Pain: Prevention, management, or therapy?
Editor’s note: This is part two of a two-part series. Read part one.
One of the primary functions of pain is to alert the body to potential danger. Pain is a warning mechanism that protects an organism by influencing it to withdraw from harmful stimuli; it is primarily associated with injury or the threat of injury.1 Logic might imply that the threat of injury should be enough to tell the body to automatically pull away from the harmful stimuli, right?
Unfortunately, chronic pain does not elicit that same kind of “hand on a hot stove” reaction. Chronic pain is more complex. It is more than a sensation or the physical awareness of pain; it also includes perception and the subjective interpretation of the discomfort.2
Pain reception versus pain tolerance
Perception and response to pain vary dramatically from person to person. The context of pain and the meaning it has for each sufferer determine how pain is perceived.1 A pain reception threshold is defined as the point at which a stimulus begins to become painful. A pain tolerance threshold is the point at which pain becomes unbearable.1
Pain from dental hygiene: A nuisance, distressing, or debilitating?
Your ergonomic journey: Protect your new hygiene career by prioritizing your health
Studies have determined that gender, ethnicity, childhood experiences, and cultural attitudes are factors that can contribute to the development of individual perceptions and tolerances of pain.1 A higher tolerance of pain may be perceived as stoic or brave for some individuals due to cultural attitudes, while others falsely tolerate higher pain levels due to fear of financial loss or the disruption of a balanced family dynamic.
Prevent, minimize, or treat
Call it disengaging, retreating, or even retiring, but the first step to successful pain relief begins with an honest determination of your expected outcome. Is the search for injury prevention, pain management, or therapeutic relief of existing pain? Is it to improve function and increase quality of life, or is it just to get through a few more years of employment at all costs? While a portion of the solution may be similar or overlapping, the actual pathway to achieve each of these outcomes is significantly different.
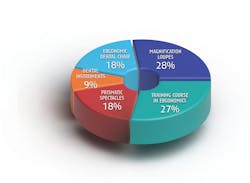
Injury prevention involves modifications to work practices, work space, and equipment, and adoption of daily strength training and muscle stretching. Products and systems are preventive, but they will not actually treat existing disorders or physical damage. In some circumstances, the use of various products may provide some pain relief, but pain is a sign that a disorder or damage is present. A medical diagnosis and intervention are still needed. A systematic literature review by Lietz, Ulusoy, and Nienhaus concluded that the most effective preventive ergonomic interventions are ergonomic stools, magnification loupes, prismatic spectacles, selection of dental instruments, and a training course in ergonomics (figure 1).3Additional preventive products or equipment to assist in the maintenance of neutral posture can include an intraoral camera, high-definition mirror, cordless handpiece, hands-free periodontal charting, ultrasonic scalers, accessories that are designed with a contra-angle, patient chairs with a narrow back and a double-articulating headrest, and a delivery system with straight, lightweight handpiece cords.
While pain management may include some the preventive products and systems, it is much more complex and involves medical intervention, preferably with the assistance of medical professionals at a pain management clinic. Alternative treatment includes acupressure, acupuncture, massage therapy, hydrotherapy, dry needling, chiropractic therapy, and/or relaxation techniques such as yoga, hypnosis, and meditation—along with a healthy diet and routine exercise.2 Additional interventional pain management options include trigger-point injections, root block injections, radiofrequency ablation, facet and sacroiliac joint injections, or platelet-rich plasma therapy.4 The stimulation of additional peripheral nerve endings by a transcutaneous electrical nerve stimulation (TENS) unit sometimes has an inhibitory effect on the nerve fibers generating the pain. It is thought that this is the same mechanism of action for acupuncture, compresses, and heat treatment.5
Treatments to reduce anxiety can result in a decreased need for a higher level of prescription pain medications.5 Persistent chronic pain management presents the greatest challenge in pain management. The source of such pain may not be obvious. Because chronic pain can cause psychological complications such as depression, sleep disturbance, loss of appetite, and feelings of hopelessness, its treatment is usually multidisciplinary.5
Surgical methods are usually only used if drug therapy and local anesthesia wane in effectiveness or prove to be completely unsuccessful. Surgical severing of the nerve can result in severe side effects such as numbness, motor loss, or relocalization of pain.2,5 One surgical alternative is to implant a pump beneath the skin to deliver pain medication directly to the spinal cord. An additional surgical alternative is to implant a spinal cord stimulation electrical device to disrupt the nerve, which inhibits the transmission of pain signals.2,5 Positive surgical outcomes have increased due to improved anesthetic techniques and minimally invasive surgical procedures utilizing the laparoscope.5
Pain due to work-related musculoskeletal disorders/injury is generally preventable, treatable, and successfully resolvable if the cause of the pain is accurately determined. Early medical intervention and clear communication for the expected outcome lead to the most successful resolution.
Editor's note: This article appeared in the July 2022 print edition of RDH magazine. Dental hygienists in North America are eligible for a complimentary print subscription. Sign up here.
References
- Meldrum ML. Pain. Physiology and psychology. Encyclopædia Britannica. February 1, 2021. Accessed April 14, 2022. https://www.britannica.com/science/pain
- Pain. The Free Dictionary. Accessed April 14, 2022. https://medical-dictionary.thefreedictionary.com/pain
- Lietz J, Ulusoy N, Nienhaus A. Prevention of musculoskeletal diseases and pain among dental professionals through ergonomic interventions: a systematic literature review. Int J Environ Res Public Health. 2020;17(10):3482. doi:10.3390/ijerph17103482
- Curie E. Interventional pain management. PowerPoint slides. Presented at: THRIVE–Ergonomic Summit; 2022; Colorado Springs, CO. Retrieved from presenter.
- Meldrum ML. Alleviation of pain. Encyclopædia Britannica. February 1, 2021. Accessed April 14, 2022. https://www.britannica.com/science/pain/Alleviation-of-pain
About the Author

Cindy M. Purdy, BSDH, RDH, CEAS
Cindy M. Purdy, BSDH, RDH, CEAS, has a passion for workplace wellness that has resulted in the creation of THRIVE, a dental-oriented wellness and therapeutic alternatives summit for dental professionals. THRIVE occurs three to four times annually at Glen Eyrie Castle in Colorado Springs, Colorado. Attendance information can be found at cindypurdy.com. In addition to multiple decades as a clinical dental hygienist, Cindy holds an ergonomic certification from Colorado State University, a certified ergonomic assessment specialist credential, and is certified in health-care ergonomics.