An exposure for systemic sequelae
by Karen Davis, RDH, BSDH
[email protected]
In a recent interview with Casey Hein, BSDH, MBA, we talked about some aspects of how the periodontal team is incorporating oral-systemic health information in this country and in Canada.
Casey, you were researching, writing about, and discussing oral-systemic health long before most clinicians even thought about it. Can you give us a synopsis of what your most recent endeavor has been regarding this topic?
Hein: First, Karen, I don’t consider myself an expert, but I am very passionate about periodontal-systemic science. I believe that the mounting evidence of oral-systemic relationships provides an unprecedented opportunity for dental hygienists to redefine their role within the healing arts. Thanks for the opportunity to share my thoughts and some of the work I’m doing.
As many of your readers know, about five years ago, PennWell partnered with me to launch Grand Rounds in Oral-Systemic Health, the first journal to focus exclusively on clinical implementation of emerging evidence of oral-systemic relationships. In 2007, I was recruited by Dr. Tony Iacopino — at that time the newly appointed dean of the Faculty of Dentistry at the University of Manitoba — to help develop the International Centre for Oral-Systemic Health (ICOSH).
As the director of education for ICOSH, my first priority was to carry out the vision for the creation of a curriculum about oral-systemic health for nondental health-care providers (HCPs) — physicians and nurses, for example, among others.
In recent years, authoritative bodies representing education in medicine and dietetics have recommended that curriculum in undergraduate and graduate education of nondental HCPs be re-formed to include oral-systemic science.1-4 The online, multimedia Curriculum in Oral-Systemic Health for Nondental Healthcare Providers at the University of Manitoba is the first comprehensive, interprofessionally vetted curriculum about oral health for nondental HCPs.
We expect to launch the first two modules of the online curriculum for students with the University of Manitoba by the end of the year. The curriculum will be especially welcome in countries where access to dental care is severely limited. Given the appropriate education and training, physicians and nurses could make a major difference in oral health outcomes of underserved populations. In September, we were excited to hear that an external funder gave the university an additional $500,000 to continue the curriculum project.
I’m also excited about the launch of www.caseyhein.com later this year. Under development for almost two years, this website will offer a generous library of free resources related to periodontal-systemic health, novel tools for screening and referral of at-risk patients, and resources for building collaboration with physicians and nurses. In addition, we’ll be integrating rich, case-based discussion forums, and multimedia, accredited continuing education for oral HCPs as well as nondental HCPs (physicians and nurses). I hope your readers will check out www.caseyhein.com in a few months.
What comes to mind as the two or three most important concepts you believe dental team members need to understand related to the perio-systemic connection?
Hein: First, stop thinking of periodontal disease as a local infection, and start thinking of periodontal disease as an exposure event for systemic sequelae. About 10 years ago, Offenbacher and Beck provided a compelling rationale for thinking of periodontal disease as an exposure event. “Periodontal disease must be thought of as a disease process that is an exposure for a systemic disease or condition rather than the outcome itself.”5
Today, we recognize that periodontal tissues serve as a portal for infectious dissemination systemically. Not only do oral bacteria induce inflammatory responses at the local site of periodontal infection, but they also interact with other tissues in the body once they overcome the local host defenses and disseminate throughout the vascular tree. This is what is implicated in exacerbating ongoing inflammation in distant organs, and increasing risk for complications of diabetes, coronary heart disease, adverse pregnancy outcomes, and respiratory diseases, among others.
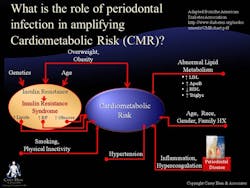
Secondly, consider how untreated periodontal disease may increase cardiometabolic risk (CMR) (see Figure 1). This concept is highly relevant as the majority of the adult population has some level of CMR. The term “cardiometabolic risk” describes a set of risk factors that, when viewed together, are good indicators of a person’s overall risk of developing heart disease and type 2 diabetes. These risk factors include obesity, high LDL (“bad”) cholesterol, high blood fat (triglycerides), low HDL (“good”) cholesterol, high blood pressure, smoking, and physical inactivity. Each risk factor poses a danger to good health, and the more someone has, the greater the risk of heart disease and type 2 diabetes.
In the lower right-hand corner of the figure, inflammation and hypercoagulation have been implicated as a component of CMR. We know that infection from any source is one of the things that precipitates inflammation. It is in this light that we must consider the contribution of infections of the oral cavity, including periodontal diseases. The CMR model allows oral HCPs to see the bigger picture and focus on the recognition and treatment of all risk factors, including infections of the oral cavity, such as periodontal diseases, to help our patients achieve better health outcomes.
Finally, do not be misled by studies that suggest that treatment of periodontal disease does not affect health outcomes. The truth is that the jury is still out on this. Right now, we simply do not know. A good example of this truth is the obstetrics and periodontal therapy study.6 This study, published in the New England Journal of Medicine in 2006, failed to demonstrate a difference in the rates of preterm birth, low birth weight, or fetal growth restriction following treatment for periodontal disease.
However, what we must realize is that in clinical trials such as this one, treatment protocols are specifically prescribed. Unlike the latitude private practitioners have in determining treatment regimens for individual patients, practitioners providing treatment in clinical trials cannot depart from carefully prescribed protocols. During a recent focus group I conducted at the University of Manitoba, one of the most highly respected obstetricians in Canada noted — as other researchers have suggested — that failure to demonstrate a treatment effect does not rule out an association between periodontal disease and adverse pregnancy outcomes. Obstetricians and nurses who participated in this focus group stated that the emerging evidence of the threat periodontal disease poses to pregnancy will definitely influence how they care for women.
A challenge for all of us in the dental profession is better collaboration between the medical and dental community in reduction of risk factors that impact both periodontal and systemic health. What suggestion do you have for dental hygienists to make a difference in this area?
Hein: Over the last four to five years, evidence of periodontal-systemic relationships has increasingly been reported in some of the most highly respected medical journals around the world. Consequently, our colleagues in medicine, nursing, diabetes education, pharmacology, and other disciplines are becoming “primed.” As oral HCPs, what we must now do is learn the science well enough to articulate it accurately, and without hesitation to our nondental colleagues. This is not a one-shot deal. Not only do we have to initiate these types of interprofessional relationships, but we need to nurture them over time.
There are many great strategies for doing this, and I hope your readers will take advantage of these kinds of learning resources at www.caseyhein.com.
Thank you, Casey, for this timely and substantive input on a topic we are all striving to better understand.
References
1. US Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, National Institute of Dental and Cranial Research, National Institutes of Health; 2000.
2. Curriculum and Clinical Training in Oral Health for Physicians and Dentists: Report of a Panel of the Macy Study. American Dental Education Association 2008; Accessed October 16, 2008 at http://www.adea.org/publications/Documents/MACY%20REPORT%202.pdf
3. Report IX; Contemporary Issues in Medicine: Oral Health Education for Medical and Dental Students. Medical School Objectives Project; American Association of Medical Colleges; June 2008. Accessed October 16, 2008 at https://services.aamc.org/Publications/showfile.cfm?file=version116.pdf&prd_id=238&prv_id=289&pdf_id=116
4. Position of the American Dietetic Association: Oral Health and Nutrition J Am Diet Assoc. 2007; 107:1418-1428.
5. Beck JD, Offenbacher S. Relationships among clinical measures of periodontal disease and their associations with systemic markers. Ann Periodontol 2002;7:79-89.
6. Michalowicz BS, Hodges JS, DiAngelis AJ, et al. Treatment of Periodontal disease and risk of preterm birth. N Engl J Med. 2006;355:1885-1894.
An exposure for systemic sequelae
Karen Davis, RDH, BSDH, is the founder of Cutting Edge Concepts, an international continuing education company, and practices dental hygiene in Dallas, Texas. She is an independent consultant to the Philips Corp. and serves on the review board for Dentalantioxidants.com. She can be reached at [email protected].
Past RDH Issues