Intraoral professionally applied topical anesthetics
Review the types of topical anesthetics that can be used safely by hygienists
Laura J. Webb, RDH, MS, CDA
In order to achieve optimum outcomes, we know from the literature that we should consider every approach to thorough debridement. The administration of local anesthesia is an important component for adequate pain management and hemostasis during comprehensive root instrumentation (manual or power) at therapeutic debridement appointments—sometimes during regular preventive oral maintenance. Effective anesthesia allows the clinician to provide treatment painlessly—especially in areas of challenging pocket topography, root anatomy, and inflammation—while maximizing access for instrumentation.
The chief role of topical anesthetics has been their routine use at insertion sites prior to injections to facilitate atraumatic injections. Since topical anesthetics do not provide pulpal anesthesia (except Kovanaze, which is discussed below), it is not prudent to use them as a substitute for local anesthesia when root sensitivity is a concern or when a greater depth and/or duration of anesthesia is required.1,2
When properly administered, topical anesthetics usually provide anesthesia of oral mucosa to a depth of 2-3mm. They can be very useful for procedures which may not require injections, such as probing, scaling in presence of inflammation, and alleviating gag reflex (radiographs, impressions).
The many preparations of topical anesthetics available for dentistry are vasodilators, which act similarly to injectable local anesthetics; however, they are of a higher concentration to facilitate diffusion through the mucous membranes.1-3 This also includes the many over-the-counter (OTC) preparations. Topical anesthetics do not contain vasoconstrictors (except Kovanaze), so cardiovascular system (CVS) absorption of some of these agents may be rapid and increase risk of toxicity/overdose.
Toxicityis influenced by an agent’s ability to penetrate tissue, the speed of systemic absorption and the total area of coverage.4 Areas of inflammation, abrasion, or injury are likely to have an increased speed of systemic absorption, increasing the risk for toxicity. Although localized reactions to anesthetics are rare, they can occur after prolonged or repeated use.3 This is confounded further by the diversity of agents, forms, and methods of application that can affect accuracy of dose determination. It is for this reason, for example, that the base forms (insoluble in water) of benzocaine and lidocaine are preferred as they are more slowly absorbed into the CVS and are less likely to produce an overdose when administered properly.2-5 Precautions increase when tissues are highly abraded and when applied to large areas.
Types of topicals
Professional forms of topical anesthetics include gels, sprays, liquids, ointments, and patches. They may be applied with the use of cotton tip applicators, patches, blunted cannulas/syringes, or aerosol containers with cannulas. Products may be available in multidose containers and/or single-dose applicators. The single unit-dose applicators help prevent cross contamination and allow for more accurate determination of dosage.
- Gels and ointments usuallywork best for site-specific pre-injection insertion sites and are not generally recommended for widespread areas or pockets. They are typically applied with cotton-tipped applicators or single unit-dose applicators, such as HandiCaine Stix. Care should be demonstrated when using cotton-tipped applicators to avoid overloading the applicator with excessive agent.
- Liquids are useful for site-specific procedures such as pocket anesthesia, but are less useful for site-specific pre-injection insertion sites since liquids are more difficult to confine on the surface tissues. Typically, a cotton pellet or a blunted syringe or cannula is used to deliver liquids subgingivally. Some liquids are used as a “rinse” by patients to allow for a more generalized application to gingival tissues or to decrease the gag reflex.
- Sprays may be metered (measured doses) or unmetered and are most often used for reducing gag reflex during intraoral radiography or the taking of impressions. Unmetered sprays are not recommended as they provide uncertain dosage and are difficult to confine to a specific site. As they are difficult to control they are potentially dangerous.2,3,6 Care should be taken to avoid patient inhalation of the spray.7
- Patches are not as commonly used as they once were and at the time of development of this column, there was only one patch product available: Topacale GelPatch (discussed below), from Premier.
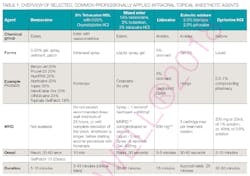
General information for selected professionally applied intraoral topical anesthetic agents is shown in Table 1. Check agent-specific package inserts for updates and details regarding use for special populations, maximum recommended dose (MRD), and general contraindications.
Tips for topical success
1. Patient preparation: Review medical history to customize the best and safest agent as well as method of application for each patient. Query the patient to learn about previous experiences with anesthetics and if they self-medicate with any topical anesthetic agents. This is important for total dose consideration.
2. Application: Ensure proper expiration date of the agent. Explain the procedure to the patient. Follow the directions for the agent. If using multiuse gel or ointment, use aseptic technique, and place a small amount of agent on the cotton-tip applicator and place on 2x2. Only a small amount of agent is needed to be effective. Too much may lead to inadvertently anesthetizing other oral structures. Dry the site (facilitates better agent penetration and less dilution) and allow the agent to remain at site for designated period of time.6
3. Documentation: Include the location and total dose of topical anesthetic provided. Consider MRD with regard to injectable local anesthetics and patient OTC use. For example, when lidocaine ointment 5% is used concomitantly with other products containing lidocaine, the total dose contributed by all formulations must be kept in mind.17
Esters
Benzocaine isthe most popular and most frequently used topical anesthetic agent in dentistry.2-5 It is available in 6-20% concentrations; however, the 20% preparations are the most often used. Forms include gel, spray, liquid, ointment, and gel-patch, and benzocaine is marketed in both multi-use and single-unit doses.
The onset of action for benzocaine is rapid and it reaches its peak effect at two minutes. In base form, it is poorly soluble and therefore is slowly absorbed into the CVS which results in a very low potential for overdose.5 The 18% benzocaine Topacale gel-pump dispenser (Premier Dental) provides ease of dispensing, minimizing waste, and reduces potential cross-contamination.8 The flexible 18% Topicale GelPatch dissolves gradually once placed in the mouth, anesthetizing the surface tissue for up to 20 minutes. The GelPatch may be used prior to injections (especially handy for palate). If desired, the needle can actually be inserted through the patch while it is in place. The patch is also useful for denture sores, oral ulcers, and irritations.9
GingiPak’s GINGICaine Oral Anesthetic Gel in syringe form allows placement of 20% benzocaine gel directly into the gingival sulcus. Since allergic (usually localized) reactions to benzocaine are possible, especially with prolonged or repeated application7, it should be avoided in individuals who are allergic to esters/PABA and are at risk for methemoglobinemia. Methemoglobinemia has been reported with the use of the higher concentration (14-20%) sprays.2
This discussion of 3% tetracaine HCLwith 0.05% oxymetazoline HCl(vasoconstrictor) is based on the “needleless” intranasal spray dental local anesthetic, Kovanaze Nasal Spray. The spray received Federal Drug Administration (FDA) approval in 2016. It is indicated to provide regional pulpalanesthesia when performing restorative procedures on teeth #4-13 and A-J for individuals who weigh 88 pounds or more.
Although the approval was restorative procedure focused, we may find that Kovanaze can also be useful for our hygiene patients, particularly those who require only pulpal anesthesia in the maxillary anterior and premolar regions. The effect on soft tissues associated with scaling and root planning has not yet been determined.
The Ciancio et al. clinical trial, which included testing of the incisive papilla and the palatal foramen, reported successful anesthesia in those areas. The authors suggested that this may be due to the proximity of the nasal spray target to the greater palatine nerve and maxillary sinus.11,12 The study also indicated some success for pulpal anesthesia for maxillary first permanent molars.11,12
Kovanze is formulated in a pre-filled, single-use nasal sprayer and is intended for intranasal use only. Administration should be on the same side of the maxillary tooth being treated. Administer two sprays, four minutes apart. For adults, 18 years of age or older, administer one additional spray if adequate anesthesia has not been achieved 10 minutes after the second spray. “Generally safe and well-tolerated with no serious side effects in study participants.” 10 Contraindications include: known hypersensitivity to tetracaine, benzyl alcohol, ester local anesthetics, PABA, oxymetazoline, or any other component of the product; and patients who exhibit uncontrolled hypertension, active thyroid disease, are taking MAOIs, nonselective B-blockers, tricylic antidepressants, or who experience frequent nosebleeds.1,10
Mixed agents, such as 14% benzocaine, 2% butamben, and 2% tetracaine, comprise a triple-ester mixture. The combination facilitates a short onset of action and long duration of anesthesia. The benzocaine contributes a fast onset but short duration; the butamben provides both an intermediate onset and duration; and the tetracaine contributes a slow onset but long duration.
Cetacaine enjoys a long history of use in dentistry.1 It is available by prescription in spray, liquid and gel. The liquid formulation is particularly useful for subgingival application. Cetacaine liquid comes in a bottle with a Luer-lock receptacle in the cap that allows for the attachment of a Luer-lock “draw-what-you-need” syringe to draw the anesthetic and comfortable application with the microcapillary tip. The flavor is mild and well- tolerated. It has a superior duration of up to an hour. The 30g bottle holds enough to treat 300 quadrants at maximum dosage. The doses are easily measured on the clearly marked syringe.
Cetacaine spray is the only FDA-recognized topical anesthetic for suppressing the gag reflex on-label. The dose is for a one-second spray. The stainless-steel cannula is autoclavable, and safe to use (won’t shoot off like plastic straws can). The bottle can be held at any angle and still sprays.13The triple-ester mixture should be avoided in individuals who are allergic to esters/PABA and at risk for methemoglobinemia.
Amides
The professional lidocaine topical anesthetic is formulated in a 5% ointment. There are also several OTC forms available ranging from 2.5-4%, including an HCL form which, as previously noted, is not recommended due to the increased risk of toxicity with the water soluble agents. Dentists sometimes purchase one or more of the OTC lower concentrations of lidocaine for use in the dental office.
It is important to note that the risk of overdose with amide topical anesthetics is greater than with esters and increases with the area of application.3 Although the use of topical lidocaine for dentistry is far less common than that of benzocaine, lidocaine is a good alternative for patients for whom esters may be contraindicated.2
An eutectic is a mixture of two (or more) substances that together have a lower melting point than components individually. The FDA-approved dental eutectic amide mixture, Oraqix (2.5% lidocaine and 2.5% prilocaine) from Dentsply Pharmaceutical, was introduced in 2004. It is a soft tissue anesthetic intended for subgingival use during nonsurgical periodontal debridement. Lidocaine provides a more rapid onset and prilocaine, which is less toxic and potent than lidocaine, has a slightly longer duration of action.5
Oraqix is a unique eutectic mixture due to the thermosetting agents it contains that allow it to change from liquid (in the cartridge) at room temperature to an elastic gel when introduced into the periodontal sulcus where it remains at the site long enough to provide site-specific anesthesia. The specialized delivery system (Oraqix dispenser, cartridges, and cannula) facilitates ease of delivery and control of dosage. One cartridge (1.7g) or less of Oraqix is usually sufficient for one quadrant. The MRD for Oraqix is five cartridges per treatment session.2,14 Because of the presence of prilocaine, the mixture should be avoided in individuals who are at risk for methemoglobinemia.1,4
Once marketed as Dyclone, dyclonine hydrochloride (0.5-1%), a liquid, is now available for dentistry by prescription only through compounding pharmacies.2 However, a commercially available product may be available soon. Dyclonine HCl is classified as a ketone and therefore is particularly useful for patients who are sensitive to amide or ester topical anesthetics.1-3 It is most often used as a mouth rinse to anesthetize a wide area of gingival tissues. Although the onset of action is slow, the duration is reported as 30-60 minutes and it provides very good anesthesia. For maximum effect, patients should “swish” without swallowing for one minute and then “spit.” Due to poor water solubility, the overdose potential is very low.4 Dyclonine HCl is commonly found in OTC preparations such as anesthetic lozenges.
Studies indicate that the use of a refrigerant topical agent prior to palatal injections may decrease application time, provide faster onset, increase patient acceptance, and provide the same or improved pain reduction compared with a 20% benzocaine gel.15,16 Studies are ongoing for this potential future trend.
We have many strategies for pain control and the variety of agents and methods for the use of topical anesthetics have their place and are important among them. Although they do not provide the pulpal or profound anesthesia needed for some procedures, topical anesthetics can be useful prior to injections, during probing, exploring, and for light debridement procedures in the presence of inflammation.
Dental hygienists should never feel pressured to administer topical anesthetics in lieu of injectable local anesthesia when pulpal/profound anesthesia is required for thorough, safe, and comfortable care. If direct supervision is required for provision of local anesthesia by the hygienists, then patients that may require local anesthesia during treatment should not be scheduled when the dentist is not available. Follow the laws for your state. For example; not all states allow RDHs or DAs to administer aerosol topical anesthetics. Nevada is one such example.
It is our ethical responsibility to select the safest agent and delivery method for each individual patient. We must know the relative toxicity of the agents we use and be vigilant about staying up-to-date regarding their use. Consulting product inserts is a good place to start. At increased risk for adverse events are children, medically compromised, and elderly patients.
LAURA J. WEBB, RDH, MS, CDA, is an experienced clinician, educator, and speaker who founded LJW Education Services (ljweduserv.com). She provides educational methodology courses and accreditation consulting services for allied dental education programs and CE courses for clinicians. Laura frequently speaks on the topics of local anesthesia and nonsurgical periodontal instrumentation. She was the recipient of the 2012 ADHA Alfred C. Fones Award. Laura can be contacted at [email protected]
References
1. Bell K. Topical anesthetics for dental hygiene procedures. Dimensions of DH. July 2017;15(7):32,34-35
2. Logothetis D (2017). Local Anesthesia for the Dental Hygienist, 2nd ed. Elsevier
3. Malamed S (2013). Handbook of Local Anesthesia, 6th ed. Elsevier
4. Basset K, DiMarco A, Naughton D (2014). Local Anesthesia for Dental Professionals, 2nd ed Pearson
5. Haveles E B (2015) Applied Pharmacology for the Dental Hygienist, 7th ed. Elsevier
6. Bird D & Robinson D (2018). Modern Dental Assisting, 12th ed. Elsevier
7. Wilkins E (2013) Clinical Practice of the Dental Hygienist, 11th ed. Lippincott Williams & Wilkins
8. https://www.premusa.com/product/hygienepreventative/topicale-gel-pumps/
9. https://www.premusa.com/product/hygienepreventative/topicale-gel-patch/
11. Webb L. “Needleless” intranasal spray: Kovanaze product for local anesthesia makes its debut. 11,12 RDH Mag Oct 2016 Vol 36 No 10
12. Ciancio SSG, Hutcheson MC, Ayoub F, Panera Jr EA, Pantera CT, Garlopo DA, Sobieraj BD, Almubarak SA. Safety and efficacy of a novel nasal spray for maxillary dental anesthesia. J DENT RES July ٢٠١٣ ٩٢: S٤٣-S٤٨, first published on May ٢٠, ٢٠١٣
13. http://cetylite.com/dental/topical-anesthetics
14. Isen D. Non-injectable local anaesthesia in dentistry: a review and case study. Oralhealth. Feb 2013
15. DiMarco AC, Wetmore AO. Clinical comparison: Fast-acting and traditional topical dental anesthetic. Anesth Prog Summer 2016: 63(2):55-61
16. Kosaraju, Vandwalle. A comparison of a refrigerant and a topical anesthetic gel as pre-injection anesthetics. Jan 2009 JADA Vol140
17. http://www.septodontusa.com/sites/default/files/2017-05/Lidocaine%20Ointment-PI.pdf