A path to fewer aerosols with ultrasonics
Clinicians must use their knowledge, skill, and judgment when considering instrument choices. This is especially true with ultrasonic instruments since they generate aerosols.
First things first: diagnosis
Having a diagnosis is essential. Instrument selection should be based on a diagnosis, not just the degree of deposits present. We are not treating the appointment book but rather a complex person. We must consider the patient’s clinical condition, the prognosis, and risk for disease. Are they healthy, actively infected, or in remission? Sounds medical, doesn’t it? Well, it is. We are health-care professionals.
The 2018 American Academy of Periodontology/European Federation of Peridontology (AAP/EFP) Classification System created a staging and grading framework for case definition.1 The severity of clinical attachment loss (CAL = recession, pocket depth, radiographic bone loss) will dictate the root surface anatomy that is available to instrument and the complexity.
The revised 2016 American Dental Hygienists’ Standards of Clinical Dental Hygiene Practice documents the process of care: assessment, diagnosis, planning, implementation, evaluation, documentation.2 Once a diagnosis and plan are made, the clinician can provide preventive services, such as cosmetic prophylaxis, as well as therapeutic services. In medicine, procedures are never delivered without a diagnosis. The diagnosis dictates your care plan and instrument selection.
Ultrasonic technologies
Ultrasonics has two components: frequency and amplitude. The frequency is the number of times the ultrasonic insert/tip (UIT) moves. Amplitude is the distance it moves. Magnetostrictive and piezoelectric are both ultrasonics. Most units operate between 25,000 and 42,000 cycles per second (25 K to 42 K). The higher the frequency, the smaller the active surface area of the UIT.
Magnetostrictive stacks drive the insert to produce elliptical motion. There is no figure-eight motion of magneto UITs in patient clinical procedures. The figure-eight motion was observed in an abnormal laboratory condition when no water was used for an extended period of time. A clinician would never use ultrasonics of any kind without water in a live clinical situation. Without water, the magneto handpiece would also become very hot.
Piezoelectric crystals in the handpiece produce linear motion. The lateral surfaces of the tip are used. In many ways, you already know how to use a piezo tip. Think of it as a powered universal curette, like a Columbia 13/14 or Barnhart 5/6, in which you use the lateral sides of the instrument. You lean the piezo tip at a 0-5° angle against the tooth surface, versus a 15° angle with magneto.
Aerosol generation
Both magneto and piezo technologies require water. While piezo requires less water to cool the crystals in the handpiece versus magneto stacks, water is still required to cool the tip-to-tooth interface. The water flow should be adjusted to a rapid drip with the point up to ensure water reaches the working end when used in the maxillary arch.
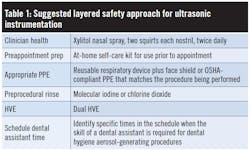
Use a layered approach4
If you choose to use ultrasonics, the aerosol containment strategy should be layered (table 1).
Start with your own health. Use xylitol nasal spray, such as Xlear, twice daily, two squirts per nostril.5
Pre-appointment prep sets the stage for increased emphasis on self-care. Recommend a pre-appointment prep regimen. You could make a customized kit or use new programs from manufacturers such as Colgate Professional Direct in which professionally recommended products are delivered to the patient’s door.6 Crest and Oral-B have six different bundled at-home product solutions.7
Preprocedural rinses can decrease microbial loads. Molecular iodine from ioTech International is a clear iodine product.9 Chlorine dioxide, such as CloSYS10 or OraCare,11 also has made claims on microbial reduction. A proposed CDT code for preprocedural rinses has been submitted to the Codes Maintenance Committee of the ADA by the DentalCodeology group and will be voted on in March 2021.
High volume evacuation (HVE) is necessary. A saliva ejector should be used only for pooled fluids. Veena et al. stated “it was not a very efficient tool in reducing the aerosol cloud.”12 HVE “will remove up to 100 cubic feet of air per minute. The small opening of a saliva ejector doesn’t remove a large enough volume of air to be classified as an HVE.”4 The James B. Edwards College of Dental Medicine at the Medical University of South Carolina conducted research showing dual HVE was the best at reducing aerosols.13 This initial research examined high-speed handpieces. On a practical note, install a T-junction in the HVE line for a dual HVE line. Devices such as the CordEze can reduce hand and wrist fatigue while holding the HVE.14 Alternatively, in the morning huddle, identify those specific times you anticipate the need for HVE and make sure to schedule a dental assistant. There has been an influx of external aerosol capture devices. Before purchasing, do thorough research. These external devices are not meant to replace intraoral HVE.
Imagine if there were no aerosols during procedures. Investigators from the University of Illinois at Chicago added an FDA-approved high molecular weight polymer, polyacrylic acid (PAA), in water to create viscoelastic forces that prevent droplet formation.15 Essentially, the PAA makes the water “stretchy” and doesn’t create aerosols. While this research looks promising and is part of a provisional patent, additional research is needed on how the PAA impacts the abilityPaschke’s “low and slow” technique
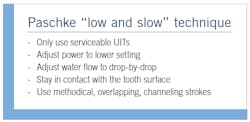
Serviceable UITs are required. Tips worn 2 mm or more are 50% less efficient, creating decreased amplitude.16 Worn UITs can burnish deposits. You wouldn’t consent to a medical provider performing a procedure with instruments that are worn and ineffective. As such, using worn UITs is akin to fraud. Inspect and measure your UITs monthly. Also, evaluate the stacks on magneto inserts. Bent stacks will not transmit energy to clean efficiently.
Use lower power and drip water flow (figures 2 and 3)
When a manufacturer states that a UIT can be used at high power, you can go to a lower power setting. With a lower power setting, you can decrease the volume of water to a drip versus spray. Water should reach the final 2 mm of the UIT when it is against the tooth surface. The combination of lower amplitude and decreased water will decrease but not eliminate aerosols. Therefore, a layered approach is still necessary.
Be methodical and precise
When using lower power, stay in contact with the surface to maintain a higher energy transfer. Use overlapping, channeling strokes as if coloring in the entire surface. This requires expertise in root anatomy and takes time. It should not be rushed.
Clinicians should follow state and federal guidance on aerosol-producing procedures. If you determine ultrasonics is the choice based on the patient’s diagnosis, employ a layered approach and Paschke’s “low and slow” technique for ultrasonic implementation.
Author’s note: Acknowledgment to Richard Paschke, Paschke Ultrasonix, for technical review.
References
- Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J Periodontol. 2018;89(Suppl 1):S159-172.
- Standards for Clinical Dental Hygiene Practice – Revised 2016. American Dental Hygienists’ Association. Accessed October 30, 2020. https://www.adha.org/resources-docs/2016-Revised-Standards-for-Clinical-Dental-Hygiene-Practice.pdf
- Harrel SK, Barnes JB, Rivera-Hidalgo F. Aerosol and splatter contamination from the operative site during ultrasonic scaling. J Am Dent Assoc. 1998;129(9):1241-1249.
- Harrel SK, Molinari J. Aerosols and splatter in dentistry: A brief review of the literature and infection control implications. J Am Dent Assoc. 2004;135(4):429-437.
- Nasal spray and sinus irrigation. Xlear Proactive Health. Accessed October 30, 2020. https://xlear.com
- Make your recommendations a reality. Colgate Professional Direct. Accessed October 30, 2020. https://www.pro.colgatedirect.com
- Crest + Oral-B 2020 Product Guide. Revised July 2020. p. 3-4.
- Breathe better with Clara. Clara. https://www.breatheclara.com
- Moskowitz H. University study: molecular iodine rinse completely effective in 30 sec against SARS CoV-2. ioTech International. October 28, 2020. Accessed October 30, 2020. https://www.iotechinternational.com/post/comparative-analysis-of-antiviral-efficacy-of-four-different-mouthwashes-against-sars-cov-2
- Antimicrobial formula doesn’t have to hurt to work. CloSYS. Accessed October 30, 2020. https://closys.com
- New study: OraCare Rinse found greater than 99.99% effective against human coronavirus with no toxic effects on tissue. OraCare. Accessed October 30, 2020. https://www.oracareproducts.com/coronavirus-info.html
- Veena HR, Mahantesha S, Joseph PA, Patil SR, Patil SH. Dissemination of aerosol and splatter during ultrasonic scaling: A pilot study. J Infect Public Health. 2015;8(3):260-5. doi: 10.1016/j.jiph.2014.11.004
- Ravenel TD, Kessler R, Comisi JC, et al. Evaluation of the spatter-reduction effectiveness and aerosol containment of eight dry-field isolation techniques. Quintessence Int. 2020;51(8):660-670.
- Simple ergonomic breakthrough. CordEze. Accessed October 30, 2020. https://cordeze.com
- Plog J, Wu J, Dias YJ, et al. Reopening dentistry after COVID-19: Complete suppression of aerosolization in dental procedures by viscoelastic Medusa Gorgo. Phys Fluids. 2020;32(8):10.1063/5.0021476. doi:10.1063/5.0021476
- Lea SC, Landini G, Walmsley AD. The effect of wear on ultrasonic scaler tip displacement amplitude. J Clin Periodontol. 2006;33(1):37-41.
- Chapple ILC, Walmsley AD, Saxby MS, Moscrop H. Effect of instrument power setting during ultrasonic scaling upon treatment outcome. J Periodontol. 1995;66(9):756-760.
Noel Paschke, MS, RDH, is a perpetual reinvention agent who has been a hospital RDH at Johns Hopkins, private practitioner, and dental hygiene faculty member at the University of Maryland. She has led three international dental companies’ North American dental education programs (Dentsply, Philips, Acteon) and was a consultant for a malpractice attorney. Currently, Noel owns Ultrasonics Plus, an education and training company that creates clarity and clinical excellence utilizing ultrasonic therapies.
About the Author

Noel Slotke Paschke, MS, BSDH, RDH
Noel is an award-winning former faculty at the University of Maryland Dental School and has led three international companies’ education departments, including Dentsply Cavitron, Philips Sonicare, and Acteon. She offers consulting and educational services through her company Ultrasonics Plus.