Achondroplasia: Oral health concerns associated with genetic disorder commonly referred to as dwarfism
Oral health concerns associated with genetic disorder commonly referred to as dwarfism
BY Jennifer S. Sherry, RDH, MSEd, and Sophia Aponte, RDH, BSDH
The overall goal of this article is to provide the reader with information on the signs and symptoms of achondroplasia by providing physical pictures (photographs and radiographs) and information from a patient with achondroplasia. It is hopeful that readers will be able to:
• Identify the physical conditions associated with achondroplasia.
• Explain the daily limitations of persons with achondroplasia and the care modifications incorporated in daily activity.
• Recognize the oral complications and manifestations of patients with achondroplasia.
• Describe the dental management for patients with achondroplasia.
Many hereditary and/or developmental disturbances manifest in the oral cavity. It is prudent for dental hygienists to be knowledgeable about such disturbances in order to provide optimum oral health services for all patients.
Achondroplasia, or dwarfism, is a hereditary skeletal disorder characterized by failure of normal conversion of cartilage into bone that begins during fetal life. It is also known as chondrodystrophia fetalis, a nonlethal form of chondrodysplasia,1,2 which is a rare congenital disease predominately affecting the long bones of the body.3 Achondroplasia affects about one in 20,000 babies or one in every 40,000 children internationally. Approximately 150,000 persons have achondroplasia worldwide.4 There are more than 10,000 individuals living with achondroplasia in the United States (equal frequency in men and women and across all racial and ethnic groups) making it the most common skeletal dysplasia.4
------------------------------------------------------
Other articles to read
- It makes a difference to me: The oral health of special needs children prompts hygienist to develop school-based program
- The world of autism: Treating patients with autism can be very rewarding for the dental hygienist
- Access stats don't lie: Students experience the challenges of a public health project for kids
------------------------------------------------------
It is inherited as an autosomal dominant trait; however, 80% of the cases are sporadic.5 There is a defect in the mutation of chondrocytes in the cartilage growth plate, which enables abnormal cartilage growth-plate differentiation and insufficient bony development.5 Most cases of achondroplasia are from an autosomal dominant inherited fibroblast growth factor receptor-3 (FGFR3) gene, which has mutated.3 The gene for achondroplasia is fully penetrant, meaning everyone who possessed it has the disorder. In only about an eighth of cases is the gene inherited from a parent who has achondroplasia; about seven-eighths of cases are due to a new mutation (a new change in the gene). The chance of a new mutation rises with the age of the father, and new cases were more often last-born (rather than first-born) children.6
Most children do not have achondroplastic parents, but they can still transmit the gene to their children, and the risk for passing that gene to a child is 50% in each pregnancy.6 When both parents have achondroplasia, in every pregnancy, there is a one in four (25%) chance their child will inherit the faulty FGFR3 gene copy from both parents. The impact of having no working FGFR3 protein produced means these children usually do not survive.5
Skeletal dysplasias are usually characterized by short stature, which may be proportionate or disproportionate. Some parts of the body may grow at a normal rate while other parts have a reduced growth rate. The cartilage cells in the baby develop into bone more slowly than normal.5
Achondroplasia is usually diagnosed at birth, and typical clinical manifestations include disproportionate short stature with normal trunk length, rhizomelic (proximal) shortening of the extremities, bowing of the lower extremities, short, stubby trident hands (increased space between the third and the fourth fingers), and spinal stenosis and lumbar lordosis (curved lower spine). Craniofacial characteristics of this disorder include macrocephaly (enlarged head), prominent forehead, depressed nasal bridge, maxillary hypoplasia, otolaryngeal system dysfunction, and foramen magnum stenosis.7 Associated comorbidities include clubbed feet, hydrocephalus, otitis media (which leads to hearing loss), and adenotonsillar hypertrophy (that involves upper airway obstruction).3 The average adult height of achondroplasia patients is approximately four feet for men and women.8
Hydrocephalus is considered a congenital disease affecting the central nervous system and is characterized by accumulation of cerebrospinal fluid in the lateral ventricles of the brain, causing progressive ventricular dilatation. Hydrocephalus is concerning due to the chronological changes in the eruption of teeth, changes in occlusion, greater accumulation of plaque, and a higher caries prevalence. Regular dental visits are needed to control caries as well as to educate the caregivers regarding oral hygiene needs for children with hydrocephalus. In addition, the dental practitioner needs to be aware of the danger of placing pressure on the ventricular-peritoneal drainage tube during dental treatment.9
Typical radiological features of achondroplasia include shortening of the tubular bones, narrow interpediculate distance in the lumbar vertebra, short vertebral pedicles, and decreased size of the skull base, as well as other alterations in bone development.10 These characteristics may lead to a number of complications including hydrocephalus, sleep apnea, upper-airway obstruction, otitis media, sinusitis, and dental malocclusion.11,12
Figure 1: Patient Q, full face photo
Figure 2: Patient Q, ultrasound
Figure 3: Patient Q, current back view
Figure 4: Patient Q, trident right hand
Some manifestations of achondroplasia can be systemic such as obesity, diabetes, cardiovascular disease, and asthma.13 Obesity can occur due to the decrease in physical activity, the persistence of an age-related appetite, and psychological weakness. Diabetes can be associated because of the obesity tendency, which can place an increase on insulin production. Sleep apnea can be caused by a multitude of issues such as brain stem/spinal cord compression, and later, due to midfacial hypoplasia, leading to a narrow upper airway.14 Also, skeletal issues are prominent such as degenerative joint disease, osteoarthritis, and excessive wear to cartilaginous surfaces. Some other concerns are with foramen magnum stenosis, lumbar stenosis (which can play a part in incontinence) and thoracic deformities (which may cause restrictive lung disease).3 Spinal difficulties and backaches occur in late childhood and midadolescence.13,15
Oral manifestations may include Class III malocclusion, although mandibular growth is not affected. Typically, there is no delay in the eruption sequence of primary or permanent teeth. However, due to the jaw structure and small stature, teeth are sometimes larger than the jaw can support. Patients with achondroplasia are somewhat prone to gingivitis and periodontal disease due to the makeup of the bone structure as well as the mouth breathing tendency.16 If children require general anesthesia for dental work, there may be concern with enlarged adenoids or small nasal pharynxes and larynxes causing difficulty for the anesthesia to be successful.17
There is no cure for this condition; however, extended limb lengthening has been used to improve stature.17 Most individuals with achondroplasia are of normal intelligence and are able to lead independent and productive lives.8
CASE STUDY
Patient Q, an 8-year-old Caucasian female, presented for oral health services at a Midwestern University dental hygiene program clinic (see Figure 1). Her medical history was investigated early in her life because of suspicions of achondroplasia (dwarfism). At the time of birth, Patient Q's mother had genetic testing done that did not indicate a genetic link to achondroplasia, nor did the father's family tree indicate any family members with this condition (see Figure 2).
However, Patient Q's family history did show diabetes, vision impairment, heart disease, and birth defects on the mother's side, and asthma on the mother's and father's sides. Patient Q's mother stated that at birth, she was a "fresh mutation," meaning that it was not inherited from either parent or extended family. Patient Q's mother stated that at birth, she had a frog hipped/frog legged appearance with a red tinge to her skin. The characteristics present at birth led to several tests, determining the disorder was achondroplasia. The disorder was diagnosed two days after birth with X-rays, bloodwork, and genetic testing.
Dental History and Oral Assessment
Intraoral and occlusion/oral habits assessment for Patient Q resulted in the following observations:
Head and neck examination
- Larger than normal head circumference
- Asymmetry of forehead was bulbous and protrusive (referred to in pathology as frontal bossing)
- Button nose
- Slight chapping of lips
- Hard palate was vaulted and narrow
Occlusion
- Molar and cuspids right and left: Class I occlusion (see Figure 5)
- Overbite 4 mm
- Overjet 3 mm
- Slight crowding No. 22 and No. 26 (see Figure 6)
- Crossbite No. 10
- Midline 1 mm shift to left
- Profile is mesognathic (see Figure 7)
Visual Assessment
Patient Q had tendency to have bruxism and clenching of teeth (see Figure 8). This was visible on occlusal/incisal surfaces of teeth K, L, M, R, S, T, B, C, H, and I (see Figure 7). She also exhibited evidence of mouth breathing. There was inflammation on the maxillary and mandibular anterior facial and lingual surfaces (see Figure 8).
Periodontal Assessment
The probing depths were all within normal limits (3 mm or under). No bleeding, recession, or mobility was noted at this time.
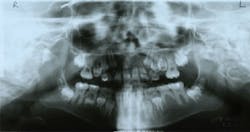
Radiographic Oral Assessment
- Panoramic radiograph (see Figure 9)
- Mandibular right deviation was 1 mm to the left
- Right condyle had a thin, flat appearance
- "Deciduous" teeth present: B, C, H, I, K, L, M, R, S, and T, and permanent teeth present: Nos. 3, 7-10, 14-19, 23-26, and 30
- Slight crowding mandibular anterior teeth
- Small jaw structure on maxilla and mandibular arches (larger permanent teeth than space will allow)
- No. 20 is congenitally missing
- Unerupted teeth: Nos. 1, 2, 4-6, 11-13, 15-18, 21, 22, 27-29, 31, and 32
- Slight deviation of nasal septum
- Normal trabeculation pattern on mandible
- Premature shedding of teeth A and J
- Slight localized horizontal bone loss
- Maxillary sinus was slightly congested (smaller and cloudy on the panoramic radiograph)
Figure 5: Patient Q, occlusion
Figure 6: Patient Q, mandibular anterior crowding
Figure 7: Patient Q, side profile
Figure 8: Patient Q, mouth breathing and inflammation
Figure 9: Patient Q, panoramic radiograph
Figure 10: Patient Q, left side full view
At three months old, an intracranial ultrasound of the head proved unremarkable. There was no evidence of hydrocephalus and no atrophy. Patient Q was diagnosed with pneumonia. Albuterol nebulizer and breathing treatment were given to assist with breathing difficulty. At seven months old, she was in the 50th percentile with weight and head circumference, and she was considered short at 21 ¼ inches long. At this stage, the patient's mother had to use a special infant seat that was supportive of her head and neck due to uncontrollable head movements.
Around one year of age, she was diagnosed with sleep apnea and plagiocephaly (flattening of one side of the skull), which included wearing a plastic helmet for molding the skull. Furthermore, she had hip X-rays that did not show hip dislocation but did reveal hip dysplasia. X-rays of the upper extremities documented facial deformity and that both humeri (arms) were shortened. Radius and ulna had a normal appearance at this time. At 18 months of age, Patient Q began walking and was fairly unstable. She had a degree of scoliosis or curvature of the spine (44 degree curve) at this time. This is very obvious in current pictures of Patient Q as well (see Figure 3). The ligaments in the body lacked elasticity and her joints had hypermobility, which, in turn, affected her care and stability. She would tend to go down the stairs on her hands and knees due to disproportionate height of steps, in comparison to her limbs and trunk.
At age two, Patient Q experienced delayed speech development and was at risk for dental malocclusions, vision impairment, and strabismus (eyes do not line up in the same direction, therefore, do not look at the same object at the same time). Furthermore, in earlier stages of development, Patient Q was at risk for conductive hearing loss due to frequent otitis media. Bowed legs and kyphosis (curving of the spine that causes a bowing or rounding of the back) were starting to occur during this time. Patient Q had bilateral tubes placed in her ears. A physiological exam revealed Patient Q's length was 27.165 in (less than third percentile); weight was 9.75 kg (fifth to 10th percentile for age); head circumference was 48 cm (90th percentile for age); and she had a regular heartbeat.
Patient Q has trident hands (see Figure 4), lower-set ears, curvature of the spine (disk T7-T11), short, bowed legs, hip dysplasia, depressed nasal bridge, button nose, eyes located farther apart, loose muscle tone, small jaw, smaller spinal cord (currently), severe sinus problems (nebulizer used for sinuses and breathing), and chronic ear infections (has had tubes in the past).
Several assessment findings from Patient Q's dental and medical histories, oral assessment, and radiographic assessment (see related sidebar) parallel the characteristics seen in patients with achondroplasia (see Figure 10). The large head circumference and asymmetry of the forehead are indicative of this condition and are very common. The hard palate and jaw structure were small and narrow. The patient had a bilateral crossbite and crowding in the lower anterior region. The permanent teeth that will be erupting in the near future are too large to fit in her actual jaw structure. Orthodontics will be indicated and possibly extractions of teeth will make room for the permanent teeth to erupt. However, Patient Q did not exhibit the typical Class III occlusion as can be observed in the attached profile photos.
Since Patient Q had hydrocephalus as a young child, some health concerns are obvious in this patient. This patient does have midfacial hypoplasia, and this leads to the narrowing of the nasal airways and obstructive sleep apnea, which her mother did discuss. Furthermore, Patient Q still has issues with breathing and asthma. Patient Q has issues with her ears and had enlarged tonsillar areas as a young child. She has difficulty with speech and possible hearing loss due to the items mentioned above. Another medical concern is the possibility of heart disease related to obesity and difficulty with daily exercise. Patients usually have a difficult time exercising due to the short stature and joint issues.
Other assessment findings that are common in patients with achondroplasia are inflammation of the gingiva (due to mouth breathing), chronic sinus and ear infections, and bruxism causing occlusal wear. All of these are evident in Patient Q. In the near future, an adaptive night guard or another appliance may be indicated to minimize attrition and grinding.
On the panoramic radiograph, there was a slight deviation in the nasal septum. This will affect the patient's breathing and complicate her asthma and sinus difficulty. Oxygen or breathing machines may need to be utilized to assist with airway issues.
Implications for Dental Professionals
Dentists and other oral health professionals should be aware of the clinical characteristics of achondroplasia and the complications that may arise as a result of this genetic disorder.14
It is imperative to consider the accommodations needed for dental patients with achondroplasia. The office should evaluate the height of the front desk, office area, and restroom facilities, as well as the operatory accessibility. The dental office may need to have a stepstool or mobile stairs that would assist the patient with all aspects of dental care. Also, items such as doorknob extenders and lower light switches are important to install in the dental office.17
Another possible way to help patients with achondroplasia is providing neck and back lumbar supports for the weak muscles in the neck and/or back. The dental chair may be equipped with a strap or a shoulder harness that will assist the patient to stay positioned and secure.17
Secondary to this condition, there are possibilities of having sleep apnea or breathing difficulties. These conditions can affect the gingival tissue and lead to inflammation, plaque and calculus accumulation, and periodontal disease. Moreover, there are situations of malocclusion due to crowding, and children with achondroplasia need to be monitored by an orthodontist to assist with spacing, occlusal interferences, and difficulty with speech.
Patients with achondroplasia will be prone to ear infections (otitis media), so it is important for the dental professional to speak clearly with their masks removed so that patients can understand instructions.
Special toothbrushes and floss handles will be imperative due to the trident hands and webbed fingers. Make sure the patient and caregiver are familiar with the equipment and instructions for use. Fluoride gel, paste, or rinses may assist with keeping decay to a minimum as well as dietary analysis and assessment for the entire family unit. Family support and understanding is an important piece of the puzzle due to psychological and social issues as evidenced in the case study.
Achondroplasia is a condition of particular interest to the dental community as the general and oral manifestations are significant in the delivery of care. This case study not only provides vital information about the typical conditions of achondroplasia, but it also provides a perspective on people that live with achondroplasia on a daily basis. Despite the physical abnormalities, which set them apart from the rest of the world, they are more than capable of living long and independent lives with optimal oral health. RDH
Jennifer S. Sherry, RDH, MSEd, is an associate professor in the dental hygiene program at Southern Illinois University, Carbondale, IL. She teaches radiology (lecture and lab), third year clinic, and community oral health and the community practicum course. Her research interests include children's health issues and school nutrition programs.
Sophia Aponte, RDH, BSDH. is a 2015 graduate of the Southern Illinois University Dental Hygiene Program, Carbondale, IL. While in school, she participated in many community service projects, including a week-long mission trip to Mexico to provide dental services. She also worked in the Community Dental Center at SIUC, which is a clinic that provides dental services to patients covered by Medicaid,or who are uninsured.
References
1. Jones K. Smith's recognizable patterns of human malformation. 4th ed. Philadelphia, PA: WB Saunders, 1988.
2. Gorlin R, Cohen M, Levin L. Syndromes of the head and neck, 3rd ed. New York: Oxford University Press, 1990.
3. Richardson N. Achondroplasia. Physiopedia. 1-8. Available at: www.physio-pedia.com/Achondroplasia. Accessed April 30, 2014.
4. Gollust S. Living with achondroplasia in an average sized world: An assessment of quality of life. American Journal of Medical Genetics. 2003; 120A: 447-458.
5. Rousseau F, Bonaventure J, Legeai-Mallet L, Pelet A, Rozet J, Maroteaux P, Le Merrer M, Munnich A. 1994. Mutations in the gene encoding growth factor receptor-3 in achondroplasia. Nature 371, 252-254.
6. Stoppler M, Perlstein D. 2014. Achondroplasia. 1-2. Available at: http://www.medicinenet.com/script/main/art.asp?articlekey=256. Accessed April 30, 2014.
7. Shirley E, Ain M. Achondroplasia: manifestations and treatment. J.Am. Acad. Orthop. Surg. 17, 231-241. 2009
8. Trotter T. Health supervision for children with achondroplasia. Pediatrics. 2005; 116; 771.
9. De Morais Gallarreta F. Bernardotti F, DeFreitas A, DeQueiroz A, Faria G. 2010. Characteristics of individuals with hydrocephalus and their dental care needs. Special Care in Dentistry. 30: 72-76.
10. Arita E. Assessment of osteoporotic alterations in achondroplastic patients: a case series. Clin Rheumatol. 2013; 32: 399-402.
11. Steinbok P, Hall J, Flodmark O. 1989. Hydrocephalus in achondroplasia: the possible role of intracranial venous hypertension. J. Neurosurg. 71, 42-48.
12. Hunter A, Bankier A, Rogers J, Sillence D, Scott C. 1998. Medical complications of achondroplasia: a multicenter patient review. J. Med. Genet. 35, 705-712.
13. Al-Saleem A, Al-Jobair A. 2010. Achondroplasia: Craniofacial manifestations and considerations in dental management. The Saudi Dental Journal. 22, 195-199.
14. Baujat G, Legeai-Mallet L, Finidori G, Cormier-Daire V, Le Merrer M. 2008. Achondroplasia. Best Practice & Research Clinical Rheumatology. 22 (1): 3-18.
15. Hecht J, Butler I. 1990. Neurologic morbidity associated with achondroplasia. J. Child Neurol. 5, 84-97.
16. Steven L, Holmes H, Roberts T, Fieggen K, Beighton P. 2005.Orthodontic management of achondroplasia in South Africa. SAMJ. 95(8), 1.
17. Aldegheri R, Dall'Oca C, 2001. Limb lengthening in short stature patients. J. Pediatr. Orthop. 10, 238-247.