SARS-CoV-2, shoes, and spitting
Saliva has been at the forefront of our thinking for the past few months of the novel coronavirus pandemic, the largest concern being aerosols. Aerosols in dentistry have been noted through studies reporting contamination of saliva and dental aerosols since 1994.1,2 But not only could we be walking through viral particles suspended in the air from coughing, sneezing, dental procedures, or even simply breathing. The ground may also be contaminated as aerosols fall to the ground or if an infected individual spits virus-laden saliva.
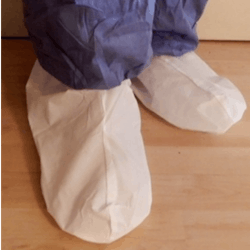
Exactly what are we taking inside buildings and homes on the soles of our shoes?
The COVID-19 pandemic has raised multiple issues regarding aerosol production from dental procedures, coughing, and sneezing, and the eventual flotation of the particles on to surfaces. A recent study reported that as medical staff walk around a ward, they can track the virus all over the floor. This was solidified in their study by the 100% rate of positivity from the floor in the pharmacy, where there were no patients.3 The virus had been tracked from one room where COVID-19 patients were treated into another room that should not have been contaminated. Samples from the soles of the intensive care unit medical staff’s shoes tested positive. The authors suggest that the soles of medical staff shoes might function as carriers of the virus leaving one room and entering another. This could have such far-reaching implications for hospitals, medical facilities, and dental facilities.
Many cultures leave shoes outside or in a room away from the rest of the home so that outside products do not contaminate other rooms of the main home. Many families have indoor shoes and outdoor shoes. This has become more common in the United States as well during the past few years. Certainly a consideration!
The role of spitting
By most cultural standards, spitting is known to spread disease and deemed socially unacceptable. In many countries, spitting has become so socially unacceptable that it is no longer considered a problem. In the United States, spit tobacco is the main reason people spit in public, and although the use of spit tobacco has declined through public education, the product is still an issue and a health consideration.
A recent editorial column by Dipankar Gupta, titled “Spitting in the coronavirus era: How Europe overcame the urge to spit, and why India might just succeed now” addressed some of the issues involved in spitting and the fact that many countries throughout history have ended this practice. The author suggests that this may be the opportunity to end this practice once and for all.
Gupta writes that when the practice of spitting stopped in Europe, it was not because of any “science” but rather the elite class found it repulsive.3 Because of the socially unacceptable connotation, just as smoking has dramatically decreased in own society, so did the practice of spitting on streets and sidewalks.
Even in early American settlements, it was not unusual to find “no spitting on the sidewalk” signs with a specified penalty. This was due to the fact that most people used the sidewalks or wooden paths since roads were often dirt filled. No one liked walking through spit puddles—especially women in long dresses. Gupta states that until the 18th century, the practice of spitting occurred because it was believed that swallowing one’s spit was physically unhealthy and immoral.3
Both Singapore and South Korea have laws prohibiting spitting in public places. Tuberculosis outbreaks contributed to some regulations regarding spit, and just as we are experiencing with the current COVID-19 pandemic, people became especially concerned with spit in general. Gupta suggests that the new regulations regarding wearing a mask may assist in limiting spitting by prohibiting a mask-wearing individual from spitting.
Conclusion
The COVID-19 pandemic has brought out the consideration of unseen pathogens and guidelines to remain healthy. I believe that the most beneficial academic course that dental professionals take is microbiology. Until this course is taken, I do not think that individuals understand the underworld of bacteria and viruses or those pathogens such as SARS-CoV-2.
As always, listen to your patients and continue to ask good questions!
This article first appeared in RDH eVillage, a weekly newsletter dedicated to dental hygienists. Join our mailing list here.
References- Bentley CD, Burkhart NW, Crawford JJ. Evaluating spatter and aerosol contamination during dental procedures. J Am Dent Assoc. 1994;125(5):579‐584. doi:10.14219/jada.archive.1994.0093
- Harrel SK, Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. J Am Dent Assoc. 2004;135(4):429‐437. doi:10.14219/jada.archive.2004.0207
- Guo ZD, Wang ZY, Zhang SF, et al. Aerosol and Surface Distribution of Severe Acute Respiratory Syndrome Coronavirus 2 in Hospital Wards, Wuhan, China, 2020 [published online ahead of print, 2020 Apr 10]. Emerg Infect Dis. 2020;26(7):10.3201/eid2607.200885. doi:10.3201/eid2607.200885
- Gupta D. Spitting in the coronavirus era: How Europe overcame the urge to spit, and why India might just succeed now. The Times of India. March 30, 2020. https://timesofindia.indiatimes.com/blogs/toi-edit-page/spitting-in-the-coronavirus-era-how-europe-overcame-the-urge-to-spit-and-why-india-might-just-succeed-now
NANCY W. BURKHART, EdD, MEd, BSDH, AAFAAOM, is an adjunct professor in the Department of Periodontics-Stomatology, College of Dentistry, Texas A&M University, Dallas, Texas. She is founder and cohost of the International Oral Lichen Planus Support Group (dentistry.tamhsc.edu/olp/) and coauthor of General and Oral Pathology for the Dental Hygienist, now in its third edition. Dr. Burkhart is an academic affiliate fellow with the American Academy of Oral Medicine, where she also serves as chair of the Affiliate Fellowship Program Committee. She was awarded the Dental Professional of the Year in 2017 through the International Pemphigus and Pemphigoid Foundation, and she is a 2017 Sunstar/RDH Award of Distinction recipient. Her professional interests are in the areas of oral medicine and the relationship between oral and whole-body health, with a focus on mucosal disease and early oral cancer detection. Contact her at [email protected].
About the Author
Nancy W. Burkhart, EdD, MEd, BSDH, AAFAAOM
NANCY W. BURKHART, EdD, MEd, BSDH, AAFAAOM, is an adjunct professor in the Department of Periodontics-Stomatology, College of Dentistry, Texas A&M University, Dallas, Texas. She is founder and cohost of the International Oral Lichen Planus Support Group (dentistry.tamhsc.edu/olp/) and coauthor of General and Oral Pathology for the Dental Hygienist, now in its third edition. Dr. Burkhart is an academic affiliate fellow with the American Academy of Oral Medicine, where she also serves as chair of the Affiliate Fellowship Program Committee. She was awarded the Dental Professional of the Year in 2017 through the International Pemphigus and Pemphigoid Foundation, and she is a 2017 Sunstar/RDH Award of Distinction recipient. Her professional interests are in the areas of oral medicine and the relationship between oral and whole-body health, with a focus on mucosal disease and early oral cancer detection. Contact her at [email protected].