The clock is king
Time management that doesn't shortchange the patient
by Lynne Slim, RDH, MS, and Rhonda Jones, RDH, BS
Many dental practices are hurting financially because new patient numbers are down and patients are foregoing care to save money. In talking to Dr. Charles Blair, practice management consultant, PPOs have increased about 60% on a national level, and that means that fees are discounted about 35%, but this percentage is variable. Fighting back in troubled economic times means focusing on efficiency and reducing expenditures, and many dental practices with good business models are proactively looking for ways to increase revenues. Time management is an important piece of the formula so that patients are not shortchanged.
Managing time
"I just know I'll run behind and probably won't have enough time for my SRP," says Kayla, RDH, as her patient, Mrs. Chatterton, bounces in with her 12-year-old hyperactive son. Unfortunately, Mrs. Chatterton views each visit as a social hour. The receptionist only scheduled 30 minutes for Miguel, which isn't enough time. Kayla is 20 minutes late in seating her SRP patient, and the office manager only allotted one hour for two quadrants.
Then in walks Mrs. King, and Kayla knows nothing about her. The practice doesn't huddle in the morning and there's no daily review of online charts. The office manager tells Kayla she is going to do the UL/LL quads. Kayla is already concerned about not having enough time to anesthetize, meticulously debride, educate the patient about chronic periodontitis, and introduce self-care measures. She clicks on the patient's online perio chart and learns that periodontal charting hasn't been done.
Kayla starts charting and is back and forth from her operatory stool to the mouse. When she learns Mrs. King smoked for 20 years, she feels much worse about her remaining time as she falls into 6 mm to 7 mm pockets in posterior sextants.
While scaling with her ultrasonic, Kayla vividly remembers a former employer who taught his staff the importance of staying on time. He would raise both arms straight above his head like he was signaling a touchdown and shout, "The clock is king!" To him, being on time was critical. If the patient was not seated on time, the doctor became very agitated. He figured his time is important and the patient's time is important, and he was very focused on time management.
If you've earned an A+ on professional punctuality, then pat yourself on the back. If, however, you've struggled at times to manage your patient schedule, read on.
Being punctual for each hygiene appointment shows a healthy respect for your patients and yourself. We all want a professional reputation as someone who is prepared, organized, compassionate, skilled, and respectful. When we allow ourselves to be excused for chronic tardiness, it reflects poorly on our professional image and prevents the practice from reaching its full potential. If time management results from improper scheduling, this should be discussed between you, the dentist, and the office manager.
The best place to start with time management is with your work habits. You cannot create more time but you can work more effectively. Start by analyzing your current work habits that reduce your productivity.
- Morning huddles – Time is money but inadequate time leads to poor quality care and unhappy teams and patients. Make sure charts are reviewed for inconsistencies, potential problems, health alerts, incomplete treatment, and special needs. The unfortunate situation with Kayla and Mrs. King could have been avoided if Kayla had been scheduled differently or received assistance. One quadrant of SRP instead of two could have been treatment planned in the one-hour appointment, especially since Kayla had to perio chart and educate the patient.
- Texting/Internet use – Even if social media networking is condoned in your place of work, it can greatly reduce your momentum. Limit personal communication and networking. Checking email, taking personal phone calls, and texting or posting on Facebook can really eat away at the minutes in a hygiene schedule. Even old-fashioned face-to-face social networking between staff members in the office can be a viable threat to productivity. Practice self-regulation, and monitor and restrict your social contacts so that you set a professional example in the office.
- Fetching – Start each clinical day with a fully stocked operatory. Everything you could possibly need should be within arm's reach. Use unit-dose items and preset clinical trays with everything you need for any hygiene appointment. Having to leave the operatory to retrieve an item is a waste of valuable time. Take time to evaluate an organizational inventory of your operatory. Is it organized for efficiency? Are all the items needed for patient care, education, and infection control available? Make a list of the items you fetch throughout the week, and then incorporate those things into your operatory inventory.
- Be a clock watcher –If you tend to run late and struggle with this on a regular basis, you can overcome it with concentration and determination. Become a clock watcher and find one you can check regularly. It may be a bling bling watch or your cell phone or a wall clock – whatever jazzes you. Place the timepiece in your direct line of vision during patient care to help you stay on schedule. Visual time reminders help you stay focused. Never seat one patient without making a clear and strong mental note of your next patient's appointment time. The next appointment should always be present on your mind's radar.
- Interrupted doctor exam – Waiting for the doctor for more than 10 minutes is likely one of the most stress inducing problems for a hygienist who is working hard to stay on schedule. While some doctors are very time conscious, others are not, but sometimes even time conscious doctors get caught in a procedure they cannot leave. One of the best habits you and your doctor can develop is the interrupted doctor's exam. Once you have updated the medical/dental history, taken radiographs, and finished gathering and documenting information, let the doctor know you're ready for his or her exam. This should occur within 15 to 20 minutes of the patient's appointment time rather than waiting until after scaling and polishing. When the doctor and hygienist are trying to develop this habit it is a good idea to involve the dental assistants. They can be valuable support by reminding the doctor to check all hygiene patients before starting the next patient.
In a true assisted hygiene model with a dedicated assistant, the dental assistant and dentist can handle the radiograph/exam schedule that will allow the hygienist to focus on uninterrupted oral hygiene services.
Seeing every patient on time
Stuff happens. Patients run late, talk way too much, ask 1,000 questions, gag, throw up, have to take a call; you name it, it happens in a dental operatory. If your office uses an automated marketing and communication company such as Demandforce, where patients provide feedback that is posted to the worldwide web, it's important to keep patients happy. Your online reputation is at risk if you don't, and that's something new for dental practices to worry about. Patients subtract significant time from your schedule, but it's important to make every effort to seat the next patient on time.
Most of the time things work out, especially if team members pitch in when you're in a pinch. For example, an assistant might review the next patient's medical history, check for unscheduled treatment, take intraoral photos, and call the dentist in to determine radiographic needs and complete an exam. The most effective way to deal with lost time is to subtract time from each segment of care remaining, but sometimes that's not possible. For example, five minutes off the allotted time for scaling and five minutes off polishing time can correct the lost time for a patient who showed up 10 minutes late. Sometimes it might just mean less chatting with the patient. Whatever you do, never shortchange the patient on debridement of biofilms because disruption of biofilms almost always results in reduced inflammation.
Some patients with a healthy periodontium have issues with staining, above average accumulation of calculus, or poor oral hygiene habits that eat up instrumentation/polishing time. When the treatment time exceeds the time allotted for a preventive appointment, the clinician must step in to educate the patient about his or her unique dental needs, and that more frequent recare visits are needed to allow for optimum preventive care.
One of the biggest time savers you have control over is using a piezoelectric or magnetostrictive ultrasonic unit. (This assumes you have such a unit. If you don't, you may want to purchase your own, but a reputable practice will give you the tools you need to do a superior job.) Power-driven scalers can increase tactile sensitivity, significantly improve calculus removal in deeper pockets, improve operator ergonomics, disrupt biofilm, increase patient comfort, remove less root surface than hand instrumentation, improve furcation access, and reduce scaling time by about 36.6%.1 Ultrasonic tips/inserts just keep getting better. Improvements include improved subgingival access and better adaptation to tooth/root anatomy, including line angles. Bottom line – make ultrasonic instrumentation a priority in biofilm and calculus removal.
Strongly consider using hand instruments that eliminate time-consuming instrument sharpening. American Eagle's sharpen-free XP technology curettes are an example of hygiene instruments that are treated with a patented nano technology process that hardens the stainless steel and then encapsulates it. This makes a diamond-like edge that lasts months without sharpening. Also consider trying some of the newer universal curettes such as American Eagle's XP technology Scandette with two cutting edges that adapt to mesial and distal surfaces. Use of all-purpose curettes save time and money.
Periodontal exam/documentation
There are many ways to get the periodontal exam done efficiently, but if you do not have an automated recording unit, here are a couple of low-tech, low-cost ideas to help you cut down on your periodontal charting time. While probing, select a probe such as Hu-Friedy's Colorvue, which provides enhanced visibility through color contrast. Don't waste precious time recording periodontal data on your own. Use a simple, inexpensive digital recorder that can be found for under $50. If you are working in an assisted hygiene model, the assistant can record from the recorder to the computer software.
Always probe circumferentially. (It's NOT about spot or point probing. Point probing is passé and was replaced by circumferential probing back in the early 1980s.2 Walk the probe around the circumference of a tooth while keeping it in the sulcus and record the deepest reading in six segments. Always record recession and track clinical attachment loss (CAL).
Take the time to record bleeding on probing, mobility, and furcation involvement. If you don't know how to record and interpret CAL and furcation involvement, ask a local periodontist for help. Discuss the clinical significance and treatment implications for posterior teeth with mobility furcation involvement.
Periodontitis (according to case type and whether or not it is chronic, aggressive or refractory, generalized or localized) should be diagnosed in writing by the dentist, and make sure the team has developed criteria for referral to a periodontist. Risk analysis for periodontitis is a critical assessment piece that can be rapidly completed when using risk assessment software such as PreViser.
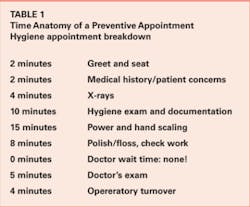
Let's look at breakdown of time in the preventive hygiene appointment. (See Table 1) While each clinician will vary on the time spent on each section of an appointment, this list should help identify average treatment times. It may help to use these categories to perform a time audit of hygiene procedures so you can understand where your time is spent and help you redirect your focus in patient care. It can also help the team understand your time constraints so they can help you stay on schedule.
Sometimes well meaning practice managers delegate duties to hygienists that take away from patient time, and this is a mistake that results in lower hygiene profitability. Not only is it stressful for the hygienist, it is unfair to the patient, who deserves quality, uninterrupted care. Checking out a patient from the operatory is not within the scope of dental hygiene duties, and neither is working on the recare system. Hygienists are primary care providers, not auxiliaries, and they need assistance to do their jobs well. If there's a hole in the daily schedule, a dental hygienist/team player should pitch in. Even tray set-ups can be delegated to an assistant so the hygienist can focus on relationship building and delivering clinical services.
Rhonda Jones, RDH, BS, is a practice-management consultant with a unique and practical perspective in practice growth and team dynamics. She is president of Anderson & Associates, a firm that holds firmly to the belief that the dental staff is the most valuable resource in the dental practice. Rhonda can be reached at [email protected].
Lynne Slim, RDH, BSDH, MSDH, is an award-winning writer who has published extensively in dental/dental hygiene journals. Lynne is the CEO of Perio C Dent, a dental practice management company that specializes in the incorporation of conservative periodontal therapy into the hygiene department of dental practices. Lynne is also the owner and moderator of the periotherapist yahoo group: www.yahoogroups.com/group/periotherapist. Lynne speaks on the topic of conservative periodontal therapy and other dental hygiene-related topics. She can be reached at [email protected] or www.periocdent.com.
References
1. Tunkel J, Heinecke A, Flemming TF. A systematic review of efficiency of machine-driven and manual subgingival debridement in the treatment of chronic periodontitis. J Clin Periodontol. 2002;29 Suppl 3:72-81; discussion 90-91.
2. Hollister LP. Periodontal probing in the clinical detection of periodontal pockets. J Dent Hyg. 1979; 53(12): 555-558.
Past RDH Issues