Making the Connection
Oral health is an integral part of general health and is essential to people’s overall health and well-being. Plaque in the oral cavity can wreak havoc with other parts of the body because of bacteria and the accompanying inflammation.1
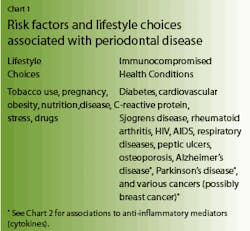
The early identification and treatment of oral disease can play a key role in preventing the progression of periodontal disease, as well as any systemic diseases associated with periodontal disease (see Chart 1).
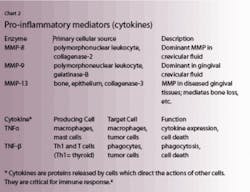
Which came first with regard to disease etiology - oral disease or the systemic disease? Numerous research reports show that inflammation can occur when bacteria, plaque, and biofilm live inside the oral cavity. It has been recognized that blood vessels play a central role in orchestrating the inflammatory and immune processes. When these organisms enter the blood stream, the cells in the blood vessels are activated by cytokines and bacterial lipopolysaccaride and become more adhesive to circulating polymorphonuclear leukocytes (PMNs), T and B lymphocytes, etc. This is what contributes to inflammatory chances in periodontal disease and, most likely, systemically.2
Chart 1 shows diseases and lifestyle choices associated with periodontal disease. Available research results establish that good oral health is important for good systemic health.3
Assessment of risk factors and periodontal disease
Periodontal infections are associated with specific pathogenic bacteria that colonize in the subgingival areas of the oral cavity. Several of these microorganisms - Porphyromonas gingivalis, Actinobacillus actinomycetemcomitans, and Bacteroides forsythus - also invade the periodontal tissues and are considered virulent organisms.5
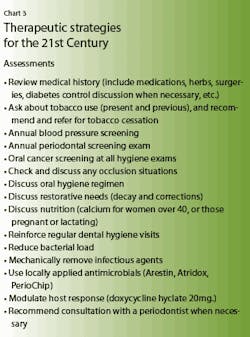
Initially, the bacteria and progression of periodontal disease is clearly modified by local and systemic conditions called risk factors (perio medicine). As health-care providers, it is important that we provide patients with proper assessments each time they visit our treatment room. To do this, it may be necessary to ask detailed questions regarding their health history and current health (see Chart 3)
Assessments
One annual assessment should be a full-mouth periodontal screening exam. Included in this assessment is an evaluation of all the soft tissues: gingival color, texture, probing depths, areas of recession, bleeding points, areas of mobility, and any mucogingival involvement. It is important that these be documented the first time a patient visits the practice and again annually.
Dentists and hygienists can now treat areas of oral infection in the periodontium with various locally applied antimicrobials such as Arestin®, Atridox®, and PerioChip®. Many patients are immunocompromised, use tobacco, make certain lifestyle choices, and have chronic periodontitis. These people are candidates for scaling and root planing procedures, chemotherapeutics, and, most likely, host modulation therapy.
Host modulation
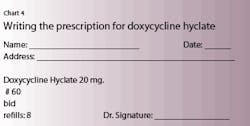
A subantimicrobial dose of doxycycline hyclate (SDD/Periostat®) is an enzyme suppressor now available in generic form from at least five companies. It can be used as an adjunct to definitive scaling and root planing. (see Chart 4)
Strong evidence now supports the use of SDD as an adjunct to non-surgical therapy to manage chronic periodontitis.6 It should be stressed that SDD needs to be considered an adjunct to treatment. Scaling and root planing must be part of the protocol for treatment of chronic periodontitis.7
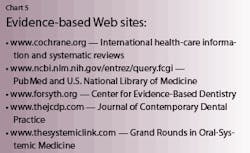
Referral to a primary care physician may be indicated when the medical history states the patient has some of the risk factors mentioned in Chart 1. Dentists, dental hygienists, dental auxiliaries, and all members of the dental team need to keep abreast of the latest research by attending dental conferences and continuing education courses, reading professional journals, and checking the medical and dental Web sites which have evidence-based research documented (See Chart 5)
Thousands of evidence-based research articles document inflammation and the connection between oral and systemic diseases. Current treatment modalities are scientifically proven to improve patients’ health.8 In 1996, the U.S. Surgeon General commissioned the Secretary of Health to research the scientific relationship between oral and systemic health. A document called “Oral Health America” documented that there is scientific evidence between oral health and systemic health.9
Research changes are underway, and we need to keep updated on these changes as they become the standard of care. By attending continuing education courses, reading our dental journals, and seeking information on the evidence-based Web sites, we can remain abreast of all the recent changes which are rapidly occurring.
After making the appropriate assessments, it is important that we sit our patients upright in the dental chair and discuss our findings with them eye to eye. This discussion should include the evidence-based information we have to back up the mouth-body connection. Most patients are likely to listen and take action when they know the truth and the science that backs it up.
A healthy body is not something a person can pay to have, nor is it something easily replaced. Patients need to take responsibility for the health of their bodies. Most people want to be healthy. Each person who comes to your treatment room has a different set of life values, and not everyone will understand the importance of good oral health. It takes a commitment of building lifelong relationships with patients, constant communication, perseverance, and patience to make a change in life values.
Healthy patients equal happy professionals.