Getting off caries infection bus: A treatment plan steers college student back to good oral health
by Patti DiGangi, RDH, BS
A peek into a college student's garbage can reveal clues about deteriorating oral health, but energy drinks, for example, shouldn't be the only consideration.
Kelly is a 20-year-old patient of record you've been seeing since she was a child. She went away to college and, when she came back for her overdue recare appointment, her mouth had changed. However, you know Kelly well and can connect with her. Although she had no history of caries infections, she tells you she hass noticed white spots and her teeth are sensitive to cold. She shares that school has been more challenging than she expected, so she's drinking more coffee and now knows why so many of her friends drink energy beverages. She also mentions that on the weekends, adding a little vodka to the energy drinks helps her get more studying done.
Kelly has never been on the caries infection bus, and you want to stop her from climbing aboard.
Although the energy drinks and junk food might seem to be the obvious red flags, caries infections are not single-faceted problems. This situation is the type of opportunity where dental hygienists can excel. As much as the first reaction might be to act like a parent, a better strategy is to become Kelly's oral health coach. Oral health coaching is a "show" strategy versus a "tell" strategy. It takes innate hygiene excellence to new levels of engagement by using new tools and technologies.
In-office risk assessment
Not all patients are at equal risk, whether for heart disease, diabetes, or caries infections. Risks change, as they did for Kelly. But for the most part, dentistry continues to address caries infections as an acute surgical problem that requires repair. While the restorative procedure repairs the structure, it does not treat the underlying disease. If current and new risk factors are not recognized and addressed, the disease continues. Something more effective is needed for Kelly.
One way for her to understand the various factors that are creating her risks is to use an inexpensive app called MyCAMBRA (mycambra.com). This app is not for Kelly as much as for you to open a dialogue with her. It uses the three traffic light colors to help patients visualize their risks.
Another idea occurs to you when you notice immediately that Kelly's teeth are more plaque-laden than when you last saw her. She says she forgot to bring her power brush charger to school so she used a manual brush. To show Kelly the changes in her mouth, you use GC Tri Plaque ID Gel disclosing gel (gcamerica.com). As with other two-tone products, old plaque shows as blue and new plaque shows as pink. While this is good information that Kelly can see and you can photograph, what makes this product different is that the color turns light blue. This means the pH of the light blue area is <4.5. After seeing this and getting a quick review of pH, Kelly is stunned by what she is seeing.
Testing Kelly's saliva will help create her in-office and home treatment plans. Saliva-Check Buffer, a saliva-testing examination tool (gcamerica.com), identifies, measures, and assesses saliva condition. It tests hydration, salivary consistency, resting saliva pH, stimulated saliva flow, stimulated saliva pH, and saliva buffering capacity. These are all important risk factors in Kelly's ability to fight the damage of caries infection. She can clearly see what is happening.
Traditional radiographic images are also in order, but not bitewings only. Based on her change in health, you decide to take a full series. Of course, Kelly can't read these images and unfortunately it takes 40% to 65% demineralization for anything to appear on the image.
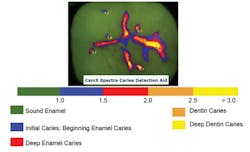
Another way for you to measure what's going on is to use fluorescence technology. An example is the CamX Spectra (airtechniques.com), a caries infection detection system that uses light-emitting diodes to project high-energy, violet-blue light of 405 nm onto the tooth surface. Light at this wavelength stimulates porphyrins, the special metabolites of cariogenic bacteria, to fluoresce red, and healthy enamel to fluoresce green. Along with the colors, a numeric reading defines potential caries infection activity on a scale of zero to five. The color differences and numeric scores should make things real for Kelly.
Kelly's diagnosis
Kelly's CamX Spectra readings on her second molars are in the blue-red zone, registering 1.5 to 2 on the occlusals. Her first molars are in the red zone with a reading of 2.0. White spots are evident at the gingival margins of both maxillary and mandibular cuspids and bicuspids and are in the blue zone with 1 to 1.5 readings.
Kelly is clearly at very high risk, and now she sees it too. She asks what she can do to change it. Wow, isn't that wonderful? It looks like oral health coaching "show" versus "tell" is working already. Kelly wants to make a difference, but she still needs your professional assistance with the in-office and at-home plans.
The traditional drill-and-fill options would be to treat all first and second molars with restorations. Though Kelly seems to have experienced a measurable quick decline, a couple of questions should be asked:
- If these risk assessment systems had been used before, would something have shown up earlier?
- Does is make sense to create larger holes to complete the restoration?
- Should the enamel be etched to protect it?
- Can minimal intervention treatment be less invasive and more effective in the long run?
Kelly's in-office treatment plan
Kelly's minimal intervention treatment plan based on her risk includes fluoride, sealants, protective restorations, desensitizing, and products for home. GC America has long been a leader in minimal intervention (MI) dentistry.
The first change means rather than automatically scaling and polishing Kelly, it makes sense based on her risk to do something different. Kelly needs her oral environment stabilized. This might begin with applying GC Fuji Triage glass ionomer sealants to all her molars. There are many reasons to do this. Most resin sealants require the use of an etchant to prepare the tooth surface. What is that etchant doing? Breaking down the enamel, and GC Fuji Triage needs no etchant. The challenge of placing multiple sealants for hygienists is keeping the field dry. GC Fuji Triage is moisture-friendly. It has self-bonding ion exchange, and high fluoride release creates a strong, acid-resistant, chemically-fused layer that continues to offer protection to the occlusal surfaces.
GC Fuji Triage is more than just a sealant barrier; the advanced fluoride protection offers protection from secondary caries. The key is to prevent noncarious lesions from progressing to cavitation. GC Fuji Triage has the highest fluoride release of any glass ionomer or resin and can be recharged when someone uses a fluoridated rinse or dentifrice.1
This is a great start, but Kelly has more issues with her white spots and sensitivity. MI Varnish™ is the wisest clinical choice for her because it is the only fluoride varnish that contains Recaldent (CPP-ACP), a formulation of bio-available calcium, phosphate, and fluoride. In Kelly's oral cavity, CPP binds to the oral surfaces, including teeth, dentin, oral mucosa, and biofilm. Calcium and phosphate ions are the building blocks for healthy teeth, and MI Varnish delivers bioavailable calcium and phosphate ions into the saliva. MI Varnish will treat Kelly's sensitivity, provide bioactive calcium and phosphate, and will recharge the Triage sealants. In addition, as noted by the American Academy of Pediatric Dentistry (AAPD), varnishes are effective in caries prevention.2
Kelly's at-home treatment plan
Nearly every hygiene professional says, "The most important part of what we do is education." As oral health coaches, this is a "show" process, not just "tell." Kelly's at-home plan needs to be a continued "show" for her. Kelly understands her issues, yet like many of us, her oral health is not always her top priority. Reinforcement of the lessons will help. This can be as simple as giving Kelly copies of the photographs taken and a copy of the CamX Spectra readings.
Or it can be as active as Kelly seeing her pH changes. She can measure what happens when she specifically works to change her pH. pH2OH (ph2oh.com) is a free new app by AT Stills University (ATSU) that patients can download. The office can supply the pH paper. (GC America, in collaboration with ATSU, has put together small and inexpensive pH packets to distribute to patients.) Once patients have the app and pH paper, they expectorate into a small cup and then dip in the pH strip. They then launch the app and hold their smartphone over the paper. The app will read and graph the results.
Patients will be able to measure and see what's happening in their mouths for themselves. Suggest that they take their pH readings after drinking coffee or an energy drink and after eating. In Kelly's case, she already understands a lot about resting and stimulated pH from the Saliva-Check Buffer test you performed at the office. This measure will show her the results of her choices at the moment she makes them rather than long after the fact.
Kelly's at-home treatment should include MI Paste Plus due to the way Recaldent works. An acid challenge will release the calcium and phosphate ions that will buffer the saliva pH to neutral (6.5 to 7.4) and provide these ions in a bioactive form. CPP-ACP is released during acid challenges, raising the oral pH to 7. MI Paste Plus includes the addition of 900 ppm fluoride-forming calcium phosphate fluoride, CPP-ACFP. This will further recharge Kelly's glass ionomer sealants. She can use MI Paste Plus when she sees her pH drop, and she can keep it at her bedside if she wakes up with dry mouth. Kelly can use it several times a day, so this is a win-win all the way around.
Off the caries infection bus?
This all sounds great, and it's not really that far from what we do successfully every day. What are the measures of success? That is the real beauty of MI dentistry-we can measure the success of in-office treatment and Kelly's home-care treatment by using the same risk assessment measures. Successful oral health coaching is not just absence of disease; it's reduction of risk.
If Kelly is still on the caries infection bus, we have the opportunity to change tactics. As an oral health coach, instantly blaming Kelly for noncompliance is not a good idea. There might be factors we missed, such as whom is Kelly kissing? Hygiene excellence, like risk, is not the same for everyone and it changes over time. RDH
Patti DiGangi, RDH, BS, is a certified health information technology trainer shaping the changes in our interoperable electronic health record world. Patti is an ADA Evidence Based Champion and holds publishing and speaking licenses for "Current Dental Terminology" (ADA) and SNODENT Coding. She is the author of the DentalCodeology series of bite-size books for busy people. Patti was awarded the 2014 Sunstar Award of Distinction and the 2013 Sonicare Mentor of Distinction award. Visit DentalCodeology.com for more information about her books.
References
1. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4336652/
2. AAPD Guideline-Reference Manual V37/No. 6 15/16 http://www.aapd.org/media/policies_guidelines/g_fluoridetherapy.pdf