Update on local delivery systems
Trisha E. O`Hehir, RDH, BS
We now have three products (five worldwide) for the delivery of subgingival antimicrobials. At first glance, this simply looks like a choice of adjuncts to supplement our current instrumentation approach. If we look closer, however, it could be an opportunity to completely change dental hygiene, resulting in far more effective therapy and much better use of our time! It`s up to us.
In the past, local drug delivery always has been viewed as an adjunct to traditional instrumentation. Efforts have been made to find the most effective antibiotic or antimicrobial and the best way to achieve prolonged release of these drugs within the pocket. It has been assumed that our primary focus should be subgingival instrumentation and that putting drugs into the pockets simply would enhance our instrumentation results. Maybe it`s time to look at these new products without our old "assumptions."
Dental hygienists strive to effectively remove as much subgingival calculus as possible. Our whole dental-hygiene world seems to revolve around calculus removal. Grades in school depend on calculus removal; state board exams count pieces of calculus; and the more calculus we remove from a mouth, the better we feel! Our professional existence depends on calculus; but, for most hygienists, our preference would be to effectively treat a patient. We would like to keep him or her calculus-free, never having to repeat the procedure, and thus freeing up more time to treat other patients. We all love the challenge of a calculus-laden new patient, but retreating that same patient recall after recall loses its fascination. Instead, let`s see if it is possible to get people healthy and keep them healthy.
We know periodontal disease is a bacterial infection and not caused by calculus. Subgingival calculus actually is a symptom of the disease and is produced by the infection itself. Our focus should be on the bacteria, not on the calculus. Focusing primarily on calculus will keep us tied to our power-scalers for life, with no end in sight to back pain and carpal-tunnel problems. We are dealing with a bacterial infection and these new drug-delivery systems should help us redirect our focus from calculus to bacteria.
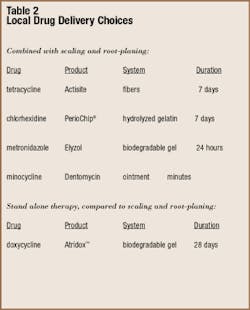
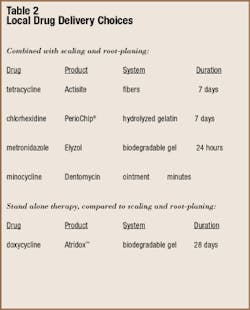
Let`s take a quick look at these products and then see how they can change the practice of dental hygiene. I have included a table summarizing information about the various products. We have one fiber, one chip, and three gels or ointments. The fiber-delivery system of Actisite was developed by Dr. Max Goodson and created the foundation upon which the new delivery systems are based. The chip incorporates chlorhexidine, and the others use antibiotics. All the gels and ointments are delivered to the subgingival area using syringes. The chips and fibers are placed individually using cotton pliers or other instruments. The fibers are the most difficult and time-consuming to place; the gels and ointments are the easiest. The chips definitely are easier to place than the fibers, taking less than a minute for each site.
Dentomycin and Elyzol, not yet available in the United States, come premixed in carpules ready to deliver. Atridox requires one-minute of mixing back and forth between two small syringes, one of which is then used to place the gel. The PerioChips are easier to place if kept refrigerated until just before placement. Actisite fibers must be cut to fit the pocket being treated.
No study has compared the five products directly, so you have to evaluate all the products individually and compare what you can. Actisite, PerioChip®, Dentomycin, and Elyzol have been tested in combination with scaling and root-planing. Used after instrumentation, the results are as good as or slightly better than scaling and root-planing alone. This difference is generally a millimeter or less. Atridox is the only product that has been evaluated in place of scaling and root-planing and found to be equivalent.
Before these products can be marketed in the United States, they must undergo rigorous and expensive testing for FDA approval. It is customary for the FDA to limit what a company can say about use of its product, based on how the research was done. Therefore, product instructions are very strict, not because that is the best and only way to use a product, but because that was how it was used in the studies for FDA approval. As knowledgeable clinicians, it is up to us to interpret those instructions and make adjustments based on our experience and the individual patient being treated.
For example, the PerioChip® instructions say patients should avoid using dental floss for 10 days at the site of chip placement, because that was how the study was structured. The apparent reason is to avoid removing the chip. However, dislodging the chip actually is quite uncommon, since it becomes a gel when in contact with fluid. It seems to me that daily, interproximal plaque removal is important and should be stressed, especially for patients with periodontal disease. Give them a 10-day vacation from interproximal plaque control and they will lose whatever habit you had worked so hard to establish! My approach would be to go ahead and risk removing a chip that has melted and have them continue cleaning interproximally.
Another example is the recommended use of a periodontal pack after Atridox™ placement. Instructions also say to avoid brushing and flossing the treated area for seven days. These instructions are required by the company, due to the fact packs were used in the FDA trials. The Atridox gel becomes waxy when it contacts fluid, so it should remain in the pocket just fine without placing a periodontal pack. In fact, patients in the studies who lost their packs after a few days had the same subgingival antibiotic level as those with packs in place the entire time. My feeling is that a periodontal pack will only enhance bacterial plaque accumulation in the area. Oral hygiene should be stressed. In other words, read the instructions and then use your own judgment and experience to get the best results with these products. Remember that the product instructions are based on the protocols followed in the research studies.
Atridox™ is considered a "stand-alone" product, since it was tested by itself and compared to scaling and root-planing. All the other products were tested in combination with scaling and root-planing. Since subgingival instrumentation is such a strong tradition in our profession, the companies selling these products recommend using the local drug-delivery systems after instrumentation. That`s true even with Block Drug, distributors of Atridox. Atridox has been shown to be as effective as instrumentation.
It reminds me of the early Cavitron® research of the 1950s that found the Cavitron and curettes equally effective in removing calculus. Did you realize we knew that in the 1950s? Despite these findings, the researchers concluded that ultrasonic scaling should not replace the traditional use of curettes. It has taken us 40 years to overcome those "assumptions" and look at the research findings objectively. I hope we don`t let our assumptions and traditions cloud our view of the research findings concerning these new, local drug-delivery systems.
If we look at the potential for controlling a bacterial infection with these new products, we can revolutionize dental hygiene therapy. We need to look at the research findings and set aside therapies based only on tradition. The six-month recall should be the first to go! Subgingival instrumentation removes hard and soft deposits, but how many bacteria pass through the pocket wall and enter the blood stream as a result? How many are forced into dentinal tubules? Perhaps we should be using these local drug-delivery systems before instrumentation, rather than after. Later, after removing the calculus, we might substitute maintenance instrumentation with local drug-delivery to avoid further calculus accumulation.
Imagine this scenario. You`ve completed the periodontal charting on a patient with early to moderate disease. You`ve explained the disease process and, together with the patient, determined the ideal, daily plaque-control routine. Instead of picking up your power-scaler, you reach for a local drug-delivery system to eradicate the bacterial infection. One week later, you will see the patient for debridement therapy. The bacterial level will be the lowest possible and the tissue will be distended slightly from the gel or chips you placed. Instrumentation should be much easier, with little or no bleeding, and considerably less pain. Instrumentation also should take less time without the usual bleeding and discomfort. The time scheduled in the past for quadrant-scaling and root-planing now will be devoted to finding the most effective means for this patient to control bacteria on a daily basis.
Prevention in the past was squeezed into an already busy schedule. Now, it will become the primary focus of our therapy. Over the next few weeks and months, you and the patient will achieve periodontal health using the therapies available. Instead of putting this patient on "recall," you will schedule short, monthly visits to monitor the bacterial levels and retreat with local delivery as needed. Short, comfortable appointments will please both you and your patient.
Reinfection no longer will occur from bacteria left in the pocket. Local drug delivery will effectively sterilize the area. Reinfection can come only from supragingival bacteria moving subgingivally. Finding effective, acceptable daily plaque-control measures will become essential. Hygienists will have the time to test and compare the effectiveness of various, new interproximal-cleaning devices. Just imagine ... a practice filled with periodontally healthy people!
If we take advantage of this new technology, we will be able to refocus our efforts. Right now, clinical dental hygienists devote most of their time to treating periodontal disease. We really are periodontal therapists. This new approach to therapy has the potential to change our focus from repeated calculus-removal appointments to treating bacterial infections.
Once treated, we will have the time to prevent recurrence for those patients and, more importantly, use our expertise to prevent bacterial infections in others. Our many years of dealing with periodontal disease provide us with unique knowledge and experience to control and prevent it. We will create a balance between our roles as a periodontal therapist and as a primary preventive specialist.
If giving up the current approach to treatment is not for you, you at least have some new options. Local drug-delivery systems can enhance the benefits of traditional instrumentation. For those areas that just don`t respond to mechanical treatment alone, these systems offer a method for delivering an antimicrobial to a specific, nonresponding area. All I ask is that you think about what these findings could mean to the future of dental hygiene practice. I think you will find it to be very exciting!
Trisha E. O`Hehir, RDH, BS, is a senior consulting editor of RDH. She also is editor of Perio Reports, a newsletter for dental professionals that addresses periodontics. The Web site for Perio Reports is www.perioreports.com. Her e-mail address is trisha@perioreports. com.