Safe water delivery
Advances in water line infection control aid the hygienist's role in safety
By Karen Siebert, RDH, MA
Hygienists have not always thought of dental unit water line (DUWL) infection control as our responsibility, but it is just as crucial to patient and practitioner safety as cleaning and disinfecting a countertop. With new choices in water line disinfection products, choosing wisely can do more than maintain a safe level of colony-forming units (CFUs).
Historically, water lines have not been a topic of discussion among hygienists. As champions of personal protection equipment, surface disinfection, and instrument care, water lines fell under equipment maintenance -- the quick "have to's" at the end of the day to keep the unit running, not critical infection control. Trusting that the little tablet dropped in the water bottle was all we needed to assure a fresh water supply, we didn't put much more thought into the issue.
Today there is an abundance of evidence that it takes more than one step to maintain a healthy water supply. "Drop in and forget" is no longer an option. The maze of tiny tubes that connect water to the delivery point have been shown to be an ideal environment for biofilm growth, linking DUWL safety directly into the chain of asepsis. As hygienists, we need to place DUWL health right up there with visible surfaces. A daily, weekly, and monthly routine should be followed to ensure safe water delivery.
-------------------------------------------
Consider reading these articles
- Cleaning or disinfection: What's right for the suction lines?
- Elimination of contaminants in waterlines may be guesswork, but several options help
- Legionnaires’ disease and dental unit water
-------------------------------------------
Hygienists have exciting choices with a new generation of DUWL products that offer a good "bang for the buck." Sustainable products compatible with the health of the environment and humans are now options, exposing patient, practitioner, and environment to fewer chemicals. One of hygiene's favorite oral rinses, 0.12% chlorhexidine gluconate is also an environmentally- and human-friendly germicide that has a long history of successful biofilm removal in dental unit water lines. With the original report of contaminated water bottles 50 years ago, chlorhexidine gluconate was the first germicide used to address the issue. Well documented as safe for patients and the environment, 0.12% chlorhexidine gluconate is proven to kill P. aeruginosa.
This new generation of products with a chlorhexidine base has uses beyond DUWL treatment. It can be used as an initial shock treatment or for weekly or daily line maintenance to effectively remove biofilm from lines. During the clinical day, chlorhexidine DUWL treatments can also be used as an irrigant. Combining multiple benefits into one product simplifies a previously puzzling topic in infection control. As hygienists, we know the safety and benefits of chlorhexidine gluconate. Products approved for intraoral use reduce worry about chemical exposure to harsh biofilm disruptors in line cleaners, and have the potential to enhance treatment outcomes when used as an irrigant.
Why is this so important? Since 1963 when the first report of contaminated water bottles appeared, evidence has been compounding that patients and practitioners exposed to treatment water with greater than 500 CFU/ml are at risk for several gram-negative bacterial and fungal related illnesses. Immunocompromised patients are especially susceptible to these infective organisms. Mainstream media has picked up on this topic, most recently reporting the death of an 82-year-old Italian woman from L. pneumophila pneumonia linked to dental unit water lines (Ricci, ML, et al., 2012).
Patients are not the only ones at risk -- practitioners are exposed to aerosols produced by high-speed handpieces and ultrasonic scalers. Proper personal protective equipment does not eliminate exposure entirely, still posing the risk of infectious microorganism aspiration. Proper DUWL care reduces microorganisms present in aerosols produced from high-speed and ultrasonic handpieces (IADR Loma Linda University, 1999). Several studies have shown antibodies to Legionella present in dental health-care workers exposed to DUWL aerosols (O'Donnell, et al., 2011). This underscores the importance of reducing inhaled microorganism counts from treatment water aerosol.
Based on the studies since 1963, both the CDC and EPA have weighed in on the topic, setting standards for safe levels of treatment water. The 2003 CDC Guidelines for Infection Control in Dental Health Care Settings states, "Use water that meets EPA regulatory standards for drinking water for routine dental treatment water output." The EPA has set the standard for drinking water at < 500 CFU/ml (colony-forming units per milliliter). In 1996 the ADA challenged practitioners to set a goal of <200 CFU/ml, but has since adapted their recommendation to align with the CDC.
Pesky biofilm
Biofilm is a current buzzword in dentistry, and for good reason. By definition, biofilm is a cohesive, living community of organisms that supports itself through an efficient system of attachment and communication. When a biofilm first begins to form, it is a fairly weak layer. As the community becomes more complex, a thick layer of infectious organisms lines the DUWL. The dynamics of water flow within the line allows a patchy film to form on the tube wall. Holes in the biofilm function as communication and nutrient channels. As treatment water flows through these channels, chunks of biofilm dislodge and travel to the patient's oral cavity, depositing a variety of organisms with the potential to cause illness.
Organisms of concern are gram-negative bacteria P. aeruginosa, Legionella, and non-tuberculosis Mycobacterium species. Candida fungal organisms also make themselves at home within the DUWL biofilm. According to the CDC report, "Pseudomonas aeruginosa in Healthcare Settings," P. aeruginosa can cause a wide variety of infections in humans, especially those with weakened immune systems. People without immunocompromised systems are not risk free -- skin rashes or ear infections have developed after exposure to water contaminated with P. aeruginosa.
Dental tubing is a perfect host for several reasons. Tubing is narrow, with a relatively low volume to surface ratio. Water flow concentrates in the middle of the tube -- very little force touches the walls of the tube, leaving the biofilm undisturbed. There is substantial downtime when water sits in the lines overnight and on weekends. Brand new tubing can form a significant biofilm colony in just five days when these factors exist (American Dental Association, 2013).
Figure 2 shows a brand new tube free of biofilm, while Figure 3 shows a DUWL tube with only three weeks of biofilm growth. Once established in an optimal environment, a biofilm community has the ability to rapidly multiply and establish a well-protected shell against disruption.
Establishing an office protocol for DUWL management and using products proven to reduce CFUs to acceptable levels are critical to preventing biofilm from taking hold and causing serious infections in patients and staff. The Centers for Disease Control recommends flushing water lines for 20 to 30 seconds between patients. This encourages removal of bacteria retracted during the previous patient treatment, but has no effect on the established biofilm within the lines.
Not too long ago it was common to recommended flushing DUWLs for several minutes at the beginning and end of a treatment day to prevent biofilm adherence. This has now been shown to be ineffective for disrupting established biofilm and is no longer recommended.
There are three critical steps to consistent DUWL health -- test, shock, and maintain. Initial testing is critical to establishing the next step. If water tests over 500 CFUs/ml, an initial shock treatment is in order to clear out established biofilm. Once cleared, a daily maintenance routine should be established.
Testing options include in-office or laboratory. In-office testing is considered screening. These chairside tests do not reliably show correct microorganism levels, while some types of organisms are not recognized at all (Porteous, 2013). Laboratory testing is much more reliable, relatively inexpensive, and accurate. To collect samples, follow the lab test recommendations carefully in order to avoid inaccurate results. When done correctly, organisms harbored in DUWL biofilm can be identified within a reasonably accurate range, allowing offices to effectively plan the next step in treatment.
If lab results return at levels greater than 500 CFUs/ml, shock treatment is in order. A shock treatment is designed to completely dislodge an established biofilm from the DUWL tubing. After achieving complete removal, daily or weekly maintenance will slow or prevent new adherence.
Several attributes should be considered in choosing a shock product. Studies show residual shock chemicals in post-treatment water (O'Donnell, et al., 2011). Chlorine-, gluteraldehyde-, and isopropanol-based shock products have effectively removed biofilm, but concern for patient and environmental exposure to these chemicals should be considered. Products that have both FDA and EPA approval are most likely to be safe for patients and the environment. See ADA professional resources for more information on available shock products.
Once biofilm has been removed from DUWLs with a shock product, a daily-use product is needed to maintain safe CFU levels. Since these products will be present in treatment water, it is time to be picky about the ingredients and effect on patients, practitioners, and environment.
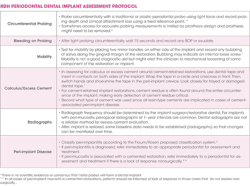
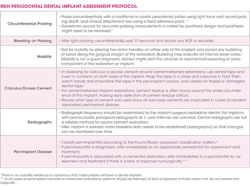
Attributes of chemicals used in DUWL cleaners
Chlorhexidine gluconate 0.12% has been shown as efficacious against a broad spectrum of heterotrophic bacteria and Candida spp. It is FDA cleared for intraoral use and environmentally friendly. A typical routine for line maintenance using a chlorhexidine-based product will be fairly time efficient because there is a lack of caustic residue in the treatment water. Post-line-treatment flush times will be reduced, and patient treatment can immediately resume after each use.
Sodium hypochlorite, otherwise known as bleach, is efficacious against heterotrophic bacteria and was the first recommended chemical for DUWL treatment. The process is time consuming, taking two hours to complete. When it is in contact with biofilm, it has been found to release chloroform (Puttaiah, et al., 1998). These two drawbacks have reduced the popularity of bleach. Depending on the concentration, it can be corrosive to equipment.
Chlorine dioxide is considered a better option than bleach. It has less potential to cause corrosion in equipment, and is bactericidal. Concentrations above EPA limits may cause skin, eye, and respiratory irritation.
Hydrogen peroxide is most effective when it oxidizes. In a study comparing several different concentrations of hydrogen peroxide against a control unit, hydrogen peroxide was shown to be effective for maintaining acceptable levels of CFUs in biofilm-free tubing. When an established biofilm was present, it took up to two months of continuous line treatment before reaching acceptable CFU levels.
Glycerin is commonly known as a separating agent and may cause insufficient bonding when present in treatment water during bonding procedures. It has no other adversarial effects.
Choosing a line cleaner that meets the criteria discussed can offer a return on investment in multiple areas. As a marketing tool, promoting a practice infection control protocol using environmentally- and health-friendly products instills confidence in patients that they are receiving the best care possible. Patients looking to patronize green businesses will appreciate your efforts to conserve environmental resources and minimize chemical exposure. Sharing practice updates via an e-newsletter will offer patients a new reason to recommend your practice to their friends.
All line cleaners deposit residue into treatment water, exposing patients and staff to the chemical in the treatment (Epstein, et al., 2002; O'Donnell, et al., 2011). A sustainable product that does not cause respiratory, skin, or eye irritation keeps practitioners free of unpleasant illnesses or irritations, guaranteeing an energized staff ready to deliver excellent care. As a bonus, gentler ingredients with a balanced pH ensure longevity for costly dental equipment, and discourage corrosion of expensive parts of the dental chair unit, saving on premature replacement of equipment.
Newer generation line treatments are environmentally friendly and beneficial for intraoral use. Aerosols generated contain less bacteria and chemical irritants than line cleaners formulated with some of the active ingredients noted above. Adding xylitol increases palatability when used as a procedural irrigant, and shows promise as a bactericidal agent. Since xylitol is already known for its inhibition of S. mutans in the oral cavity, it would be beneficial to carry out studies that evaluate whether xylitol has any bactericidal effects on water line biofilm.
While one more task thrown into a busy hygienist's schedule is not ideal, when the potential consequences of an inconsistent or ineffective DUWL treatment plan are considered, there is no choice but to put patient and staff health first. Involving the entire team can make DUWL treatment an office mission focused on what is best for everyone, and the importance will outweigh the extra step in the day. Share your mission to use effective, sustainable products with your patients. They will appreciate your professionalism and efforts to keep them healthy. They may even brag about their dental team.
Karen Siebert, RDH, MA, earned a degree in dental hygiene from the University of Iowa and a master's in education with an emphasis on teaching with technology. She teaches oral pathology and theory and practice of dental hygiene to second year dental hygiene students. She is a clinical instructor at all levels. Volunteer positions include local component trustee and state membership chair for the Illinois Dental Hygiene Association, and committee member of Northern Illinois Oral Cancer Walk for Awareness. She is a member of ADEA and a 2013/2014 member of Career Fusion.
References
American Dental Association, 2013, Oral health topics: water lines, dental unit. http://www.ada.org/2756.aspx?currentTab=2. Accessed August, 2013.
Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases Division of Healthcare Quality Promotion, Pseudomonas aeruginosa in healthcare settings. http://www.cdc.gov/hai/organisms/pseudomonas.html. Accessed August 19, 2013.
CDC Guidelines for infection control in dental healthcare settings – 2003. MMWR 2003; 52(RR17) http://www.cdc.gov/healthywater/other/medical/med_dental.html#more_info. Accessed August, 2013.
Epstein J, Dawson JR, Buivids I, Wong B, Le N. The effect of a disinfectant/coolant irrigant on microbes isolated from dental unit water lines. Spec Care Dentist 2002 22(4): 137-141, 2002.
Lin S, Svoboda K, Giletto A, Seibert J, Puttaiah R. Effects of hydrogen peroxide on dental unit biofilms and treatment water contamination. European Journal of Dentistry. 2011;5(1):47–59. Available at: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3019751&tool=pmcentrez&rendertype=abstract.
O'Donnell M, Boyle M, Russell R, Coleman D. Management of dental unit water line biofilms in the 21st century. Future Microbiol, 2011 6(10), 1209–1226.
Porteous N. (2013, January). Dental unit water lines. OSAP Core Training IP & S Symposium, Dallas, TX.
Ricci ML, Fontana S, Pinci F, et al. Pneumonia associated with a dental unit water line . Lancet 2012; 379 (9816): 684.
Richards S, Fitzmorris L, Doan TN, Kuniyoshi KS, Nguyen HH. (1999) The effectiveness of Bio2000 – a chlorhexidine gluconate dental handpiece irrigation solution – in the reduction of aerosolized bacteria produced during dental procedures. IADR, Loma Linda University School of Dentistry Student Research Program.
Srinivasan A, Bova G, Ross T, et al. A 17-month evaluation of chlorine dioxide water treatment system to control Legionella species in a hospital water supply. Infect Control Hosp Epidemiol. 2003 Aug;24(8):575-579.
Relevant Internet articles
http://www.ada.org/sections/professionalResources/pdfs/cleaning_water lines4.pdf
http://www.osap.org/?page==issues_DUWL_1&hhSearch
Guidelines from The Centers for Disease Control direct office efforts in achieving healthy water treatment:
1. Use water that meets nationally recognized standards set by the EPA for drinking water (<500 CFU/mL for heterotrophic plate count) for routine dental treatment output water. 2. Take precautions to prevent waterborne contamination of dental unit water lines and instruments: 1. After each patient, discharge water and air for a minimum of 20 to 30 seconds from any dental device connected to the dental water system that enters the patient's mouth (for example, handpieces, ultrasonic scalers, and air/water syringe). 2. Consult with dental water line manufacturers to: 1. Determine suitable methods and equipment to obtain the recommended water quality, and 2. Determine appropriate methods for monitoring the water to ensure quality is maintained.3. Consult with the dental unit manufacturer on the need for periodic maintenance of antiretraction mechanisms.
Here is a list of questions to ask about a daily line cleaner:
- Is this product FDA and EPA approved? Asking this covers sustainability, germicidal claims, and patient compatibility.
- Is this product compatible with your equipment?
- Are any of the ingredients considered carcinogens or hormone disrupters?
- Does the active ingredient kill a wide spectrum of microorganisms? For example, non-tuberculosis mycobacteria are resistant to iodine and chlorine.
- What is the recommended contact time for product effectiveness? Effective biofilm disruptors have to sit in the lines for maximum effectiveness. Promises of results without extended contact time are unlikely to consistently perform.
- What is the pH of the product? pH-neutral products do not corrode or damage equipment.
- Do any of the ingredients affect material bonding capabilities? Glycerin has been shown to negatively impact the bonding capability of composite materials.
- What is the cost per treatment?
- Can this product be used for shock treatment as well as daily/weekly maintenance?
- Is it time efficient for staff?
Past RDH Issues