Teeth look like ...
Visual impairments represent a challenge to the oral health care educator
BY Giordana F. Tagliareni, RDH, and Dianne L. Sefo, RDH, BA
The World Health Organization has estimated that 285 million people are visually impaired worldwide.1 There are different classifications relating to the degree of visual impairment. According to the International Classification of Disease, there are four levels of visual function: normal vision, moderate visual impairment, severe visual impairment, and blindness. The degree of visual impairment can range from the inability to distinguish dark shadows, images, colors, or even observe large print to complete absence of vision.
Visual impairment can be congenital or acquired throughout life. Congenital eye deficiencies can be caused by a hereditary condition known as retinoblastoma or by medical complications during pregnancy such as rubella.2 Other conditions that may impact vision include albinism, cataracts, glaucoma, or macular degeneration.
-----------------------------------------------------
Additional reading
-----------------------------------------------------
People who are visually impaired may feel as though they are incapable of undertaking normal tasks and may have a harder time acquiring and processing information. Visually impaired children, especially those who are completely blind, are deprived of the opportunity to learn by imitation. An adolescent patient who is visually impaired will require special care and attention, additional motivation, and time for successful interaction.
As a health-care provider, there are many factors to consider when treating a patient with visual impairment. Barriers to accessing proper care for the visually impaired include: transportation, communication, financial status, and culture. Office accessibility is important for all patients, but specifically more so for those who are handicapped. The Americans with Disabilities Act (ADA) ensures equality and prohibits discrimination of people with disabilities. It is important that all offices follow the rules and regulations for the standard of care for the visually impaired. The ADA title II states, "State and local governments are required to follow specific architectural standards in the new construction and alteration of their buildings."3
Some patients may require a wheelchair or a guide dog, and thus, offices should be ready to accommodate these types of situations. The specific criteria for offices include having the proper size, width, and height of the doorways, hallways, restrooms, countertops, and handicap parking spots. It is important to recognize that injuries can be prevented in the office setting by keeping passageways clear of clutter, organizing the workspace, keeping the office well lit, hanging any plants, and avoiding the use of loose rugs. In addition, offices can supply their visually impaired patients with braille or large print maps and signs to help direct them appropriately.
Becoming familiar with the dental office
There are numerous ways to make the dental visit a pleasant experience for a visually impaired child. It may be beneficial to have a pre-appointment visit for these children so they can feel comfortable and focus on the importance of their oral health care. The pre-appointment should consist of familiarizing the child with the layout of the office, filling out paperwork, oral health education, and getting to know the child, including a proper evaluation of his or her degree of blindness. Children tend to become nervous when visiting the dental office, so the pre-appointment should be used to assess the level of anxiety to address their fears appropriately. A discussion regarding expectations from the provider, child, and parent/guardian should be conducted thoroughly.
Another main component of the pre-appointment is to educate the child about his or her teeth. The importance of optimal dental health should be emphasized along with the detrimental effects of plaque and calculus. The discussion should include a thorough understanding of caries initiation and progression so prevention can be fully enforced. Effective communication is the main goal and should incorporate the other senses blind children depend on, such as touch, smell, and hearing. It may be difficult to get the full attention of a child, so an emphasis on detail and imagination is very important.
Supplying the patients with models can help them visualize what is being described by using their sense of touch (see Figure 1). An example would be incorporating different mouth models. One model can depict a healthy dentition and the other can be a dentition that contains calculus (flecks, bumps, grits). This can help the child understand what calculus feels like in order to increase their awareness when evaluating their own oral health.
Americans with Disabilities Act Guidelines for a Barrier-Free Environment | |
External Features | |
Parking | Reserved area, clearly marked, near entrance, 13 feet wide (8-foot car space with 5-foot access aisle) |
Walkways | 3 feet wide for wheelchair accommodation, surface is solid and nonslip, no irregularities, curb ramps (cuts) from the street and from the parking area are necessary |
Entrance | At least one entrance to the building on ground level accessibility by a gentle sloping ramp (rise of 1 inch for every 12 inches) |
An easily grasped handrail (height 30-34 inches) is necessary on at least one side, and preferably both sides to accommodate left- and right-handed cane and one-crutch users | |
Door | Lightweight door with lever type handle opening at least 32 inches for persons using a tall crutch or a wheelchair |
External Features | |
Passageways | At least 3 feet wide, with handrails along the sides |
Passageways free from obstructions, such as hanging signs that a tall blind person could collide with | |
Floors | Level floors with nonslip surfaces are necessary |
Thick or small, unattached movable rugs or carpets present obstacles for wheelchairs or walkers and hazards for a patient with crutches, cane, or leg brace | |
Reception Area | At least part of the furniture will permit easy access during seating and rising |
Chairs with 18-inch-high, flat, firm seats, and arms for support when pushing oneself up by the arms | |
Select chairs that do not slide or tip as the person rises | |
Treatment Room | Space needed for the dental chair, related dental equipment, and the wheelchair |
The dental chair is able to be lowered to 19 inches from the floor and accessible from both sides for wheelchair transfer | |
An X-ray machine in the same treatment room can be used to reduce the problem of moving the patient to a separate radiography room | |
Americans with Disabilities Act, [Internet]. 2010 ADA Standards for Accessible Design. Washington, DC: United States Department of Justice; 2010 Sep 15[cited: 2014 August 12]. Available from: http://www.adagov/2010ADAstandards_index.htm | |
Another component of the pre-appointment is to familiarize the child with the instruments and other dental hygiene aids that will be used during the prophylaxis. This information can ease the child's transition to obtaining dental hygiene care. The sense of smell should be considered by the practitioner to improve the experience. This may be done by having the child smell the different flavors of prophy paste and toothpaste provided by the office. The sense of hearing on the other hand can be inhibiting because the sounds of the dental equipment can be frightening to a child. Therefore, having the child touch and feel the suction tip, air syringe, and prophy cup can help create a more relaxed environment. Furthermore, the use of dark safety glasses can provide comfort to the patient by preventing light sensitivity.4
Figure 2
Visualizing dentistry
Oral clinical findings in a patient who is visually impaired may sometimes differ from one whose sense of vision is intact. This does not mean that a provider should expect to see different anatomical structures, but rather an increase in the severity of risk indicators of oral diseases. Research shows there is potentially poorer oral hygiene and increased severity of gingivitis and periodontitis in the visually impaired population.5
Initial key inflammatory signs indicating dental disease, such as gingivitis and its progression to periodontitis, are often visual. Visually impaired patients have difficulty detecting the cardinal signs of inflammation such as redness, gingival swelling, and recession. When these patients fail to detect bleeding or redness of the gingival tissues at home and do not report it to the dentist, it puts them at a greater risk for disease progression. Other oral conditions visually impaired patients may not be able to distinguish include: early signs of caries, occlusal wear due to bruxism, or linea alba due to cheek biting. It is also common to find increased calculus and plaque accumulation due to inadequate brushing and flossing techniques, as well as lack of oral health knowledge. Children who are blind lack the ability of visual feedback, and therefore may not have the motivation to complete the proper home care. However, there are many ways to improve their oral hygiene and motivate them chairside.
Primary prevention is an ideal objective in preventing disease, predominantly for the visually impaired. It is crucial to emphasize the importance of proper oral home care at an early age, so it can become a normal part of their everyday routine. It may take more time for the child to learn how to properly practice home care. Studies have shown that a longer period of reinforcement can improve the oral hygiene of a visually impaired child.5 Patience, time, and repetition are key components when educating the visually impaired on his or her oral home care.
The health-care provider must not only educate but also motivate. An inability to visualize any improvement in oral hygiene can make it more difficult to establish compliance. Therefore, they must be motivated through other means, such as having them run their tongue across their teeth before and after the prophylaxis. This allows the patient to differentiate between plaque, calculus, and a healthy smile.
Adequate instruction on proper home care must include all essential components of dental hygiene such as brushing, flossing, rinsing, and risk behavioral counseling if needed. Studies have shown that electric toothbrushes or conventional toothbrushes with crisscross bristles are highly effective for plaque removal for visually impaired children.6 There are also numerous types of effective dental floss including dental picks, flavored floss, and special handles (see Figure 2). Finding an oral aid the child likes using will increase the likelihood of the child using it more often.
An effective method for proper flossing is to permit children to demonstrate the technique and advise them to listen for the "squeak noise."4 This type of feedback will help the visually impaired child access all surfaces in addition to reaching the base of the gingival sulcus. An adjunct to brushing and flossing in caries prevention is the supplementation of a fluoride mouth rinse and fluoride-containing dentifrice, which come in a variety of flavors.
Depending on the child's oral status, risk behavioral counseling, such as nutritional guidance, can also be highly beneficial. Children have been shown to prefer foods and beverages with high sugar content regardless of disability. It is important to educate the child and parent on healthy food alternatives and to emphasize the role of time of exposure in the initiation of the caries process. A constant exposure to fermentable carbohydrates facilitates an acidic environment favorable to caries initiation and progression. Effective home care instruction involves a thorough discussion with the parent or guardian. The discussion should emphasize the importance of positive reinforcement at home.7
Audio instructions are another valuable way for children to develop a proper home maintenance protocol at their own pace. Listening to their favorite song lasting at least two minutes can help encourage brushing for an adequate amount of time. Finally, when dismissing the child, include the distribution of written oral hygiene instructions in large print or braille, as per the degree of visual impairment.
The most rewarding feeling as a dental hygienist is when the patient leaves the office with a smile that runs from ear to ear. Caring for a patient with visual impairment can be challenging but rewarding. Time, patience, and motivation are the three most important factors when treating these patients. There is a variety of techniques and skills that can help make a dental visit a good experience, especially for children. Every encounter can be a learning experience for both the patient and the provider as they grow to establish a strong, trusting relationship.
Outreach with the visually impaired
During my last year in the dental hygiene program at New York University College of Dentistry (NYUCD), I was given an assignment to complete an educational outreach. The objectives and goals were to educate a group about the importance of oral health. Many students chose nursing homes, preschools, elementary schools, and high schools. I knew immediately that I wanted to focus on a group that involved children, but I wanted to do something different. My dad has worked at an institute for visually impaired children for many years. He always speaks highly of the children and tells me stories of how sweet and spectacular they are. I decided to check out the school and see if they would grant me permission to make a presentation to a group of students.
When I contacted the school, they were thrilled to have me present. They were helpful in setting up a date, time, room layout, and group. At first I inquired about presenting to the kindergartners and first graders. The assistant principal told me the younger groups already received an oral hygiene presentation and asked if I was interested in working with the sixth and seventh graders, since they had not yet had the opportunity to participate in an oral hygiene presentation. I immediately said yes.
Although I was thrilled to have this opportunity to work with the visually impaired children, I was nervous in working with this age group. The older children can be more difficult to please and grab their attention. I had to think of a completely different presentation due to the change in age. I not only had to consider that they were visually impaired, but also that they were in the preteen age. I thought about what they would be interested in, and a few thoughts came to mind. I knew that I would use all other senses to make the presentation fun and educational.
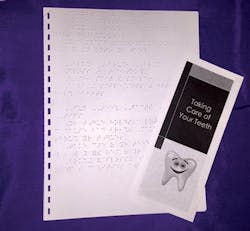
To grab their attention through sense of hearing, I searched for videos and came across a fun, yet informative video about dental caries. For senses of touch, smell, and taste I decided to include study models of the mouth, fruit scented floss, and two flavors of toothpaste. I also prepared a pamphlet for the children and gratefully had the opportunity for them to be printed in braille and large print (see Figure 3). This was done for the children with different degrees of visual impairment. For the end of the presentation I arranged goodie bags that supplied them with a toothbrush, floss, and toothpaste.
On the day of the outreach, I was excited, but also very nervous. This was not an experience that I was used to. I hadn't had many opportunities working with visually impaired children. I was nervous that I would say something like "Do you see this?" I was also nervous that the presentation would not grab the children's attention and they would not enjoy it. When I arrived at the school, the assistant principal came to greet me and brought me to the classroom. When I entered the room, there were desks grouped together, a big projector screen with speakers up front, a desk for the teacher, and 15 children. They were all surrounding the desks in the front and seemed excited for the presentation. My nerves then settled down as I realized that they were just like other children.
I began by speaking to them about the importance of oral health and home care. After the video, I grouped the children into three groups and allowed each child to use a mouth study model to practice flossing and brushing of the teeth. I also gave each child the opportunity to smell and taste a very small amount of two different flavors of toothpaste, which were mint and bubblegum. They had the options to use fruit flavored and scented string floss and floss picks. The presentation went extremely well and the children were very intrigued and asked many questions. They were bubbly and excited to learn more about their teeth.
The outreach assignment inspired me to continue researching about dental hygiene considerations for visually impaired patients. Throughout my research I learned new techniques and ideas that helped me become a better clinician in treating this population of patients. I decided I wanted to share all this information in effort to increase the awareness of caring for visually impaired patients with all other registered dental hygienists. I am very pleased to have had this wonderful opportunity and look forward to working with this institute again each year as I bring future students of NYUCD for outreach. RDH
Giordana F. Tagliareni, RDH, graduated from New York University in 2014. She is currently employed as a part-time registered dental hygienist while fulfilling her academic requirements to obtain a bachelor's degree in dental hygiene. Giordana's passion for quality care has led to her direct involvement in raising awareness through community outreach, placing an emphasis on the importance of proper oral hygiene. She can be reached at [email protected].
Dianne L. Sefo, RDH, BA, is a clinical instructor and preclinical coordinator at New York University. She participates in didactic and clinical dental hygiene education. Dianne has previously worked as a dental hygiene educator at Monroe Community College and Concorde Career College - San Diego. She has also held positions at various private practices in New York and southern California. In addition to her teaching and clinical work, she has contributed to various publications pertaining to the advancement of the standard of care in evidence-based dental hygiene therapy.
References
1. World Health Organization. Visual impairment and blindness. Available at: http://www.who.int/mediacentre/factsheets/fs282/en/. Accessed July 29, 2014.
2. National Federation of the Blind. Common Eye Conditions and Causes of Blindness in the United States. Available at: https://nfb.org/images/nfb/publications/books/books1/ifblnd10.htm. Accessed July 29, 2014.
3. Safety Net Dental Clinic Manual. Facilities and Staffing. Available at: http://www.dentalclinicmanual.com/chapt2/1_10.html. Accessed July 29, 2014.
4. Jaccarino J. Vision impairment: treating the special needs patient with a sensory disability: patients' loss of vision need not impede their dental care. Available at: http://www.thefreelibrary.com/Vision impairment: treating the special needs patient with a sensory...-a0207643087. Accessed July 29, 2014.
5. Shetty V, Hegde AM, Varghese E. A novel music based tooth brushing system for blind children. J Clin Pediatr Dent. 2013 Spring;37(3):251-5.
6. Sharma A, Arora R, Kenchappa M, Bhayya DP, Singh D. Clinical evaluation of the plaque-removing ability of four different toothbrushes in visually impaired children. Oral Health Prev Dent. 2012;10(3):219-24.
7. Hebbal M, Ankola AV. Development of a new technique (ATP) for training visually impaired children in oral hygiene maintenance. Eur Arch Paediatr Dent. 2012 Oct;13(5):244-7.