Diabetes Mellitus
by Deborah M. Lyle, RDH, MS
Diabetes mellitus (DM) is a group of metabolic diseases characterized by altered glucose tolerance or impaired lipid and carbohydrate metabolism. Diabetes affects an estimated 17 million people in the United States or 6.2 percent of the population. Of the 17 million, an estimated 5.9 million people are unaware that they have the disease. Diabetes is increasing at epidemic proportions and is a costly chronic disease. The increasing incidence of DM is due in part to the growing number of older Americans, the prevalence of obesity, and sedentary life styles. In 1997, the per capita health care cost was $10,071 for diabetics as compared to $2,699 for those without diabetes.
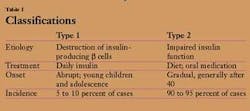
The American Diabetes Association currently classifies diabetes into three major types based on etiology. Type 1 diabetes (formerly known as juvenile or insulin-dependent diabetes mellitus) is caused by the autoimmune destruction of the insulin-producing b cells of the pancreas. Type 2 diabetes (formerly called noninsulin-dependent diabetes mellitus) is caused by impaired insulin function, which may be caused by a defect in the insulin molecule or from altered cell receptors for insulin. Type I results in no insulin production and Type 2 results because the body is unable to utilize the insulin that is produced (see Table 1).
Gestational diabetes, the third classification, may also occur, and is an abnormally high blood glucose level in pregnant women who do not have a previous history of diabetes. Gestational diabetes develops in approximately 4 percent of pregnant women or about 135,000 cases in the United States each year.
The medical condition, prediabetes, was established by the American Diabetes Association in 2002 and refers to a high blood glucose level that is below the threshold of a definitive diagnosis of diabetes. It is estimated that about 16 million people (15.6 percent) in the United States between the ages of 40 and 74 have pre-diabetes. Recent research has shown that interventions targeted at controlling blood glucose levels can delay or prevent Type 2 diabetes. A host of other types of diabetes may result from specific genetic disorders, surgery, medications, and infections, or associated with diseases of the pancreas.
Signs, symptoms, and complications
The general signs and symptoms of DM are related to hyperglycemia and include the triad of polyurea, polydipsia, and polyphagia, along with pruritis, weakness, and fatigue. Weight loss and ketoacidosis are generally associated with Type 1 diabetes. Prolonged hyperglycemia may produce complications such as retinopathy, possibly leading to blindness, atherosclerotic cerebrovascular, cardiovascular and peripheral vascular diseases, peripheral neuropathy with possible loss of limbs, progressive renal dysfunction, and impaired wound healing (see Table 2).
There are several risk factors for diabetes mellitus. The following should be considered when reviewing medical histories:
• 45 years of age and older
• Family history of Type 2 diabetes in parent or sibling
• Obesity — weight greater than 120 percent of desirable body weight
• Ethnicity — Hispanic/Latino, Native American, African American, Asian American, Pacific Islander descent
• History of impaired glucose tolerance or impaired fasting glucose
• Hypertension or dyslipidemia
• History of gestational DM or delivering a baby weighing more than nine pounds
Medical treatment of DM is designed to control blood glucose levels and to prevent the symptoms and complications associated with the disease. Type 1 diabetes requires insulin therapy, which is available in multiple formulations. Type 2 diabetes can be controlled by diet and weight loss, with the addition of oral drugs to stimulate insulin release and promote uptake in the tissues when necessary.
Some researchers have investigated whether periodontal infections contribute to problems with glycemic control. The elimination or improvement of oral infections has led to improved glycated hemoglobin blood levels in some studies. The evidence is inconclusive at this time but warrants further study due to the increased severity of oral infection, especially in uncontrolled or poorly controlled individuals.
Oral manifestations
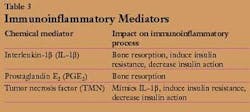
Periodontal diseases are chronic bacterial infections that affect the tissues of the periodontium and cells active in the immunoinflammatory response. Data support the concept that in diabetes-associated periodontitis, the altered host inflammatory response plays a critical role. Polymorphonuclear leukocytes (PMN) are a first line of defense in the immunoinflammatory process. A reduced PMN function has been found in patients with diabetes, exposing the host to an increased risk of bacterial invasion and subsequent upregulation of destructive chemical mediators such as interleukin-1b, prostaglandin E2, and tumor necrosis factor (see Table 3).
Some diabetic patients have significantly higher gingival crevicular fluid levels of both PGE2 and IL-1b as compared to those without diabetes. Diabetes can also increase the production of TNFa. This may lead to greater attachment loss and alveolar bone destruction.
Oral manifestations of DM were first described more than 100 years ago. Findings include gingivitis, periodontitis, bone and tooth loss, and soft tissue pathologies. The increased susceptibility to periodontal infections is generally seen in poorly controlled or uncontrolled diabetics and does not necessarily correlate with increased plaque or calculus. Uncontrolled and controlled Type 2 diabetics have a higher incidence and more severe bone loss than non-diabetics.
The reduction of salivary flow leading to xerostomia is a common oral finding and may be accompanied by burning mouth or tongue syndrome and enlargement of the parotid glands. Tissue may be more susceptible to trauma and opportunistic infections such as candidiasis due to the reduced salivary flow. An increase in caries is sometimes seen in poorly controlled or uncontrolled DM individuals. However, in well-controlled individuals with good oral hygiene, the incidence of caries is equal to or lower than non-diabetics.
Periodontal treatment considerations
Several studies have evaluated different modes of treatment in diabetics with varying levels of periodontal infections. The combination of systemic antibiotics and topical antimicrobials, along with scaling and root planing, has resulted in pocket reduction and clinical attachment gains in individuals with both uncontrolled diabetes and severe periodontal disease. Nonsurgical therapy has also been successful, but it is important to note that in some cases there was a more rapid recurrence of pocket formation in uncontrolled diabetics, especially in the absence of maintenance therapy.
The compromised immune response, glycemic control, early intervention, and awareness of the impact on oral health contribute to the success of therapy. Continued care, patient education, and meticulous home care are vital. Control of the dental biofilm can be difficult for many patients, but the threshold for the initiation of infection is greater in those who are immunocompromised.
The addition of devices, techniques, and antimicrobials to improve self-care results may be imperative. Powered toothbrushes are an excellent way to improve supragingival plaque control. The multitude of brushes makes it easy to find a product that the patient likes and can afford.
Interproximal removal of the plaque biofilm can be enhanced when the right product is recommended. Manual floss is effective but compliance is generally low. Interproximal brushes, wood sticks, or powered flossers are effective alternatives. Recommending home oral irrigation will help address the increased production of destructive chemical mediators as evidenced by the reduction of GCF levels of PGE2 and IL-1b, along with reduction of gingivitis, bleeding on probing, and pathogenic bacteria. Specifically, a recent study showed that diabetics fared better when they added oral irrigation to their home care routine.
Fluoride therapy and palliative treatment for xerostomia should be included in the treatment plan if the patient presents with abnormally high caries or complains of dry mouth.
Treatment for DM will vary, depending on the type of diabetes and risk factors. Other than glycemic control, treatment considerations include nutritional counseling, exercise, stress reduction, smoking cessation, and monitoring of blood pressure and blood lipid levels.
The dental professional may be the first to notice early signs of DM, especially since many individuals are undiagnosed. Thorough documentation of medical treatment and glucose levels, including type of diabetes, medications, frequency of testing, and current symptoms is imperative. Consultation with the treating physician will support the development of a comprehensive treatment plan that meets the patient's specific needs. Education should include the impact on the oral environment and the relative risk for periodontal disease. Monitoring the patient for any signs of complications may prevent a medical emergency.
Diabetes mellitus is a common metabolic disorder that will affect many of the patients in your practice. Individuals with diabetes will present with an array of clinical and oral findings that need to be evaluated along with a comprehensive medical history. The altered host response helps explain the severity of periodontal infections, especially in uncontrolled, poorly controlled or undiagnosed individuals.
The dental hygienist may be the first health care provider to identify the need for a medical consultation due to symptoms or oral findings presented. Treatment plans need to include comprehensive self-care techniques that control the dental biofilm and modulate the host response. It is important to treat the whole patient and not just the specific oral findings he or she may present. Treatment outcomes improve with correct diagnosis and compliance to both medical and dental interventions.
Deborah M. Lyle, RDH, MS, is currently employed by Waterpik Technologies as the manager of professional marketing and education. She has presented numerous continuing education programs both nationally and internationally. Lyle also is a member of the ADHA Council on Education. She may be reached at [email protected].