Identifying and responding to child abuse and neglect
In 1874, neighbors reported the cries of a severely abused orphan named Mary Ellen Wilson to the New York City authorities. A charity worker along with the founder of the Society for the Prevention of Cruelty to Animals (SPCA) posed as census workers to investigate the allegations of abuse against the nine-year-old. At this time, there were already laws in place to protect children, and even domestic and farm animals, from abuse and remove them from dangerous homes. But the reality was that most, even those in law enforcement, were reluctant to intervene.
Laying eyes upon the child, they removed her at once from the tenement and brought Mary and her adoptive mother before a judge to investigate the claims of abuse: “Her body was bruised, her face disfigured, and the woman, as if to make testimony sure against herself, had the day before, struck the child with a pair of shears, cutting a gash through the left eye-brow and down the cheek, fortunately escaping the eye.”1
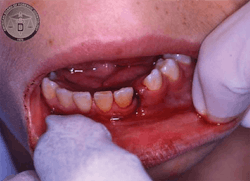
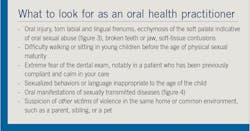
The child’s appearance was testimony enough, and on April 9, 1874, she was rescued. Abuse of this severity is inarguably deeply disturbing. It is conspicuous, unavoidable, and straightforward to document effectively. However, when pediatric physical abuse is hidden, intermittent, or sexual or emotional in nature, or a mixture of all, the dental team may not see any conspicuous evidence, and must be knowledgeable about the insidious markers that abusers leave behind. These signs are physical, too, but may also manifest as behavioral messages.
Going forward 150 years from Mary Ellen’s case, although laws protecting the abused child are advanced and support organizations are plenty, the attitudes regarding reporting or intervening haven’t changed significantly. The attitude of society, religion, culture, and law enforcement toward child endangerment and abuse is one of unanimous agreement in that it is abhorrent and intolerable. Yet when it comes to practice, the system fails many children.
Defining abuse
Child abuse and neglect (CAN) is not only defined medically and psychologically, but it also is defined legally. Legal definitions of CAN not only are broad but have a direct influence on case outcomes, as they affect prosecution and defense parameters and the decisions of lawyers and judges. Moreover, these legal definitions affect the policies and practices of child protection agencies, and the training and attitudes of practitioners.2
There are two legal systems set up to respond to and prevent CAN. First is the civil legal system, which focuses on the future of the child’s safety and best interests. It determines whether protection is needed, and the level of proof required is low (i.e., “balance of probability”). Second is the criminal legal system, which focuses on the past by judging the guilt of the accused. It is aimed at punishing the offender and for that, the standard of proof is set high (i.e., “beyond reasonable doubt”). An exception to this is the placement of a convicted child sex offender on a sex offender register, which is future focused and based on crimes the offender may commit in the future.3,4
The World Health Organization defines CAN as “all forms of physical and/or emotional ill-treatment, sexual abuse, neglect or negligent treatment, commercial or other exploitation, resulting in actual or potential harm to the child’s health, survival, development, or dignity in the context of a relationship of responsibility, trust, or power.”5 In international legislation, the term “child abuse and neglect” refers to behaviors and actions that result in actual and/or likely harm to any child or young person. These behaviors may be intentional or unintentional and include acts of omission (neglect) and commission (abuse).6
When a child alleges sexual abuse by a parent, the focus of the child protection court is solely on the child’s future safety. Although the criminal court may have judged the parent not guilty of the crime of child sexual abuse (due to lack of evidence), this does not mean that the civil child protection courts cannot make a ruling about the future safety of the child. Child protection proceedings focus on whether the child is in need of protection.3,4 They do not make a judgment about the guilt of an accused. This protection response is not, nor should it be, contingent on securing a conviction.4
Although young people under the age of 18 are legally children according to the United Nations Convention on the Rights of the Child, in this context, calling a young person a “child” can fail to acknowledge some important differences between children and young people, such as the difference in their desire and the age of consent that differs depending on legislation. This also applies to young people and older children as the perpetrators of abuse as well.
Child abuse and neglect can be subdivided into
- physical abuse,
- emotional abuse,
- neglect,
- sexual abuse, and
- exposure to domestic/family violence.
Although there is a broad consensus on this classification, defining each one in a way that is recognizable (or identifiable) can be difficult. For example, parenting practices that are acceptable in one culture may be considered abusive in another, although some are abusive regardless of culture. Therefore, it can be difficult to know whether the parental behaviors are harmful enough to constitute child abuse, as practitioners can have different perceptions about what constitutes “good enough” parenting.7
Most child protection legislation defines child abuse as a behavior or action that causes or is likely to cause a child significant harm, without defining the point at which a child is suffering significant harm or how to predict whether a child who is apparently suffering no harm or suffering minor harm is likely to suffer significant harm in the future. As such, the notions of culpability, motive, and intent are important when making decisions about whether to describe an incident as child abuse and neglect.8 Many parents who neglect their children do not intend to do so, but the abuse occurs as a consequence of poverty or disability.
Detection of CAN may be due to a child’s disclosure or through behavioral and physical indicators. The presence of a single indicator does not necessarily prove that a child has been abused, although in some instances single indicators clearly suggest the possibility of abuse. The repeated occurrence of one indicator or the presence of several indicators raises the possibility that the child has been, or is being, abused.
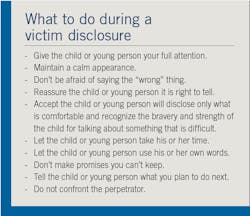
Victim disclosure
Abuse to children, adolescents, and teenagers happens at the hands of someone known to them, most prominently one or both parents or another close family member, 90% of the time. One in 20 children are the victims of abuse, be it physical, sexual, emotional, or a combination of two or more forms. Disabled children are three times more likely to become victims of sexual and physical abuse.9Physical indications of abuse
Children, such as newly walking toddlers or school-age children who play sports, are prone to accidents. However, accidental injuries almost all happen in protruded areas of the body (e.g., forehead, nose, elbows, knees, and shins)—in other words, the parts that stick out. Self-inflicted or nonabuse-related injuries rarely happen in protected areas of the body (e.g., ears, neck, inner arms, inner thighs, and genitalia). However, concern should be raised if the location, nature, or extent of the injury does not fit with the explanation given by the child or adult, or the child’s biological age or developmental age/stage is not consistent with the type of injury.
Some injuries are internal and need specific tests to identify them. Fractures, a life-threatening concern in a child under the age of two, are not often detected without radiography. Although the child may have a swollen joint and appear to be in pain or irritable, at this age they cannot verbally articulate to you that they are harmed. Similarly, brain or abdominal injuries (e.g., a bruised/ruptured liver or spleen) may be present without any visual signs. The presentation could be pain, vomiting, restlessness, or fever.
Behavioral indications of abuse observed in young children
Behavioral signs, or a sudden change in behavior, must be interpreted with regard to the victim’s age and developmental stage. This change is highlighted if the individual subjected to abuse is a regular patient. These signs may be presented in a combination or singularly:
- The child is unusually wary of physical contact with adults.
- The child seems to be unduly frightened of a parent or another adult.
- The child does not show emotion when hurt.
- The child offers unlikely, implausible explanations of injuries.
- The child wears inappropriate long-sleeved clothing on hot days (to hide bruising or other injuries).
- The child shows extreme polarity of normal behaviors to be overly compliant, shy, withdrawn, passive, and uncommunicative, or profoundly hyperactive, aggressive, disruptive, and destructive toward him-/herself and others.
- The child displays regressed behavior, such as bedwetting or soiling their clothes well after toilet training has occured.
- The child habitually misses scheduled dental/medical appointments and/or school. The parent/caregiver may be keeping the child at home until physical evidence of abuse has disappeared.
Behavioral indications in adolescents and teenagers
Other behavioral indicators, which may be more common in adolescents and young people than in children, include depression, criminal behavior (e.g., stealing, drug and alcohol use), and also civilly disobedient behaviors such as truancy, vandalism, and running away from home. Victims may behave as if they completely reject or lack trust in the world.12-14
Behavioral indications of abusers
Parents and caregivers guilty of abusing children will likely deny and/or attempt to conceal physical abuse. To do this, abusers may do any of the following:
- Accuse the child or adolescent of lying about the abuse.
- Provide an explanation for the injury, which is unbelievable, inadequate, or illogical. For example, the parent may say, “He bruises easily,” “Her brother hits her all the time and causes bruising,” or “He is so clumsy and prone to accidents.”
- Change their explanation for the injury over time.
- Appear unconcerned about the child’s condition.
- Delay seeking dental and medical assistance.
- Take the child to several different dentists, doctors, and hospitals.
- Break dental and medical appointments frequently.
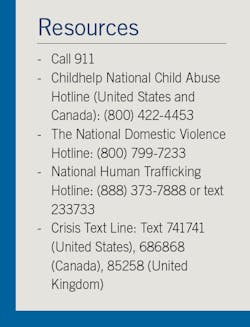
Reporting
It is important for individuals who work with children to be able to recognize child abuse and neglect. For example, if a health-care provider knows, or has reason to believe, a child is being hit or disciplined in a concerning way, the practitioner must first ask, is this, or might this be, child abuse? If a practitioner believes or suspects CAN, then a report must be made to child protection services or the police (see sidebar). In cases of child abuse reporting, health-care provider/patient privilege does not apply. If a child, parent, or caregiver confides to you or any of your staff that abuse has occurred, you must report it, and you are not required to keep that information confidential.
If the situation is an emergency, or you feel that the child or young person is in immediate danger, call 911 and report the situation to law enforcement right away. Demand that law enforcement officers (LEOs) arrive as soon as possible at your practice. Wait for LEOs to arrive before proceeding with procedures or confronting a parent or caretaker with direct questions or your suspicions. Be certain that the child and the adult are never left without supervision by a member of the dental team after law enforcement has been contacted. All conversations and all physical examination of the child should be performed with a member of the dental team as a witness. If the dentist is examining the child, an assistant or hygienist should be in the operatory at all times as a witness to all procedures performed and all conversations held between all parties. If a hygienist is examining the patient and suspects abuse, the hygienist should immediately request the assistance of any team member available to be present in the room during their examination at all times for the same reason. Front office personnel are also able to serve as witnesses.
In addition to your clinical diagnosis or differential diagnosis, some additional documentation is recommended here. Take photos (intra- and extraoral) using a ruler or scale next to injuries to show size. Even a cotton roll or periodontal probe can be used, because it is a size that is reproducible and consistent. Coins have been used in some cases for a size reference because that was all that was on hand, and it works! Include quoted remarks, comments, explanations made by the child and by the parent/guardian/caretaker, and take very descriptive notes on hard-and-soft tissue findings and any comments on the observable demeanor of the child and adult. Remember that this might be the only chance to document an injury before it heals.
Some witnesses to abuse are afraid of reporting it in case they are wrong in their suspicion or that the abusers may know who reported. Your identity as the reporter is confidential within the offices involved. However, if a case should go to court, your identity would be made known to the court through your written report and documentation, and your appearance may be required to provide testimony.
A mandated reporter is immune from civil or criminal liability when filing a report, whether or not it turns out that abuse has occurred. However, this does not mean that the reporter cannot be sued; another individual can sue anyone. So, the possibility does exist that a disgruntled parent or guardian might sue a mandated reporter. Even though the reporter will probably not be found guilty of any wrongdoing if the report was made in good faith, the reporter may nonetheless have to defend himself or herself in court and pay for legal counsel. If a mandated reporter is sued, the reporter can petition the state for compensatory legal fees.
Knowing this, consider the penalties for not reporting: any mandated reporter who willfully fails to report, or any person who impedes or inhibits a report of abuse or neglect of a person under the age of 18, and abuse or neglect is discovered to have occurred, can be liable for civil or criminal prosecution that can result in fines and/or a jail term. Furthermore, if the abuse or neglect results in death or great bodily injury, the negligent mandatory reporter can be liable for criminal prosecution, which can result in significantly higher fines and/or a jail term of up to one year or more.
In many states, an employee who is a mandatory reporter must sign a statement acknowledging understanding of this. For the states that do not require it, it is still a recommended action by employers that any person in their employ who meets the definition and provider category of a mandatory reporter sign a statement, provided and retained by the employer, to the effect that he or she has knowledge of the reporting law and will comply with its provisions. Dental office owners and administrators are strongly encouraged to provide training to their employees who are mandated reporters as to the office protocols and action plans for scenarios when abuse is suspected. An example statement for employees may be obtained at thecapcenter.org by searching “employee notification.”
Conclusion
CAN may affect the future lives of children and adolescents.15 Although this article highlighted some forms of abuse, there are many more types that require series of articles to tackle them. While some children are at greater risk than others, all children are potentially vulnerable to child maltreatment simply because they are dependent on adults for food, shelter, nurture, care, and protection. Moreover, exposure to different types of abuse varies for children depending on age, gender, and other social factors.
Oral health practitioners who have contact with children should ideally have a set of protocols in place to respond quickly and effectively to disclosures and reporting of abuse. If there are no protocols in place, you or your management should contact the relevant child protection department in your state or jurisdiction to set it up. Most importantly, the needs and welfare of the child or young person must take priority over any perceived threat to the reputation of the practice or associated individuals.
If a child or young person discloses abuse that is occurring, or has occurred, you should support the child or young person by believing them and reassuring them that telling was the right thing to do. If your organization does not have protocols in place for such circumstances, you should still report it to your management and the relevant statutory child protection department. Finally, keep information confidential. Only those people who must know should be informed of the disclosure.
It is important to remember that while it is your role to be a supportive listener, it is not your role to counsel the child or investigate his or her claims. Child protection workers will undertake investigations, and professional counselors should provide counseling.
Your response to a disclosure of abuse can be central to the individual’s ongoing safety and recovery. If no one takes action when there are suspicions that a child is being abused, it may place the child at serious risk of ongoing abuse and prevent the child’s family from receiving the help they need.
Further information on identification, screening, and assessment can be found on the Child Welfare Information Gateway website (childwelfare.gov).
References
1. Senn DR, Weems RA, eds. Manual of Forensic Odontology. 5th ed. Boca Raton, Florida: CRC Press; 2013:35.
2. Tomison AM, Tucci J. Australian Institute of Family Studies. Emotional abuse: The hidden form of maltreatment. NCPC Issues No. 8. https://aifs.gov.au/cfca/publications/emotional-abuse-hidden-form-maltreatment. Published September 1997.
3. Plum HJ. Legal responses to child maltreatment. In: Conte JR, ed. Child Abuse and Neglect Worldwide. Vol 1. Santa Barbara, California: Praeger; 2014:181-204.
4. Australian Law Reform Commission. Family violence—a national legal response. ALRC Report 114. NSWLRC Report 128. https://www.alrc.gov.au/wp-content/uploads/2019/08/ALRC114_WholeReport.pdf. Published October 2010.
5. Butchart A, Harvey AP, Mian M, Fürniss T. World Health Organization, International Society for Prevention of Child Abuse and Neglect. Preventing child maltreatment: a guide to taking action and generating evidence. https://apps.who.int/iris/bitstream/handle/10665/43499/9241594365_eng.pdf. Published 2006. Accessed June 9, 2019.
6. Bromfield LM. Chronic child maltreatment in an Australian statutory child protection sample [dissertation]. Geelong, Australia: Deakin University; 2005.
7. Turney D, Platt D, Selwyn J, Farmer E. Improving Child and Family Assessments: Turning Research into Practice. London, United Kingdom: Jessica Kingsley Publishers: 2012.
8. Platt D, Turney D. Making threshold decisions in child protection: A conceptual analysis. Brit J Soc Work. 44(6):1472-1490.
9. Wired UK. Sue Black catches paedophiles by looking at the marks on their hands. YouTube. https://www.youtube.com/watch?v=Qjqa8oTikP8. Published February 20, 2018. Accessed June 9, 2019.
10. Australian Institute of Family Studies. Australian legal definitions: When is a child in need of protection? CFCA Resource Sheet. https://aifs.gov.au/cfca/sites/default/files/publication-documents/1912_australian_legal_definitions.pdf. Published December 2019.
11. Benson R. To catch a paedophile, you only need to look at their hands. Wired UK website. https://www.wired.co.uk/article/sue-black-forensics-hand-markings-paedophiles-rapists. Published September 20, 2017.
12. McKelvie G. ‘I finally snared my paedophile granddad’: Woman went to cops after seeing sickening picture of pervert celebrating his 100th birthday. Mirror website. https://www.mirror.co.uk/news/uk-news/brave-woman-brings-paedophile-granddad-11628047. Published December 2, 2017. Updated December 6, 2017.
13. Stuewig J, McCloskey LA. The relation of child maltreatment to shame and guilt among adolescents: psychological routes to depression and delinquency. Child Maltreat. 2005;10(4):324-336. doi:10.1177/1077559505279308.
14. Johnson JG, Smailes EM, Cohen P, Brown J, Bernstein DP. Associations between four types of childhood neglect and personality disorder symptoms during adolescence and early adulthood: findings of a community-based longitudinal study. J Pers Disord. 2000;14(2):171-187. doi:10.1521/pedi.2000.14.2.17.
15. Annerbäck EM, Sahlqvist L, Svedin CG, Wingren G, Gustafsson PA. Child physical abuse and concurrence of other types of child abuse in Sweden-Associations with health and risk behaviors. Child Abuse Negl. 2012;36(7-8):585-595. doi:10.1016/j.chiabu.2012.05.006.
Amber D. Riley, MS, RDH, is a forensic dental consultant and dental autopsy technician for the San Diego County Office of the Medical Examiner and a practicing hygienist. She is a fellow of the American Academy of Forensic Sciences, member of the California Dental Hygienists’ Association, American Society of Forensic Odontology, and an associate member of the American Academy for Oral Systemic Health. She lectures internationally, covering evidence-based oral-systemic topics for dental professionals, forensic odontology, and oral pathology.
Sakher AlQahtani, BDS, MClinDent, PhD, is an assistant professor, pediatric dentist, and consultant at the College of Dentistry at King Saud University in Riyadh, Saudi Arabia. He is also an honorary professor at the University of Queensland, Australia. He is the founder and head of the Clinical Forensic Odontology Unit in Saudi Arabia, vice president of the Arab Association of Forensic Odontologists, and a member of the Medicolegal Health Council of Saudi Arabia.
About the Author

Amber D. Riley, MS, RDH
AMBER D. RILEY, MS, RDH, is a forensic dental consultant and dental autopsy technician for the San Diego County Office of the Medical Examiner and a practicing hygienist. She is a fellow of the American Academy of Forensic Sciences, member of the California Dental Hygienists’ Association, American Society of Forensic Odontology, and an associate member of the American Academy for Oral Systemic Health. She lectures internationally, covering evidence-based oral-systemic topics for dental professionals, forensic odontology, and oral pathology.

Sakher AlQahtani, BDS, MClinDent, PhD
SAKHER ALQAHTANI, BDS, MClinDent, PhD, is an assistant professor, pediatric dentist, and consultant at the College of Dentistry at King Saud University in Riyadh, Saudi Arabia. He is also an honorary professor at the University of Queensland, Australia. He is the founder and head of the Clinical Forensic Odontology Unit in Saudi Arabia, vice president of the Arab Association of Forensic Odontologists, and a member of the Medicolegal Health Council of Saudi Arabia.