragliano-Muniz is an assistant clinical professor at Tufts University School of Dental Medicine and maintains private practices at Charles River Dental in Boston, Mass., and with Gary Wheeler, DDS, in Lynn, Mass. Dr. Maragliano-Muniz maintains professional memberships with the American Dental Association, Massachusetts Dental Society, American College of Prosthodontists, and the American Dental Education Association. You may contact her by email at [email protected].
DONA R. ROBERTS, RDH, currently practices with Lewis Wharf Dental Associates in Boston. Her caries management and periodontal protocol programs in private practice were recognized nationally by the ADA in 2010 as the office was awarded the Preventive Practice of the Year. She has extensive experience consulting, volunteering and presenting continuing education lectures.
ROBERT J. CHAPMAN, DMD, is a Professor Emeritus at Tufts University School of Dental Medicine and maintains a private practice in Boston.
Past RDH Issues