Selecting the right needle: Making the right choice for local anesthesia
Needle selection is a very important component for the safe and effective provision of local anesthesia. Selection is often influenced by one or more of the following:
- What we learned in school
- What is available at the office
- Employer preferences
- What we think will be most comfortable for the patient
However, the main criteria for needle selection should include injection type to be administered, the depth of penetration and thickness of tissue, and vascularity of the tissues/potential for hematoma.
Needle anatomy: The main components of the dental anesthetic needle include the bevel, shank, hub, syringe adaptor, and cartridge penetration end. The syringe adaptor/hub complex is commonly referred to as the "hub" (Figure 1).
Needle length: Dental needles most commonly found in the dental office are the long, short, and ultra-short. The two most common lengths of needles used by dental hygienists for intraoral injections with the traditional syringe are the "long" and the "short" (Figure 2). The length of the needle can vary some by manufacturer, but usually, from hub to tip, a long needle is about 32 mm (1.5 inches) and the short is about 20 mm (1.0 inch).
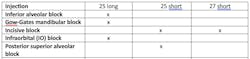
The long needle is required for the various mandibular blocks because the depth of penetration ranges from approximately 20-25 mm for an average adult. The long needle is also recommended (adults) for the Infraorbital (IO) block injection. A short needle is usually preferred for the posterior superior alveolar injection (PSA) to avoid overinsertion; for supraperiosteal injections; and tissue infiltrations.1-3 (Table 1)
It is extremely important to avoid insertion to the hub, the weakest part of the needle. At the hub, the needle can break more easily. If the needle does break, and if it is not visible, it would likely be lost in the tissues and very difficult to retrieve.1,2 The risk of needle breakage also occurs if the needle is bent, forced, the direction is changed, or it is a 30-gauge needle.
Needle gauge: The gauge of the needle represents the diameter of the lumen, the hollow tunnel within the needle. In dentistry, common gauges include: 25, 27, and 30. The larger the number, the smaller and thinner the gauge. Gauge selection should be determined by depth of injection and risk of intravenous injection. 1,2
Although clinicians often feel that using the thinner gauge needles is more comfortable for the patient,it is important to emphasize that hundreds of studies over several decades have indicated that patients cannot tell the difference between 25-, 27-, and 30-gauge needles, even without topical application. Patient comfort is reliant on clinician technique! 1-4
With the larger gauge (25 or 27) needles, because they are more rigid, there is resistance to needle breakage and less deflection as the needle advances through deeper tissues, which then results in greater accuracy for reaching the desired target. More importantly, aspiration is much more reliable since the larger lumen facilitates ease of aspiration.
You might also be interested in: Selecting local anesthetic agents for nonsurgical periodontal therapy
The 25-gauge needle is strongly recommended for all injections with a high risk of positive aspiration and/or with a significant depth of penetration. The 27-gauge needle is recommended for other injections where depth of penetration and risk of positive aspiration are minimal (Table 1).1-3 The 30-gauge needle is not recommended for supraperiosteal or block injections with the standard syringe, but can be useful for localized infiltration (injecting the papillae to obtain hemostasis), and is used with computer-controlled local anesthesia delivery systems (CCLAD).1
Needle bevel: The bevel is the slanted surface of a needle, which creates the tip and facilitates nontraumatic entry into tissues (Figure 3). Manufacturers often describe bevels as short, medium, long, multi beveled, and scalpel. 1-2 Experts have indicated that the angle of the bevel as it relates to the long axis of the needle may affect the degree of needle deflection.1-3 The greater the angle is with the long axis of the of the needle, the longer is the deflection in the soft tissues. Several years ago, Septodont developed the newer innovative scalpel designed bevel (Figure 3, middle). The purpose of the design is to allow for smoother penetrations, less tissue displacement, less deflection, and less force required of the clinician. This design is useful for infiltration and periodontal ligament (PDL) injections, but is not recommended for nerve blocks where the nerve could be contacted.1,2 They also developed a triple-bevel needle with a larger bore to reduce pressure needed to deliver the anesthetic and thereby reduce pain during injections (Figure 3).
Although not critical to the success of injections, bevel design remains a topic of discussion and study.5 The orientation of the bevel should be toward the bone during injections that are close to the periosteum. Doing so increases patient comfort and reduces trauma to the periosteum if bone is contacted.
Metal versus plastic hubs: The metal or plastic needle syringe adaptor/hub complex, the "hub," attaches the needle to the syringe. Metal hubs are pre-threaded and must screw down tight to avoid loosening and often the bevel or syringe window will be out of position. Once screwed down tight, they can then be more difficult to remove, removing the needle adaptor of the syringe (if present) with them. The plastic hubs are usually self-threading and usually fit all syringes well, including syringes which have needle adapters that are stripped or have defects. They are easy to rotate for bevel alignment and they are resistant to removing the needle adaptor. Many manufacturers of plastic needle hubs include a dot or arrow indicating the location of the bevel (Figure 1).
Special considerations
When contact with bone is required prior to deposition, the contact should be gentle. A fishhook-type barb may be observed on the tip of the needle (Figure 4) due to a manufacturing error, but more often it is caused from the needle contacting the bone forcefully during an injection. As a result, the patient experiences pain during withdrawal.
Over time, most of us adapt our techniques so that, regardless of the features of our armamentarium, we can reach our targets to provide successful anesthesia. However, needle selection is a very important consideration for safe and effective provision of local anesthesia. The main criteria for needle selection remains consideration of the type of injection to be administered, the distance to the target, and the vascularity of tissues.
Editor's note: Originally posted in 2015; updated in 2023 by the author
References
1. Malamed S. Handbook of Local Anesthesia. 7th ed. Elsevier; 2020.
2. Logothetis D. Local Anesthesia for the Dental Hygienist. 3rd ed. Elsevier; 2022.
3. Bassett, DiMarco, Naughton. Local Anesthesia for Dental Professionals. Pearson; 2010.
4. Flannagan T, Wahl MJ, Schmidt MM, Wahl JA. Size doesn't matter: needle gauge and injection pain. Gen Dent. 2007;55(3):216-217.
5. McPherson J, Dixon S, Townsend R, Vandewalle K. Effect of needle design on pain. From Dental Local Anesthetic Injections. Anesthesia Progress. 2015;62(1):2-7.
About the Author

Laura J. Webb, MS, RDH, FAADH
Laura J. Webb, MS, RDH, FAADH, is an experienced clinician, educator, and speaker who founded LJW Education Services (ljweduserv.com). She has provided educational methodology courses and accreditation consulting services for allied dental education programs and CE courses for clinicians. Laura has frequently spoken on the topics of local anesthesia and nonsurgical periodontal instrumentation. She was the recipient of the 2012 ADHA Alfred C. Fones Award. Laura can be reached at [email protected].
Updated May 2023