How dental hygienists can help patients with thyroid disease
Dental professionals can overlook thyroid disease easily. When reviewing medical histories, dental professionals often focus on heart and lung conditions, high blood pressure, cancers, past and recent surgeries, and diabetes. Reviewing a patient’s medical history for all endocrine and autoimmune diseases is just as important. Thyroid disease has oral manifestations that should be taken into consideration before, during, and after any dental treatment.
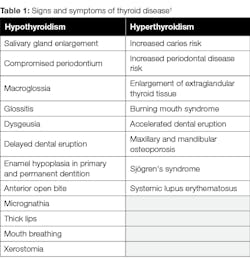
Thyroid dysfunction is the second most common glandular disorder of the endocrine system and is common among women.1 Many patients go undiagnosed or have disease that is not well controlled. Dental professionals should be aware of the oral and systemic manifestations of thyroid disease so they can best treat the patient. If uncontrolled or undiagnosed thyroid disease is expected, it is important to contact the patient’s primary-care physician or endocrinologist prior to any elective oral procedures. Table 1 describes the signs and symptoms of thyroid disease.
Hypothyroidism
Hypothyroidism is caused by a decrease in thyroid hormone production and thyroid gland function. In addition to those listed in Table 1, other characteristics include weight gain, intolerance to cold, dry and cool skin, swollen face and eyelids, and normal blood pressure with a slow heart rate. People who have Sjögren’s syndrome, pernicious anemia, iron deficiency, type 1 diabetes, rheumatoid arthritis, and lupus are at risk of developing hypothyroidism.1
Hashimoto’s disease, in which the immune system attacks the thyroid, is a common form of hypothyroidism.2 Other forms and causes include thyroiditis, congenital hypothyroidism, radiation treatment of the thyroid, medications, and removal of all or part of the thyroid.
Prior to dental procedures, certain considerations should be evaluated. Patients with hypothyroidism may have lack of hemostasis and are at increased risk for infection due to decreased metabolic activity in fibroblasts. The possibility of delayed healing time is important to consider to prevent infection. Patients who have hypothyroidism are also at risk for heart disease.
Hyperthyroidism
Hyperthyroidism is caused by unregulated production of thyroid hormones and is characterized by tremors, intolerance to heat, sinus tachycardia, hypertension, increased appetite, and weight loss. A patient is at risk for hyperthyroidism if he or she has a family history of thyroid disease; has other systemic conditions, such as pernicious anemia, type 1 diabetes, or primary adrenal insufficiency; consumes large amounts of iodine; is over 60; is female; and/or has been pregnant in the last six months.
Graves disease, an autoimmune disease in which the immune system attacks the thyroid and causes it to produce too much thyroid hormone, is the most common cause of hyperthyroidism. Patients with hyperthyroidism can have an elevated blood pressure and pulse and therefore may experience increase bleeding. Elevated levels of thyroid hormones can cause patients to be extremely sensitive to sympathomimetic drugs such as epinephrine, which is used in dentistry as a vasoconstrictor in local anesthesia and retraction cords.3
It is important to note that patients who have hyperthyroidism have increased levels of anxiety and stress, and being in the dental office can trigger thyroid storm. Thyroid storm is characterized by high pulse rate, high blood pressure, and high body temperature, and it is often life threatening. If thyroid storm is suspected, dental procedures should be delayed and emergency services called.
Periodontal disease and caries risk
As we know, periodontal disease is an inflammatory process. Numerous systemic diseases have been linked to periodontal disease officially. Thyroid disease can lead to homeostatic imbalance in the body, which affects the healing abilities of tissue. Thyroid disease has not been linked to periodontal disease officially yet, but there are numerous case studies that have shown a strong correlation between the two.4
Caries risk increases primarily due to decrease in saliva flow, which can increase the acidity of the saliva. This results in a rapid progression of caries. Sjögren’s syndrome is the most common disease causing xerostomia, but autoimmune thyroid diseases can also affect salivary glands. In a recent study, more than half of patients with xerostomia also had thyroid disease.5 Patients with high caries risk and Sjögren’s syndrome should be closely monitored at each visit.
Role of the dentist
Dental professionals are often the first to suspect a thyroid disorder that is uncontrolled and aid in early diagnosis or intervention for treatment. Dental complications can arise from uncontrolled or undiagnosed thyroid disease. It is important to communicate with the patient or with his or her doctor to find out how long the disease has been active and the current therapy in order to help prevent infection and a possible life-threatening cardiac event.
Cardiac events have been linked to thyroid disease. Taking the patient’s blood pressure and pulse at the start and end of a dental procedure is recommended. Dental treatment modifications are needed for patients who have undiagnosed or uncontrolled thyroid disease. A medically well-controlled patient doesn’t have any contraindications to dental treatment.
Role of the hygienist
Patients often see us more than the dentist and other doctors. We are on the forefront of patient care, so it is important to think about what you see while you’re cleaning the patient’s teeth in conjunction with thinking about his or her medical history. Do not be afraid to ask the patient in-depth questions or ask the dentist to get involved.
Talking to patients about products that can improve their signs and symptoms is needed at each recare visit. For example, patients with Sjögren’s syndrome might find it helpful to use a toothpaste and mouth rinse formulated for dry mouth. Colgate’s new Hydris mouth rinse and toothpaste have helped many dry mouth sufferers. Xylitol products are also great for patients who have oral manifestations of thyroid disease, such as caries and xerostomia.
Educating patients about products that can help with xerostomia while preventing caries is ideal. I often suggest several products and provide a list in order to help them find a product they like. It is important to follow up with patients and advise them to call if they have questions.
Talking to the patient
Recently, I have had a couple of patients who have presented with uncontrolled and/or undiagnosed thyroid disease with gingival inflammation and fast progression of caries. My first thought was, “Why?” At first glance, one might think that these patients didn’t have the best home care and dedicate the appointment to educating them on the importance of home care. But maybe it isn’t just because of poor home care—maybe there is a systemic condition causing poor oral health.
It is important to ask the patient outside-the-box questions. For example, you might ask if the patient has had recent blood tests; seen any specialists; had dry mouth, skin, or eyes; or had any signs or symptoms of systemic disease. Is there anything significant in the patient’s medical history?
Both of my recent patients had uncontrolled diagnosed thyroid disease. The dentist wrote letters to both patients’ doctors regarding the findings during their appointments so the patients would be reevaluated by their physicians.
In dentistry, it is important to ask yourself why. I call it “why dentistry.” It is very easy to have blinders on when treating a patient, and it is even easier to treat the problem itself instead of finding out what caused the problem in the first place. There are reasons why problems occur, and finding out those reasons can help prevent more problems in the future. Always think with the end in mind.
Conclusion
Regular communication between the dentist and patient’s endocrinologist is vital in helping the patient maintain and control thyroid disease. Dental professionals must remain up to date on thyroid disease and its oral and systemic manifestations. Looking for signs of uncontrolled systemic diseases at each recare visit can help patients improve their overall health. Don’t be afraid to ask questions and think outside of the box. Remember to always think, “Why?” Once you know the reason why, patient care improves. Dental hygienists can help patients by recommending oral care products based on the condition, advising patients to follow up with their physicians, and improving patients’ overall health.
Editor's note: This content was originally published in 2019 but has been updated as of January 2025.
References
1. Chandna S, Bathla M. Oral manifestations of thyroid disorders and its management. Indian J Endocrinol Metab. 15(Suppl 2):S113-S116.
2. Hypothyroidism (Underactive Thyroid). National Institute of Diabetes and Digestive and Kidney Diseases website. https://www.niddk.nih.gov/health-information/endocrine-diseases/hypothyroidism. Updated August 2016.
3. Hyperthyroidism (Overactive Thyroid). National Institute of Diabetes and Digestive and Kidney Diseases website. https://www.niddk.nih.gov/health-information/endocrine-diseases/hyperthyroidism. Updated August 2016.
4. Kothiwale S, Panjwani V. Impact of thyroid hormone dysfunction on periodontal disease. J Sci Soc. 2016;43(1):34-37.
5. Jung JH, Lee CH, Son SH, et al. (2016). High prevalence of thyroid disease and role of salivary gland scintigraphy in patients with xerostomia. Nucl Med Mol Imaging. 2017;51(2):169-177.
About the Author
Jessica Raymond-Allbritten, BASDH, CRDH
Jessica Raymond-Allbritten, BASDH, CRDH, practices dental hygiene at Lepore Comprehensive Dentistry in Dunedin, Florida. She was a member of the 2015 Colgate Oral Health Advisory Board, and she is currently a contributing author for the Colgate Oral Health Advisor web page. You may contact her at [email protected].