Finding A Place In Your Heart For Special Smiles
Children with developmental disabilities often miss, among other things, the opportunity to have dental care delivered to them.
Cathleen Terhune Alty, RDH
Statistics say 48 million Americans have special needs: people with developmental disabilities, including mental retardation, autism, epilepsy and cerebral palsy. February is Children`s Dental Health Month, so the focus here is on the 11 million children who are included in this statistic.
Since developmental disabilities are sometimes untreated and even unrecognized, these numbers may be substantially higher. Experts also predict that the special needs population will increase due to:
- Higher survival rates for low birth-weight babies.
- HIV infection.
- The abuse of alcohol, crack or cocaine during pregnancy.
- Emotional problems.
In regards to the latter, epidemiologists report psychological disorders now rank among the most prevalent health conditions of modern childhood.
Special needs in dentistry too
The dental needs of these 11 million children are equally substantial. Genetic disorders can cause congenitally missing or malformed teeth. Malocclusions, including craniofacial or orofacial muscle dysfunctions, abnormal tongue position, and aberrations in growth and development, can contribute to dental problems. Children with disabilities may have higher incidents of orofacial trauma, either accidental or self-inflicted. Sugar-laden medications can cause rampant decay, and some medications may adversely affect oral mucosa. A child with a physical handicap may be dependent on a caregiver or parent for all basic oral hygiene tasks, and the caregiver may not know how to do this.
The sheer magnitude of these statistics and dental problems should indicate that there are many children, as well as adults, with special needs who should be receiving care from the dental profession. Unfortunately, most of them are not finding their way into private practices.
Dr. Steven Perlman, associate clinical professor of pediatric dentistry at Boston University Goldman School of Dental Medicine, is creator of the "Special Athletes, Special Smiles" program. This educational oral health screening and referral program is run in conjunction with Special Olympics in cities nationwide. The program is sponsored by Boston University and Colgate Oral Pharmaceuticals and is affiliated with Oral Health America and the Academy of Dentistry for Persons with Disabilities.
The "Special Athletes, Special Smiles" program is "a unique opportunity for dental professionals to provide care to those patients who are in desperate need, but are often overlooked," according to Dr. Perlman. "People with disabilities, especially those who live in community residences or with their families, often do not receive nor can they afford proper dental care," he explained.
Susann Clifford, RDH, is associate professional relations manager for Colgate Oral Pharmaceuticals in Canton, Mass. She is involved with instructing dental hygienist volunteers and being an on-site consultant during "Special Athletes, Special Smiles" events.
"We are fulfilling a real need with this program," Clifford said. "Access to care is the number one problem we see. Caregivers don`t always know what they need to do to help the person with special needs. Some of the athletes just need some encouragement to do oral care for themselves and some need someone else to actually do the oral care for them. We see the full range."
As a dental hygienist in the corporate world, Clifford sees her position as a way to create and support these kind of programs and facilitate routing information to other dental hygienists.
Special needs experts cite several reasons why these 11 million children are not receiving the dental care they need.
First, dentists and dental hygienists lack training concerning patients with special needs. Dr. Perlman said, "Students are graduating from dental school and dental hygiene school with little or no training in treating patients with special needs. Therefore we can`t expect them to be real comfortable doing it."
Dr. Perlman advocates curriculum changes in dental schools that would provide students with more lecture hours and hands-on care with patients who have special needs.
He refers to a 1993 survey conducted by the Academy of Dentistry for Persons with Disabilities to determine training levels in dentistry for the treatment of people with disabilities. The academy performed the survey at the request of the Joseph P. Kennedy, Jr. Foundation and found:
- Dental schools averaged 12.9 hours in lecture, but 47 percent of the schools reported eight or fewer hours.
- 65 percent of dental schools reported 10 or fewer hours of clinical experience. This represents, on average, fewer than five treatment appointments.
An unpublished but more comprehensive survey done in 1994 of 170 dental hygiene programs revealed that many schools (35 percent) devote only six to 10 didactic hours to special needs training. At only a little more than half of the dental hygiene programs, less than 20 percent of the students receive hands-on, clinical experience with patients who have special needs.
Few dental hygiene schools reported actively recruiting patients with developmental disabilities for their clinical cases. This contrasts sharply with real practice. In October 1995, for example, a survey of dentists and dental hygienists who attended the ADA`s Annual Session showed that, among 692 respondents, 72.5 percent of dentists and 74 percent of hygienists were currently treating patients with special needs. Of those who chose not to treat these patients, the majority refer special needs cases to pediatric dentists.
Almost 83 percent of these dental professionals agree that there needs to be increased attention in dental schools and continuing education courses on how to care for patients with special needs.
Financial and physical barriers
Another problem that exists with the special needs population is inadequate or often non-existent reimbursement for dental care services. Medicaid services, particularly for adults, have been cut in 43 states, according to Dr. Perlman. Government statistics show that 25 percent of individuals with developmental disabilities live with incomes below the poverty level.
A third area involves issues of access: Can the patient with special needs find a dentist who will treat them, regardless of their financial status? Can this patient physically enter the office?
The Americans with Disabilities Act of 1990 was designed to eliminate discrimination against people with disabilities, allowing them access to services and employment without physical barriers, which includes dental offices. Is the office prepared to manage the patient`s special needs with comfort and expertise? Can the staff connect with the patient as a person and not just his or her disability?
Using common sense
Patient management issues are another area that often prevent children with special needs from receiving dental care. The solutions, though, involve common sense more often than special equipment.
Recommended patient management techniques are the same as those used when providing dental services to non-disabled children:
- Use a calming, pleasant, and reassuring voice. Speak to the child appropriately by using simple, direct language, establishing a rapport.
- Use specific, positive reinforcement for all cooperative behavior.
- Recognize the child`s feelings by asking and then listening to their response. Express concern instead of rationalizing or reassuring. (Most young children can`t rationalize and studies indicate reassurances are overused and ineffective.)
- Tell the child what to expect; keep appointments short. Use the "Tell-show-do" concept - tell the child about one task, show them what you will use to perform the task, then perform the task before talking about the next step.
For example, instead of saying, "First, I`ll check your teeth, then I`ll polish and floss," consider saying, "First, I will check your teeth. I will use this mouth mirror. If you look in it, you can see yourself. I will use it to see your teeth better." Then use the mirror. It has been found that a child`s cooperation increases when they know what to expect.
Dolores Yoder, RDH, who works in a pediatric private dental practice in Boston, said, "I never worked with special needs patients until I started here. In the beginning it was not easy. But I got a lot of help from the rest of the office staff and now I feel confident."
Use of local anesthesia when performing restorative dentistry, if given enough time to take effect, can help keep a child comfortable and increase compliance.
Are physical restraints needed?
One area of intense debate regards use of restraints. A committee from the Academy of Dentistry for Persons with Disabilities was formed to study the legal, ethical, and medical considerations on the use of restraints in the delivery of dental care for special needs patients. The committee concluded that although there is "no consensus among the states on the definition of restraint, the current national view is that restraint should only be used when absolutely necessary, and it shall not be used as punishment or for the convenience of the staff. Use of restraint is an acceptable dental practice when appropriately used for behavior control of patients with developmentally disabling conditions."
Physical restraints should cause no physical injury, and documentation and informed consent is required. Restraints can range from a caregiver or family member seated in the dental chair restraining the child with his or her body, mouth props, head, arm and/or leg restraints, Pedi-Wrap blanket, Papoose or Pedi-Board, sedation, and general anesthesia. The use of restraints limits movement and can allow the operator to work in a safer and more efficient manner.
Some dental professionals are not comfortable with the idea of using restraints under any circumstances.
Dr. Perlman said it must be emphasized to the patient and the caregiver granting informed consent that "the restraint is not a punishment but rather a method to help the patient control physical movements."
Kathryn Olson, RDH, dental services coordinator for Swedish American Hospital in Rockford, Ill., finds that treating the dental problems of the patient with special needs who are institutionalized a challenging, but very rewarding, job.
"It is a very challenging task; definitely not traditional hygiene. At the end of the day, I am physically exhausted," Olson said. "There isn`t always easy access and often not much cooperation. We do what we can as long as we can. Our goal is to see improvement each time we see that patient at a recall visit."
Olson is also involved in training the staff to care for the oral health of the patients. Olson said that in-service training helps those who are new to the job and to continually reinforce the information for those who are experienced.
"We always say that daily personal oral hygiene is not a personal issue, like combing a patient`s hair. It`s a medical issue. The total implications of oral disease are far reaching," Olson added.
The role of medical factors
Another area to consider is the lack of medical knowledge of many dental professionals. Children with special needs often have systemic diseases or medication regimens that need to be understood before dental treatment begins. It is important to consult the caregiver and the physician regarding not just the health history but the nature of the disability, its pathophysiology and treatment, and how it may compromise oral health.
Numerous factors may affect oral health in patients with special needs, including orofacial muscle disturbances, craniofacial deformities, neuromuscular control problems, tongue thrusting, ruminating/regurgitating (creating an acidic environment), bruxing, mouth breathing, delayed eruption, retained deciduous teeth, swallowing difficulties, and pouching (holding food in the mouth for long periods of time).
Since many people with disabilities may have a soft diet to make chewing, swallowing, and digestion easier, plaque accumulation can be accelerated. The high sugar content of medications, particularly when given in nighttime doses, can lead to rampant tooth decay. Many caregivers are unaware of the problems associated with extended feedings, particularly when used to quiet a child or help a difficult sleeper fall asleep.
Excessive drooling can cause facial dermatitis and chapping, and a crowded dentition is harder to clean. Children with developmental disabilities may lack coordination, finding it more difficult to clean their own teeth. They may also be more susceptible to falls and other traumatic injuries which require dental care.
By treating children with special needs, we can help improve the child`s self-image and sense of well-being in a very positive way. By training ourselves, we can better understand the nature of each disability and create an individual treatment plan designed to best help the specific needs of the patient with special needs. By educating the patient and their caregivers, they will be able to better maintain oral health at home and understand that oral health is indeed a part of total health.
Cathleen Terhune Alty, RDH, is a contributing editor for RDH and is a member of the Office of Sterilization and Asepsis Procedures Research Foundation.
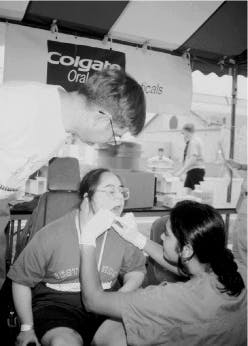
Emily and Jonathan Derr, left, are siblings in Swampscott, Mass., who find much to smile about when visiting the dentist. In photo above, dental hygienists offer instruction on brushing and flossing to children and adults with mental retardation during the 1995 Special Olympics Summer Games.
Volunteer dental professionals conduct oral health screenings for athletes at the Special Athletes/Special Smiles programs sponsored throughout the country last summer.
Wanted: `Great Rewards`
What can you do if the dentist you work with is not interested in helping those with special needs, but you want to? Volunteering may be the answer!
"Don`t be afraid," Kathryn Olson, dental services coordinator for Swedish American Hospital, said, "just do it! I`m no different from anybody else. I had no experience when I started. My dental hygiene education did not include much contact with persons with disabilities, and I`d be lying if I said I wasn`t intimidated at first.
"But I told myself, `I`m a dental hygienist and I can do this!` I`ve never worked anywhere where I`ve been so respected and so fulfilled. Every single dental hygienist has had training in daily oral care. Pick a nursing home or other facility and make it your own. Walk in and say, `I`m a dental hygienist and I want to help.` The rewards are so great that once you start, you`ll never want to stop."
The "Special Athlete, Special Smiles" program welcomes volunteers during Special Olympics programs. Check with your component dental hygiene society to learn what other events or programs need dental professional volunteers.