A practical guide for testing dental unit waterlines: Part 3
In the February issue of RDH, part one of this series discussed the science of dental unit waterline systems (DUWS), agencies thatoversee DUWS, and resources to help with compliance. Part two in the March issue discussed a case study and keys to maintenance. In part three, I provide solutions if a testing failure occurs.
What if I fail?
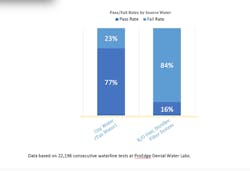
Learning the needs of your DUWS is part of the process. Many offices fail on the first test and are able to resolve issues that could impact the bacterial counts (CFU/mL). Thirty-one percent of treated waterlines fail.1 As offices train their staff, investigate and understand their systems, and get expert consultation, pass rates go up significantly. The top six reasons why offices fail waterline tests include:
1. Not shocking ever or enough; using the wrong product for shocking and daily care
2. Not following product instructions for use (IFU)
3. Poor source water (figure 1)
4. Relying on central systems, in-office distillers, or distilled water
5. No water reservoir on dental unit for shocking
6. Not following waterline testing shipping instructions; cross-contamination of sample vials
As in other areas of infection control, such as sterilization, most of the failures can be attributed to operator error.2 The following can help you achieve compliance.
Change the water bottle properly
It is important to be careful when changing the bottle on the dental unit. We observed dental offices removing bottles barehanded and allowing the plastic tubing to hang in the atmosphere, creating a potential source of contamination (figure 3). Have spare bottles available so you can replace the empty bottle with a full bottle immediately after removal. This saves both time and decreases possibility of contamination.
Related reading
Follow the IFU for antimicrobials
Second only to regular shocking, this is one of the largest determining factors in testing success.Shock and daily treatment IFUs should be followed at all times. Do not dilute or deviate from the requirements. Know what is required of the product you choose to use. For example, if you are going to use a bound iodine product, make sure your chlorine level is correct if you are using city water. The product you use should tell you that level, which is generally 1.0 ppm. Know how to test the iodine level. Know if the product has EPA approval as a disinfectant. Read and follow the instructions for use closely.
Test your product
Some of the products require periodic testing of the disinfectant level. This is due to outside factors, such as needing to know the level of chlorine in water that is treated with an iodine-based product. Using a very simple, inexpensive test strip, you can be assured the iodine-based product is working effectively between waterline testing.
Flush and purge the lines
Flush your lines at the start of the day for two minutes and for 20 to 30 seconds between patients. Purge or remove water out of all lines at the end of the day. For more, see “Water safety: Protocol for flushing waterlines” in the April 2018 issue of RDH magazine or at bit.ly/wl-protocol.
Allowing the lines to be free of water at the end of the day will reduce biofilm formation. This is especially important for the waterlines of ultrasonic units. Allowing the device to sit for days with water present creates a perfect environment for biofilm formation and bacteria proliferation.
As dental health-care professionals (DHCP), we face many challenges in adhering to the standard of care. Our goal of staying up-to-date can protect both the patient and DHCP from disease. Bringing new research and regulations forward can limit the risks involved in DUWS. Understanding the practical steps to take to maintain water quality keeps your patients, you and your team, and the practice safe.
References
1. Dewhurst N, Molinari JA. Treating and Monitoring Water. CDEWorld website. https://cdeworld.com/courses/21039-Treating_and_Monitoring_Dental_Water. Published May 2018.
2. Centers for Disease Control and Prevention. Guideline for Disinfection and Sterilization in Healthcare Facilities (2008). Centers for Disease Control and Prevention website. https://www.cdc.gov/infectioncontrol/guidelines/disinfection/sterilization/steam.html. Updated February 27, 2018.
Author's note: A special thanks to the class of 2018 and Cabrillo College for their dedication to this research project: Amanda Anfield, Stephanie Archibald, Sarah Augenstein, Maria Becerra, Jessica Carrera, Kristan Castro, Daniel Donoghue, Jordan Durrer, Adriana Garza, Esther Gonzales, Amanda Mason, Sara Nelson, Thomas Nop, Annalisa Ortiz, Sierra Partridge, Michelle Peterson, Thi Phan, Kathlyn Romero, Halley Santaella, Katia Serrano, Lorena Thomas, and Michelle Van Schoick.
Questions to ask if you continue to fail
Looking at all aspects of waterline contamination is a must.Investigate the following if your tests are failing.
• If you are using city water, what is the count before it enters the building? Is there a filter on the building? Has it been maintained?
• Is the filter or filters changed properly and in a timely manner? Our discovery of an additional filter on the unit revealed where the bacteria was being harbored. As soon as we replaced the filter and shocked the lines, all units were below the required CFU/mL and have remained so with further testing.
• What is the mineral content of the water? Is the content of the water interfering with the action of the disinfection product?
• If you use deionized (chlorine-free) water, have you addressed the need for an additional antimicrobial?
• Are the bottles that are being used to store water cleaned, disinfected regularly, and aired out at the end of the day? One of the DHCP we consulted with found this was the area where contamination was reoccurring. This person had not been cleaning or disinfecting the bottle.
• Is the microtubing kinked or bent? Our units with the highest counts included lines that had issues with kinking.
Updated November 29, 2022
About the Author
Noel Kelsch, MS, RDHAP
Noel Kelsch, MS, RDHAP, is a syndicated columnist, researcher, writer, speaker, and cartoonist. She is the director of Cabrillo College dental hygiene program, past president of the California Dental Hygienists ‘Association, and immediate past president of the Dental Hygiene Board of California. She owns her own dental hygiene practice that facilitates care for those dealing with homelessness and hospice care. She has received many national awards and may be reached at [email protected].