Nd:YAG Laser-Assisted Treatment of Periodontitis As a Manifestation of Systemic Disease
This case study was prepared for the Academy of Laser Dentistry for an advanced case study in March 2005. This case is still being followed and the patient is now maintaining without any pockets greater than 4mm. This serves as a guide through the required process for the Academy of Laser Dentistry’s advanced laser certification and an outline of the documentation that should be followed.
Diagnostic Tests
❏ Outline of case - This 80-year-old woman has been a patient of record since 2002. She needed to have some periodontal therapy completed, but was leery of starting treatment at her age. Following education about periodontal disease and the importance of overall health, she committed to visiting the hygienist more frequently to maintain her dental health.
In December 2003, the patient reported an aphthous ulcer, and was encouraged to have laser treatment. When she was convinced of the laser’s ability and safety, she scheduled an appointment.
❏ Medical history - The patient’s health history revealed that she had several areas of concern including abnormal blood pressure, allergies, diabetes, glaucoma, arthritis, artificial joints and/or pins in her left knee, and premedicating prior to dental appointments. She provided the office with a complete list of medications.
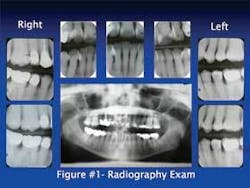
❏ Radiography examination - Panorex and seven vertical bitewings were taken (Figure1). The radiographs revealed moderate generalized horizontal bone loss with several areas of vertical bone loss on the anterior and posterior teeth. The crestal bone was absent on all teeth and furcation involvement was noted on tooth No. 30.
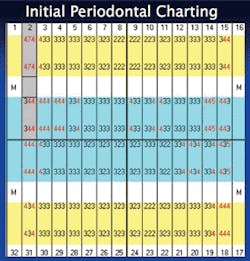
❏ Soft tissue status - Complete six-point periodontal charting was performed with localized 4 mm pockets being noted throughout the mouth. No recession was detected. However, localized bleeding was evident upon stimulation and Class II furcation was noted on the buccal of No. 30 (Figure 2).
❏ Hard tissue assessment - All third molars were listed as missing and all restorations were completed prior to the initial periodontal therapy. There was no mobility charted, and all teeth were vital. It was determined the patient needed an occlusal guard appliance to correct her occlusal disharmonies.
Diagnosis and Treatment Plan
❏ Diagnosis - The diagnosis of this patient was periodontitis as a manifestation of systemic disease.
❏ Treatment plan - The treatment plan included four, one-hour periodontal therapy appointments that would include:
• Health history review
• Blood pressure screening
• Topical and local anesthetic as needed
• Full-mouth micro-ultrasonic instrumentation with light hand scaling to provide bacterial decontamination
• Laser soft-tissue debridement and superficial coagulation
• Vitamin E applied to the tissues for rehydration and patient comfort, which also aids in healing
• Postoperative instructions
The six-week post-therapy appointment included:
• Six-point periodontal charting to track healing
• Micro-ultrasonic instrumentation to provide bacterial reduction
• Coronal polishing
• Laser debridement of the necessary area
• Determining an appropriate recare interval
❏ Treatment alternatives - Conventional scaling and root planing can be followed by periodontal surgery and frequent re-care visits that included more scaling.
❏ Indications for treatment - The tooth surface was prepared with ultrasonic scaling. The Nd:YAG laser is highly absorbed in melanin and hemoglobin, and both of these chromophores are present in inflammatory tissue. This laser helps reduce bacterial counts and achieve superficial coagulation to aid in healing. If periodontal disease is left untreated it will lead to tooth loss.
❏ Contraindications for treatment - It is important that the laser beam from the Nd:YAG laser is directed away from the tooth structure.
❏ Informed consent - It is essential for the dentist to receive informed consent. The 80-year-old patient was educated in the progression of periodontal disease and given both a verbal and written treatment plan. The patient verbally agreed to treatment, then signed the consent form and scheduled treatment and follow-up appointments.
Treatment
❏ Treatment objectives - The treatment objectives were to reduce the bacterial population, decrease probing depths, eliminate bleeding, stop the apical migration of the gingival margins and epithelial attachments, and provide oral hygiene instruction.
❏ Instrumentation - A free running pulsed Nd:YAG laser (PulseMaster, American Dental Technologies, Corpus Christi, Texas) with a 1,064nm emission wavelength was used in a contact mode with a 300 micron fiber. For bacterial reduction, the laser parameters were 30mJ and 60 Hz, average power of 1.8 watts. For superficial coagulation, the settings were 100mJ and 20 Hz with an average power of 2.0 watts. The total laser emission time for the four treatments was 24 minutes.
❏ Treatment sequence - The treatment for each therapeutic appointment included: (Figures 3, 4, 5)
• Premedication with antibiotics because the patient had knee replacements
• Health history review
• Blood pressure screening
• Chlorhexidine 0.12 percent preprocedural rinse
• Pre-, peri- and postoperative photographs
• Patient completed therapy without topical or local anesthetic
• Micro-ultrasonic instrumentation and light hand scaling
• Laser debridement with superficial coagulation
• Vitamin E applied to the tissues for rehydration and patient comfort
Laser safety measures were considered, and included:
• Specific eyewear for the Nd:YAG laser
• 0.1 micron filtration mask
• Environment protection to limit access
• All safety issues, including posting warning signs
• Minimizing reflective surfaces
• High volume evacuation utilized for plume control and to help cool the tissue
• Chart documentation
The laser fiber was cleaved and the laser was test fired. The fiber was calibrated to 1mm less than the pocket depth, and the fiber remained in constant contact with the gingival tissue, starting at the top of the pocket and then moving vertically and horizontally until the calibrated depth was reached. Care was taken to be sure that the fiber was directed away from the tooth structure. Any accumulated tissue was wiped away from the fiber to be sure a proper cleave was maintained (Figures 6, 7).
❏ Postoperative procedures - The patient was provided with written postoperative instructions. This included avoiding crunchy, acidic, and rough foods for the first 24 hours to prevent debris from lodging under the tissues.
The healing process is the most important process of the procedure; therefore, it is important for the patient not to dislodge the blood clot that forms around the pockets. The patient was instructed to be careful with the use of an electric toothbrush, rubber tip stimulator, and subgingival flossing for one week.
❏ Complications - The patient had no complications during or after the laser treatments.
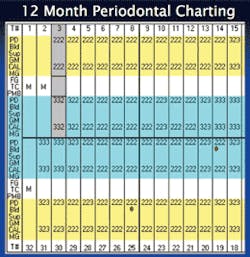
❏ Long-term results - At three months, the patient had reduced pocket depths, but her oral hygiene care was still a concern. At six months, there was overall improvement with the exception of tooth No. 2. Endodontic therapy was diagnosed on this tooth, but the patient elected to have the tooth extracted. The patient was improving at her nine-month appointment, but there was still concern about her oral hygiene. The staff reinforced her commitment to appointments every three months for her periodontal maintenance. At her 12-month appointment, the patient had progressed with her oral hygiene care and had finally committed to a daily routine. Her periodontal charting showed results at this appointment, and so did her smile. She is currently continuing with three-month periodontal maintenance.
Prognosis
The patient was compliant with all aspects of her care, so her prognosis is good. All this is contingent on the following:
• Diabetes control
• Oral hygiene maintenance
• Continued use of Oral-B toothbrush
• Daily use of brush-on fluoride
• Scheduling the recommended three-month periodontal maintenance
The final charting pictures show the comparison of initial treatment and the last recorded treatment (Figures 8, 9, 10). The decreased depth of the pockets and the appearance of the gingival tissue should be noted. This case shows successful periodontal therapy. However, since periodontal disease can be manifested in cycles, the practitioners and patient must strive to maintain a good continued-care program.
Author acknowledgement: A special thank you to Nora Rafetto, RDH, for all of her advice with this article.