Just clean teeth
by Lynne H. Slim, RDH, BSDH, MSDH
[email protected]
Suzanne Newkirk, RDH, and I recently flew together from her Seattle home to southeastern Washington, where she works part-time for Bob Gottlieb, DDS, a periodontist. I remember Suzanne saying that working with Bob is like being Cinderella at a ball. Everything she could possibly desire in an office is there for her — the best co-workers, equipment, and employer. What a wonderful compliment to Dr. Bob, who is known to send text messages to his staff at the end of every workweek to thank them for their dedication and hard work.
I was fortunate to be able to observe Suzanne and Dr. Bob for an entire day, and I was tickled pink with Dr. Bob’s approach to a new patient exam. He draws pictures on his glove with a Sharpie pen to illustrate the bone, tooth, and gingival anatomy and explain the etiology of periodontal disease. I almost fell off my chair laughing when he explained bone loss in between roots because he used the analogy of exposing one’s crotch!
Suzanne is a perioscopy trainer and practitioner, and she finds it very exciting to have the opportunity to apply the technology in Dr. Bob’s periodontal practice. I was there when she met the following new patient, and I’m going to let Suzanne describe her findings in her own words. Following her description of the patient and initial therapy that follows, including her results, we’ll critique her protocol from an evidence-based perspective.
Background
Female, age 39. No health issues, no meds, no social habits. Patient is from Sri Lanka originally and has very advanced perio disease.
Diagnosis
Generalized chronic periodontitis, advanced in extent with associated occlusal traumatism; pocket depths 3-11 mm; recession: Nos. 20, 29; mobility: generalized Class l (No. 24 presents Class III); missing: Nos. 1,7,10,19,30.
Etiology
- History: pattern of dental care, only for dental emergencies; last hygiene care, never
- Local factors: supragingival and subgingival calculus, heavy deposits; plaque, heavy deposits; caries near gingival margin on Nos. 14; No. 16, 17 completely bombed out
- Signs of inflammation: sulcular bleeding, generalized; suppuration (sulcular) scattered throughout, especially lower anterior
- Initial treatment plan: Antibiotics to control the systemic infection; penicillin VK 500mg one week prior to therapy; improved personal oral hygiene; FM perioscopy with extraction of hopeless teeth Nos. 16, 1, 7, 24; impressions for a flipper to replace missing tooth No. 24; caries control restorations beginning with tooth No. 14; three-month periodontal maintenance
After initial disease control therapy, treatments could include:
- Laser surgery
- Orthodontics to position teeth in the proper place
- Tooth replacement therapy to replace missing teeth and teeth that might be lost in therapy
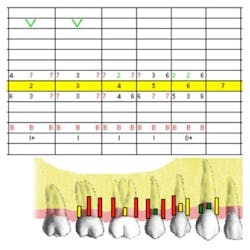
Pretreatment periodontal charting
UR Nos. 2-6
Pocket depths 3 to 7mm
Furcations: Class l buccal both molars
Generalized mobility: Class l
Generalized bleeding on probing (BOP)
Click here to view more charts
Treatment
- FM perioscopy completed in two 2-hour sessions with local anesthetic and microultrasonics. Initial debridement of heavy sub and supra tenacious calculus was removed using a Hu-Friedy H3 bladed piezo tip. Two-handed endoscopic debridement utilized a manual tune Tony Rizo magnetostrictive ultrasonic and 25 K universal tip that was able to adapt to all surfaces in the mouth.
- Enamel Pro Varnish Clear was placed on exposed root surfaces of Nos. 20, 29 to reduce possible sensitivity post-debridement.
OH instructions and recommendations:
- Recommended a power toothbrush such as a Sonicare or Braun. Patient has used a manual toothbrush only, no interproximal care. I demonstrated proper brushing using a soft toothbrush and Proxabrush for interdental cleaning.
- Recommended an oral irrigating device such as Shower Floss or H2 Oral Irrigator. Because this patient previously used only one OH device, I did not want to overwhelm her with OH tools. Having an irrigator already in the shower makes daily irrigating easy.
- A sample of Sensodyne was dispensed for possible sensitivity post-debridement.
- Fluoridex Sensitive was dispensed for caries control and possible sensitivity issues with instructions for daily use in the evening prior to bed.
- Post-treatment instructions dispensed and three Advil for post-treatment discomfort.
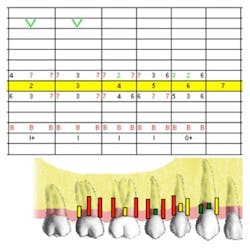
Seven weeks’ post-treatment perio charting
Click here to view remaining charts
Conclusion
- Overall improved dentition
- Pockets 2-4mm, no BOP, tissue pink and firm
- Improved personal oral hygiene
- Selective extractions on hopeless teeth Nos. 16,17, 24
- Patient is thrilled with outcome and is ready to move forward with orthodontics prior to permanent restorative dentistry
- 3-month periodontal maintenance
Suzanne and Dr. Bob are co-therapists and teamed up successfully for initial therapy. From an evidence-based perspective, they chose conventional initial therapy for patients with periodontal disease and the “gold standard” of meticulous scaling and root planing with ultrasonic instrumentation, assisted by a dental endoscope that magnifies dental tooth/root anatomy and subgingival calculus.
Dr. Bob prescribed systemic antibiotics, and in reviewing the literature on the effects of various systemic antibiotics on various clinical outcomes, there is still confusion about clinical benefit and the advantages and disadvantages of antibiotic use. There are no uniform guidelines for the administration of systemic antibiotics, including microbial testing, and there is also concern about antibiotic resistance.
In traveling around the U.S. and observing different periodontal protocols for initial therapy, I marvel at the different approaches in personalizing care, but it also concerns me that there is so much confusion about the effectiveness of adjuncts such as soft-tissue lasers, subantimicrobial dose doxycycline (SDD), or localized and systemic antibiotics. A decision whether or not to use an adjunct or some new technology must be based on evidence for clinical efficacy, and it’s sometimes hard to sift through the journal articles and manufacturer’s claims.
Learning how to weigh the strength of the evidence for clinical efficacy, taking into consideration the temptation of being constantly on the cutting edge of diagnostics and new technology, is a challenge that oral health-care professionals are just now meeting.
Suzanne and Dr. Bob chose a tried and true approach to initial therapy for this particular patient, and Suzanne customized self-care recommendations for biofilm control and desensitization. The results speak for themselves.
Lynne Slim is an award-winning dental author who has published extensively in dental/dental hygiene journals. In 2003, Lynne founded Perio C Dent, a dental practice management company that specializes in the incorporation of nonsurgical periodontal therapy into the hygiene department of the general dental practice. She is also the owner and moderator of the periotherapist yahoo group at www.yahoogroups.com/group/periotherapist. She also lectures on the topic of nonsurgical periodontal therapy and evidence-based decision making in dentistry. Lynne can be reached at: [email protected] or www.periocdent.com.