The use of respirators in the dental office requires OSHA compliance
Originally published May 28, 2020. Updated August 1, 2020.
As many dental practices across the United States are returning to providing care for patients, they are implementing the use of N95 masks or respirators for employee protection. While the use of N95s is recommended by the CDC and OSHA when treating a patient who is positive or suspected to be positive for COVID-19, practitioners are instituting the use of N95s for the entire workday due to the potential of exposure through aerosols in the dental office.
The use of N95s requires establishing an OSHA-complaint respiratory protection program. Until now, an N95 mask was mostly used in construction industries and manufacturing, so this is new territory for dental offices. Hopefully, this will help guide dental offices in compliance if you are instituting the use of N95 or higher masks in your office.
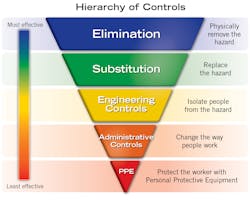
The Occupational Safety and Health Administration (OSHA) requires that employers protect their employees from workplace hazards that could cause injury or illness. Specifically, the General Duty Clause of the Occupational Safety and Health Act of 1970 states, “each employer shall furnish to each of his employees employment and a place of employment which are free from recognized hazards that are causing or are likely to cause death or serious physical harm to his employees.”1 In the hierarchy of controls (figure 1), the most effective is elimination and substitution of the hazard.2 This means that we remove or replace the hazard from the workplace. In dentistry, it is impossible for us to remove or replace the hazard when we are discussing exposure to pathogens in the form of viruses or bacteria, especially because patients may be asymptomatic. Therefore, we must utilize engineering controls, administrative controls, and personal protective equipment (PPE) to protect ourselves and employees.
PPE is worn by an employee to minimize the exposure to a variety of hazards. In dentistry, our PPE includes gloves, eye protection, and a mask, gown, and face shield. Until recently, dentists, hygienists, assistants, and lab technicians used an appropriate level procedure mask for the task being performed. As SARS-CoV-2, the virus that causes COVID-19, has become a threat to the health of medical and dental providers, recommendations for a higher level of respiratory protection have become necessary. This is due to the virulence of the pathogen and our proximity to patients while providing care. The new normal is for providers to wear an N95 mask while providing patient care likely to cause aerosols. The wearing of a respirator in a workplace in the United States requires specific procedures to ensure the equipment is effective. It is essential that an office design and implement a respiratory protection program before the first use and reevaluate the program annually.
An OSHA Respiratory Protection Program (29 CFR 1910.134)
OSHA’s respiratory protection standard requires employers to establish and maintain an effective program when employees must wear tight-fitting respirators to protect them from workplace hazards. This standard contains requirements for a written respiratory program that includes elements for program administration, work site-specific procedures, selection of appropriate respirator, employee training in the use of a respirator, medical evaluations, fit testing, instructions for use, cleaning, and storage. The program administrator must be qualified and trained to carry out all aspects of the program.
Employees must be aware of the risks of the job they are asked to perform. Simply wearing a respirator does not eliminate the hazard. If the respirator fails or does not fit properly, the employee may still be exposed to the hazard. To reduce the risk of an exposure, the program administrator will determine the best NIOSH-approved (National Institute of Occupational Safety and Health) respirator for the job as it relates to the risk.
In dentistry, it has been determined that a tight-fitting disposable N95 negative pressure respirator is applicable for protection against possible exposure to the SARS-CoV-2. A negative pressure respirator is one in which the air pressure inside the facepiece is negative during inhalation with respect to the ambient air pressure outside the respirator.3 In situations where an N95 or above are not available, some KN95s have been approved. Use these with caution, as they do not carry the NIOSH approval and many counterfeit ones have made it to the US market. Consult the FDA for a complete updated list of approved KN95s and N95s. Regardless of the respirator, a respiratory program is still required.
Once the administrator has decided on the specific respirator to be used, the employee who will be wearing the respirator must undergo a medical evaluation. The use of a respirator may place a physiological burden on the employee. A physician appointed by the employer should perform medical evaluations using a medical questionnaire and an initial medical exam. Some employees will not be able to wear a respirator. The medical exam is provided to the employee during work hours and at no cost to the employee. When an employee is given medical clearance, it is documented and maintained in the employee file. The employee can then be fit tested for the appropriate size respirator.
Fit testing for respirator use ensures that the mask fits properly on the face with an adequate seal. Facial hair, jewelry, or objects on the face, nose, and ears can interfere with the fit of the mask. Employees must be tested using the same type (make and model) respirator that will be used when performing a job. Fit tests may be qualitative or quantitative using OSHA-accepted protocols and procedures for testing. When an employee successfully passes a fit test using a specific model, that is the respirator model they will use. The fit of the mask should be evaluated with protective eyewear to ensure that the seal is not jeopardized.
After initial fit, additional tests may be needed if the employee has a change in facial structure through weight gain or loss, corrective surgeries, or dental procedures as this may change the fit. Otherwise, fit tests are required annually. (OSHA has currently waived all annual fit tests through September 30, but an initial fit test is still required prior to use.)
Training for use of a respirator should occur prior to placing an employee into a specific job where the respirator will be required. An employee must understand why wearing a respirator is necessary. This training should include use, maintenance, cleaning, repairing, and storage of the respirator. (Some of this may not be applicable to a disposable respirator.) Training should also include adverse effects of improper fit, neglect, and abuse of the respirator as this can compromise health and safety. Maintain safety training records for respirator use as with other OSHA programs.
Disadvantages to continual use of respirators
While respirators are recommended when workplaces contain airborne contaminants that cannot be controlled through engineering or administrative controls, they are not without dangers. While N95 masks and respirators filter out particles as small as a virus, they also reduce the oxygen intake of the wearer anywhere from 5% to 20%. Extended use of respirators can interfere with job performance as well as cause physiological and psychological stresses for the wearer. If not addressed and corrected, these stresses can become severe or cause life-threatening conditions. Respirators may interfere with respiration, thermal equilibrium, vision, communication, feelings of well-being, personal procedures such as eating or sneezing, and effectiveness of other protective equipment.4
The use of a respirator may increase the time it takes to complete a task when compared to completing the same task without a respirator. If time is critical for completion of a job it may become necessary to employ two people to perform the task. The decrease in work capacity is due to the demands of the physiological limitations on the respiratory system, cardiovascular system, and thermal equilibrium.4
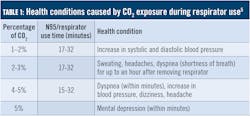
Headaches, shortness of breath, dizziness, and impaired decision have all been reported by employees wearing respirators for extended periods of time (table 1). Respirator use restricts the amount of oxygen exchanged when the wearer breathes. Recall basic anatomy and physiology: oxygen is delivered to the lungs when we breathe and is exchanged in the lungs where the oxygen is transported in the blood and is finally used in the muscles. We breathe in oxygen and exhale carbon dioxide in a respiratory exchange creating homeostasis. Respirators restrict a healthy oxygen exchange which causes our bodies to undergo physiological responses to compensate for the abnormal diffusion of carbon dioxide from the blood. This also causes an increase in the rate and depth of breathing thus cardiac output will increase to compensate for additional carbon dioxide exposure.5
The new normal in dentistry
As we seek a feeling of normalcy, some want to return to their offices, others want to wait because the zone of uncertainty is still too large, and yet others have vowed to never return to dentistry due to the risk. As health-care providers, we have a commitment to provide care to our patients. As an employee or employer, we are required to have a safe place in which to work. Finding a balance in a fluid environment such as the one we find ourselves in currently is difficult for all parties involved.
Talk with your employer or employees; everyone should have a voice in the safety programs you will utilize in your office. In dentistry, we have had years of training in infection control measures and the importance of implementing these measures to protect ourselves and our patients. The COVID-19 pandemic does not have to change the care we provide—it does change the way we provide that care! If an office does decide to implement respirator use as part of the PPE protocol as recommended by the CDC and OSHA, you are required to have a written respiratory program. Neglecting this requirement could cost the office huge fines and penalties from OSHA.
Editor’s note: An earlier version of this article was first published in the RDH eVillage newsletter. To sign up, visit rdhmag.com/subscribe.
References
- OSH Act of 1970. Occupational Safety and Health Administration. Accessed May 5, 2020. https://www.osha.gov/laws-regs/oshact/section5-duties
- Hierarchy of controls. The National Institutes for Occupational Safety and Health. Accessed May 5, 2020. https://www.cdc.gov/niosh/topics/hierarchy/default.html
- Standard Number 1910-134 – Respiratory Protection. Occupational Safety and Health Administration. Accessed May 5, 2020. https://www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.134
- Johnson AT. Respirator masks protect health but impact performance: a review. J Biol Eng. 2016;10:4. doi:10.1186/s13036-016-0025-4
- Sinkule EJ, Powell JB, Goss FL. Evaluation of N95 respirator use with a surgical mask cover: effects on breathing resistance and inhaled carbon dioxide. Ann Occup Hyg. 2013;57(3):384‐398. doi:10.1093/annhyg/mes068
Lori Gordon Hendrick, MS, RDH, CDA, CDT, is a licensed dental hygienist, certified dental lab technician, certified dental assistant, and dental office infection control consultant. She practices clinical dental hygiene and functions as office manager in a private practice in North Carolina. She also owns and operates Athena Dental Solutions LLC, a dental lab and consulting business. Hendrick recently completed her master’s in dental hygiene and global health. She is currently pursuing a doctoral degree in public aministration at Old Dominion University.
About the Author

Lori Gordon Hendrick, PhDc, MS, RDH, CDA, CDT
Lori Hendrick, PhDc, MS, RDH, CDA, CDT, is working toward a PhD in public administration and policy with a concentration in health policy at Old Dominion University. In addition to practicing dental hygiene, she owns Athena Dental Solutions and teaches clinical hygiene and professional development at Central Piedmont Community College. She’s a past president of the North Carolina Dental Hygiene Association, a consultant on the North Carolina Dental Society Work Force Task Force, and on the board of directors for North Carolina Caring Dental Professionals. Email Lori at [email protected].
Updated February 4, 2022