the BIOFILM between
Getting your patients excited about interproximal care
Biofilm- the culprit in the majority of our dental pathology issues.
Interproximal biofilm- the true antagonist in the film titled “Oral Care, Maintaining Your Teeth for a Lifetime.”
We can talk until we are blue in the face (no pun intended, which you will realize after you finish reading this article), but trying to explain to our patients about plaque can be highly frustrating. Unless the teeth are so heavily coated as to appear dull due to the thickness of the film, the patients just don’t get it. We have all scraped off a thick smear of plaque, not unlike taking excess butter off the side of a piece of bread, and used that visualization. But what can we do to show our patients more?
We know the plaque biofilm begins innocuously as nonpathogenic, normal, intraoral bacteria, which forms almost immediately after brushing, flossing, and dental prophylaxis. The later entrants in this biofilm collection are the anaerobic players that cause the destruction and inflammation. These anaerobes are the nasty pathogens that cause the most damage inside the sulcus. Remember, they can’t go out to eat, so they survive in their own little world - the protected sulcus. Depending on the depth of the sulcus, they have unlimited party space and limitless ability to do damage to the bone and supporting structures. This is not a commercial for “Well, if it forms immediately, then aren’t we in a losing battle, so why bother?” Absolutely not. The matrix can be disrupted by home and professional care, so that is why we need to bother. We need to reinforce our patients’ need to perform daily home care. We talk brush and floss, but we need to show and tell with some memorable information.
Our patients are relatively savvy about knowing their periodontal numbers. We probe and probe at each appointment, usually reciting the threes, fours, fives, and sixes to them so they are aware of their health or disease status. Then, we proceed with our oral-health instruction and dental prophylaxis. But in addition to pocket depth, we also see the effects of plaque and biofilm accumulation on our patients’ teeth. What we need to do is find more meaningful methods to inspire our patients to improve their own oral conditions by removing this invisible culprit.
Back in school, we were apprised of several plaque scores and indices. The Plaque Index by Silness and L?e focused on the thickness of the biofilm at the gingival area in addition to periodontal assessments of gingival color, consistency, and bleeding on probing. The Plaque Control Record by O’Leary, Drake, and Naylor evaluates plaque presence on all teeth surfaces, allowing patients to monitor their levels over time. Other indices do exist (Navy Plaque Index, Turesky Index, Patient Hygiene Performance, Simplified Oral Hygiene Index, and Quigley and Hein Index), if the clinician is more comfortable with those methods. The Plaque Free Score (PFS), which was developed by Grant, Stern, and Everett, measures location, number, and percentage of biofilm-free surfaces in the patient’s mouth. It will also assess papillary bleeding upon probing. The PFS is a more positive motivator for the patient.
Everyone has a different learning style. Some learn by seeing, some by doing, some by hearing. Our patients respond to a variety of stimuli during the dental visit. Depending on the value the information has on their immediate life, patients may or may not respond to our education. By using different formats to disseminate our oral self-care information, the higher the probability our patients will retain and act on our suggestions. Additionally, by using positive reinforcement, patients will be more receptive to our instruction.
The PFS records the biofilm on four surfaces of each tooth. To calculate this score, multiply the number of teeth by four to determine the number of available surfaces, and then subtract the number of surfaces with biofilm from the total available surfaces to determine the number of biofilm-free surfaces. The score is derived by multiplying the number of biofilm-free surfaces times 100, then dividing by the number of total available surfaces (Table 1). The evaluation of this system is relatively patient friendly. A score of 100 percent is ideal. This method is easily given to the patient for follow-up at home.
Now that we recall these methods to assess the patient’s biofilm numbers, how do we accomplish this important component of the educational process during our preventative maintenance time frame? The simplest method of assessment is to disclose the patient to enhance our oral hygiene instruction. I can see you cringing with school memories of the disclosant flying all over the place, coating all surfaces, biological or not, with red dye that was not easy to remove from extraoral surfaces. Yes, the red disclosing solution was an effective tool in determining our level of plaque removal expertise during our educational experience. It is also a great tool for patients to see where they are missing brushing and flossing, because what they can’t see, they don’t think is there. This system is portable and inexpensive. In addition to utilizing the disclosing solution chairside, we are able to distribute it to our patients to follow up at home. There are also solutions and tablets that demonstrate both new plaque and old plaque with staining variations (Table 2). Alas, there are some patient (and operator) compliance issues with this form of demonstrating the existence of biofilm.
When I first began my dental hygiene career, I worked in a periodontist’s office. We gave detailed instructions to patients regarding brushing, flossing, and interdental care. One of the devices we gave our patients was a unique disclosing solution that was used with a hand-held light source, called a “Plak Lite.” Utilizing a fluorescent dye, the biofilm was exposed to a light and glowed yellow. This product is now being reintroduced by Sunstar Butler as the GUM® Plak-Check®. By using the yellow sodium fluorescein liquid dye that becomes visible only with the provided blue light to disclose plaque, Plak-Check eliminates the residual stains common to tablet and other liquid disclosants. It is simple to use chairside and has a glowing (pardon the pun) revelation of biofilm presence.
The solution is supplied in individual cellophane-wrapped applicators that are infection-control- and operator-cleanliness-friendly. After activating by simply breaking the stick inside the wrap, the swab is placed below the tongue for a few seconds. Patients swish the liquid around in the mouth and rinse with a small amount of water. The detecting unit is comprised of a light-emitting source and a mirror to visualize the biofilm remaining on the teeth, which will glow yellow. To visualize the plaque, patients hold the light/mirror unit in front of their teeth. A hand-held dental mirror is provided to allow patients to visualize the linguals of their teeth.
Not only is this product now available again to the profession, but Sunstar will also be selling a consumer “model” that can be purchased wherever toothbrushes are sold. The home Plak-Check unit includes a bottle of solution for 50 applications along with a hand-held mirror that contains the light source. This is a great idea for kids. Adults will also be more willing to use a disclosant since Plak-Check solution is nearly invisible without the blue light. They can go about their business without the residual temporary staining of traditional disclosants.
Most importantly, when our patients are able to visualize their plaque levels, they tend to be more proactive in the removal of this biofilm. One bonus to all of this visualization: the patient is highly aware of all the bacteria living on the tongue. Instruction in tongue cleaning will be readily acceptable at this point of demonstration.
With all of this illumination, what do we do about the findings? By showing the patient where the biofilm is located and knowing the plaque numbers, we are better able to increase the patient’s knowledge about the importance of interproximal oral care. We know that only 13 percent of our patients floss on a regular basis. We also know that only 50 percent of the biofilm is removed from tooth surfaces with brushing alone. So, how do patients remove all of this interproximal plaque?
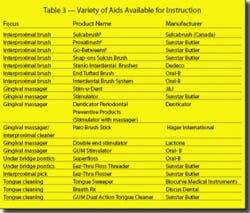
Various methods of interproximal cleaning are available. Let’s be honest: flossing is the most effective and least actively preferred by the majority of our patients. They will come up with many creative reasons why they don’t floss. Therefore, we need to come up with some creative solutions to entice our patients to begin new, healthier interdental habits. Armed with the knowledge of their biofilm numbers, and now able to visualize the actual biofilm enemy on their teeth, patients should be more willing to try other devices to remove the debris growing between their teeth. If they are reticent or unwilling to use dental floss, we need to be “at the ready” with other options (Table 3).
One of the first objectives in getting patients to discover interdental care is simplicity. We need to show them that if they don’t floss, they need to put something between their teeth to disturb, and hopefully remove, the biofilm matrix. Patients want to use something that is readily available (both from our distribution point of view and the market where they shop). Our patients look forward to their “goodie bags” to see what little trinkets we have bestowed upon them at their current preventive visit.
Interproximal cleaners run the gamut of wooden sticks, flattened on one side to both clean and stimulate, to small brushes that vary in size to fit almost every embrasure or under every pontic. Handles are made of either plastic or metal, with removable bristles. Sunstar Butler offers compact sizes that are perfect for taking to the office or travel. All Sunstar Butler brushes are antibacterial due to their coating with chlorhexidine. Two interproximal products have removable brushes angled off of plastic handles for use on facial/buccal or lingual/palatal surfaces. Sulcabrush is a Canadian product that has been available in the United States for many years. The conical brush is replaceable. They also make a smaller, travel version, the Pocket Sulcabrush. Both are excellent for getting under orthodontic appliances. Sunstar Butler has just introduced a similar product, GUM Snap-On Sulcus Brush, as an augmentation to its ergonomic Proxabrush handle. The antimicrobial brush has a 6 mm diameter, which makes it soft and flexible. In addition, the packaging comes with two extra refills for the handle. Oral-B offers a variety of interproximal brushes that “lock” into their handles. Multiple bristles are available, including soft foam for postsurgical care. A travel version is also available.
Interproximal massagers are another form of interdental care. Metal and plastic handles hold rubber tips that fit into the interproximal spaces and stimulate the tissue. These aids may remove some debris but do little effective mechanical plaque removal. Their main purpose is to flatten and massage the tissue.
Bridges and pontics may be cleansed by the interproximal bristles as mentioned above. Two alternatives for under-bridge care are offered by Oral-B and Sunstar Butler. Superfloss is a piece of floss that has a stiff end used to slide under the pontic. An area of fuzzy floss is used to clean under the prosthesis. Multiple strands are packaged together. Sunstar Butler Eez-Thru Floss Threader is a large loop of very thin nylon through which floss is threaded. The plastic piece is able to be cleaned and is reusable. Both are excellent to use with orthodontic appliances.
Encourage flossing, and also have some alternative interproximal tools to add to your vast array of choices.
References
• Wilkens E. Clinical practice of the dental hygienist. Lippencott, Williams & Wilkins, 9th Ed, 2004, 328-334.
• Navy Plaque Index. The Medical Algorithms Project: “ndices for evaluating dental health status. Chapter 9. http://www.medal.org/visitor/www/Active/ch9/ch9.01/ch9.01.06.aspx. Accessed Dec. 4, 2005.
• Sunstar Butler Product Information Data: GUM® Plak-Check®.
• Tongue Sweeper. http://www.tonguesweeper.com/properties.html. Accessed Dec. 4, 2005.
• Christou V, Timmerman M, Van der Velden U, Van der Weijden F. Comparison of different approaches of interdental oral hygiene: interdental brushes vs. dental floss. J Periodontology July 1998; 69:7:759-764.
• Waerhaug J. The interdental brush and its place in operative and crown and bridge dentistry. J Oral Rehabilitation 1976; 3:107-113.
• Kiger RD, Nyland K, Fellerk RP. A comparison of proximal plaque removal using floss and interdental brushes. J Clin Periodontology 1991; 18:681-684.
• Bergenholtz A, Olsson A. Efficacy of plaque-removal using interdental brushes and waxed dental floss. Scandinavian J Dental Research 1984; 92:198-203.
• Nayak R, Wade AB. The relative effectiveness of plaque removal by the Proxabrush® and rubber cone stimulator. J Clinical Periodontology 1977; 4:128-133.