Originally published June 18, 2020. Updated August 1, 2020.
Dear Dianne,
Now that many offices are opening back up, I have so many unanswered questions that I don’t even know where to begin. I’ve always practiced impeccable infection control protocol, but now everything has changed.
In a Zoom meeting he conducted with his staff, my employer stated that the pandemic was no different than a bad outbreak of the flu. He stated that all of the hoopla we’ve been hearing on the news is a conspiracy, a way to control the people. However, he did state that he would provide face shields and disposable gowns.
I am terrified to return to work. I’m hoping you will have some words of comfort that will help ease my troubled mind. I love my patients and the work I do, but this is hard!
Troubled RDH
Dear Troubled,
According to the American Dental Hygienists’ Association, there are over 150,000 licensed dental hygienists in the United States. The COVID-19 pandemic has affected every person in every state, and I think it is safe to say that all 150,000 of your colleagues are having the same troubling thoughts that you are having.
I have to say that your employer’s attitude is upsetting, and I’m sure I would be concerned if I worked with a doctor who did not take this pandemic seriously. His words may just be a way to deflect or quell fears, or maybe he’s been spending too much time on social media. There are lots of conspiracy theories floating about, but the fact that to date, the United States has had 4,320,000 confirmed cases and 150,000 deaths is clearly indicative of more than a “bad outbreak of the flu.”
The current viral pandemic blindsided us in dentistry. While we’ve always been aware that the procedures we do create lots of aerosols, we’ve never been confronted by the specter of viral-laden aerosols that can linger in the air and possibly have the ability to make us very sick or even cause death. According to the New England Journal of Medicine, the virus is viable in suspended aerosols for up to three hours.1
A recent recorded webinar on the American Dental Association website, titled “The role of aerosol on the transmission of coronavirus and the impact in dentistry,” shared valuable science-based information on the aerosolization of viruses.2 One presenter is Dr. Donald Milton, who has more than 20 years of experience in environmental and occupational medicine with a research focus on disease aerobiology and exhaled breath. The other presenter is Dr. Purnima Kumar, who is a practicing periodontist with a PhD in molecular microbiology and is actively involved in research through the National Institutes of Health.
Dr. Milton discusses transmission, especially through asymptomatic people, stating that “up to 45%-50% of transmissions are from people who are not having symptoms but who may develop symptoms later. Some carriers never develop symptoms.” Dr. Milton shares that people create aerosols through breathing, talking, coughing, or sneezing. The distribution of aerosols depends on the airflow in the room. In hospital settings, they have found heavier viral deposition on the outer garments of people who worked in small, confined spaces rather than large spaces.
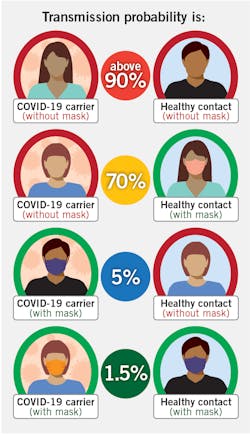
Shared during a recent ADA webinar, Figure 1 shows how two studies have suggested medical masks prevent the spread of the coronavirus.2–4 However, Dr. Kumar states, “Absence of evidence is not evidence of absence.” There are several studies now that show coronavirus in saliva, the upper respiratory tract, major and minor salivary glands, and possibly in the gingival crevicular fluid. So now, “we must practice to the highest levels of infection control, not because we have evidence of the virus in aerosols but because we don’t have evidence that it is not transmissible in the aerosols that come from the patient’s mouth.” Dr. Kumar also recommended that we insist our patients wear masks except for when their actual dental procedures are occurring.
The best way to reduce aerosols is through the use of high-volume evacuation (HVE). According to Harrel, intraoral HVE can reduce aerosols 90% to 98%.5 More recently, extraoral HVE has been introduced to the market. These units are typically positioned about 12 inches from the patient’s mouth. Some have HEPA filters or UV lights. Some models have the capacity to remove up to 300 liters per minute. The only problem is that we don’t have solid studies that prove the efficacy of external HVE units. The information is still evolving.
Preprocedural mouthwashes have been recommended in the past for reducing oral pathogens prior to dental procedures. Now, in the midst of COVID, preprocedural rinses are more important than ever. There are a number of options, but the recommendation is to use something that is known to inactivate viruses. In an article in the International Journal of Oral Science published in May 2020, they found that 1% hydrogen peroxide or 0.2% povidone iodine was more effective against viruses than other rinses.6 Although not tested against the COVID-19 virus, a molecular iodine product, IoRinse, has been found to be very effective in inactivating human coronavirus #229E and rhinovirus type 14 at 25 ppm.7 The ready-to-use rinse is 100 ppm. It is nonstaining and has a pleasant taste.
The biggest and most burdensome change for dentists and dental hygienists is the extra personal protective equipment (PPE) being recommended. The recommendations now are to avoid aerosol-producing procedures when possible, and wear a surgical mask, eye protection (goggles, protective eyewear with solid side shields, or a full-face shield), and a gown or protective clothing.8 More information on PPE can be found on the CDC’s website. Please keep in mind that this is a rapidly changing area that will likely see a number of new products on the market in the near future.
The fact is, nobody likes change. We settle into a routine with patient care, and we’d prefer to keep it that way. However, we cannot control circumstances that necessitate change, so we must change some of the ways in which we practice to ensure safety for ourselves and our patients. There was a similar situation in the mid-’80s when the AIDS virus was first identified. As a ’78 graduate, none of my training mandated gloves, a mask, or protective eyewear. I did not enjoy the new level of PPE back then, but everyone eventually adjusted to the new mandates.
Since information is constantly being updated, I know that what I write today may change shortly. So, I want to point you to the best information that is available. Please stay updated as things progress. The best information can be found by visiting the websites in the Resources section below.
Finally, I want to give you some hope. We in dentistry are resilient, smart, and strong. We will rise to this challenge. We cannot allow fear to chain us. We’ve been knocked down, but we are not defeated. Our patients need us, and the care we provide helps them live healthier lives. It is a noble calling.
All the best,
Resources
- ADHA releases interim guidance on returning to work. ADHA. Updated June 18, 2020. https://www.adha.org/adha-interim-guidance-on-returning-to-work
- https://www.coronavirus.gov/
- Cases in the U.S. Centers for Disease Control and Prevention. Updated June 30, 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html
- Interim infection prevention and control recommendations for healthcare personnel during the coronavirus disease 2019 (COVID-19) pandemic. Centers for Disease Control and Prevention. Updated May 22, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html
Editor’s note: An earlier version of this article was first published in the RDH eVillage newsletter. To sign up, visit rdhmag.com/subscribe.
References
- van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564-1567. doi:10.1056/NEJMc2004973
- The role of aerosol on the transmission of coronavirus and the impact in dentistry (recorded webinar). American Dental Association. May 14, 2020. https://ebusiness.ada.org/Education/viewcourse.aspx?id=428.
- Eikenberry SE, Mancuso M, Iboi E, et al. To mask or not to mask: Modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect Dis Model. 2020;5:293-308. doi:10.1016/j.idm.2020.04.001
- Howard J, Huang A, Li Z, et al. Face masks against COVID-19: an evidence review. Preprints. doi:10.20944/preprints202004.0203.v1
- Harrel SK, Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. J Am Dent Assoc. 2004;135(4):429-437. doi:10.14219/jada.archive.2004.0207
- Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12(1):9. doi:10.1038/s41368-020-0075-9
- ioTech International. https://www.iotechinternational.com/
- Interim infection prevention and control recommendations for patients with suspected or confirmed coronavirus disease 2019 (COVID-19) in healthcare settings. Centers for Disease Control and Prevention. Updated May 18, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html
DIANNE GLASSCOE WATTERSON, MBA, RDH, is a consultant, speaker, and author. She helps good practices become better through practical analysis and teleconsulting. Visit her website at wattersonspeaks.com. For consulting or speaking inquiries, contact Watterson at [email protected] or call (336) 472-3515.
About the Author
Dianne Glasscoe Watterson, MBA, RDH
DIANNE GLASSCOE WATTERSON, MBA, RDH, is a consultant, speaker, and author. She helps good practices become better through practical analysis and teleconsulting. Visit her website at wattersonspeaks.com. For consulting or speaking inquiries, contact Watterson at [email protected] or call (336) 472-3515.
Updated June 30, 2020