Saliva is the “liquid gold” of the mouth. It serves as the mouth’s natural cleansing agent, carrying calcium and phosphate to aid in the remineralization process of the enamel and dentin.1 Saliva serves as a buffer to protect the oral, pharyngeal, and esophageal mucosa from orally ingested acid or acid regurgitation from the stomach.1,2 It also plays an essential role in taste sensations as well as digestion through the production of amylase. Saliva has a protective role, as it contains many antibacterial, antiviral, and antifungal agents that help provide a balanced microbial flora.1 Yet, studies indicate that up to 55% of the population experiences symptoms of xerostomia, or dry mouth.1
Review of xerostomia
There are many contributors to dry mouth, which include but are not limited to the use of certain medications, inhalers, vaping,
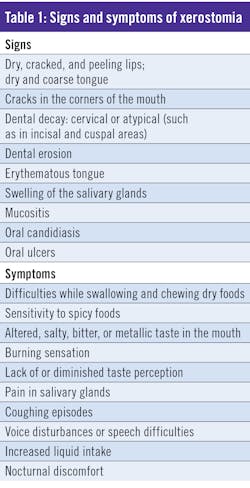
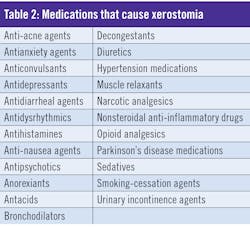
Table 1 lists the many signs and symptoms of xerostomia that clinicians should be aware of when assessing patients. Table 2 lists medications that may cause dry mouth.
Review of salivary glands
The three major salivary glands are the parotid, submandibular, and sublingual. These provide 90% of the total saliva volume.2 The parotid gland secretes mostly serous saliva, whereas the submandibular and sublingual glands secrete both mucous and serous saliva. Saliva is formed by acinar cells and modified by ductal cells to create a hypotonic solution.2 These glands provide unstimulated salivary flow to provide moisture throughout the mouth, which aids in normal functions such as speaking, swallowing, and remineralizing teeth.Other minor salivary glands contribute the remaining 10% of total saliva. Every two hours, the salivary glands are stimulated to complete alimentary functions, such as food digestion.2
Unstimulated and stimulated salivary flow
Saliva can be measured clinically by an unstimulated or stimulated flow. When determining the unstimulated salivary flow, the Challacombe technique (reviewed later in this article) is recommended.
The stimulation of saliva is dependent on the duration of the stimulus and the intensity. For example, a highly acidic stimulus (such as lemon-flavored candy) will result in a high saliva output.
Baseline production
The normal daily production of saliva is between 0.5 and 1.5 liters.2 A measurement of unstimulated salivary flow is a more accurate representation of baseline saliva production.
Total salivary flow is typically measured using a spit technique. Because salivary flow changes throughout the day, the purpose of the salivary measurement is to replicate the production of the individual patient.
A technique is advised by Mahvash Navazesh, DMD, to measure baseline production (figure 1).2 An unstimulated whole salivary flow rate of <0.1 ml/min or a stimulated flow rate of <0.7 ml/min is considered below normal.2
Clinical assessment of salivary gland hypofunction
Salivary gland hypofunction can be measured clinically. One method of measurement is to collect stimulated saliva.2 The protocol involves the patient spitting into various collecting devices. The following steps should be followed:
- Instruct the patient to lean his or her head forward over a collecting cup.
- Instruct the patient to swallow, which voids the mouth of saliva. This is the starting time.
- Instruct the patient to begin chewing a piece of gum according to the pace of a metronome set at approximately 70 beats per minute.
- At the end of the first minute, ask the patient to spit his or her saliva into the cup. The patient should refrain from swallowing. Tell the patient after the first minute to “Spit out, keep chewing,” and repeat this command after every minute.
- Discard the first two minutes’ samples. Proceed with three or more minutes of collection using a tube and funnel.
- After the final minute, ask the patient to spit everything (saliva and gum) into the tube.
- Weigh the sample. Subtract the weight of the gum, tube, and funnel, which should be preweighed before the start of the procedure.
This protocol also suggests implementing the same stimulated salivary test by having the patient suck on a piece of candy. Repeat steps one through seven. Substitute chewing gum with sucking on sugar-free, lemon-flavored candy. Remember, unstimulated whole saliva collection should always precede stimulated whole saliva collection.2
As previously mentioned, salivary gland hypofunction is considered as whole unstimulated saliva <0.1 ml/min (g/min), whole chewing stimulated saliva <0.7 ml/min, or both.2
The Challacombe chairside assessment
A clinical assessment that can be done chairside in less than five minutes is known as the Challacombe chairside assessment for
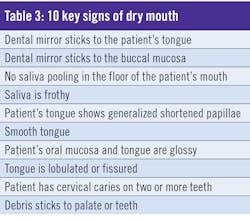
xerostomia. Stephen Challacombe, a professor of oral medicine at King’s College London, created an easy-to-use tool to identify the severity of xerostomia in patients.3,4 The scale is based on a clinical oral dryness score (CODS) and lists the 10 key signs of dry mouth, which are accompanied by example images. The patient’s score indicates the level of dry mouth.3,4 For each of the factors listed in Table 3 that the patient has, a point is given. A total score of 1 to 3 is classified as mild xerostomia, 4 to 6 as moderate, and 7 to 10 as severe.3,4
This process is easy to implement into a dental hygiene appointment, as these details are naturally assessed during the intraoral exam.
The increased use of medications in the general population can disturb the natural rate of salivary flow and increase the progression of oral disease.
Relief of xerostomia
GUM Hydral Dry Mouth Relief products are an ideal addition to xerostomia patients’ daily oral care routines. Adults and children over the age of 12 can implement this product into their everyday oral hygiene regimen for relief.
The GUM Hydral rinse can be used up to five times daily. Thanks to its higher viscosity, it coats the oral tissues for additional lubrication and comfort.5
GUM Hydral Dry Mouth Relief Gel provides immediate and up to four-hour relief of xerostomia after application. The recommendation is to apply 1–2 cm to the gums and tongue as needed.5 (Of note, patients tend to experience the most severe symptoms of xerostomia at night, as they are not stimulating the saliva through mastication.)
An easy-to-use dry mouth relief spray is also an option in the product line.
The GUM Hydral formulation is the only product that combines hyaluronic acid (as sodium hyaluronate; a high-viscosity humectant that has exceptional lubricating properties), betaine (a humectant), taurine (an amino acid used to help maintain proper hydration and electrolyte balance), and polyvinylpyrrolidone (PVP; a lubricant that forms a protective film over the oral mucosa). The unique combination of these four ingredients provides deep moisturizing relief at the tissue level and soothes the oral mucosa.
The product does not contain drying and irritating agents, such as alcohol, sodium lauryl sulfate (SLS), or sulfates. The formulation is nonoily and does not contain milk or egg derivatives. It has a mild flavor that can help with compliance.
Summary
The occurence of xerostomia is likely higher than ever before. The increased use of medications in the general population is one important reason. Disturbances in the natural rate of salivary flow increase the progression of oral disease. Therefore, treating xerostomia at its earliest signs will help preserve patients’ pH balance, natural flora, and oral health.
References
1. Dawes C, Pedersen AM, Villa A, et al. The functions of human saliva: a review sponsored by the World Workshop on Oral Medicine VI. Arch Oral Biol. 2015;60(6):863-874. doi:10.1016/j.archoralbio.2015.03.004
2. Navazesh M, Kumar SKS; University of Southern California School of Dentistry. Measuring salivary flow: challenges and opportunities. J Am Dent Assoc. 2008;139 (suppl):35S-40S. https://jada.ada.org/article/S0002-8177(14)63880-0/pdf
3. Dry mouth scale launched. Br Dent J. 2011;211:351. doi.org/10.1038/sj.bdj.2011.884
4. Das P, Challacombe SJ. Dry mouth and clinical oral dryness scoring systems. Prim Dent J. 2016;5(1):77-79. https://www.researchgate.net/profile/Stephen_Challacombe/publication/322009020_Dry_Mouth_and_Clinical_Oral_Dryness_Scoring_Systems/links/5a9d185a0f7e9be3796869b0/Dry-Mouth-and-Clinical-Oral-Dryness-Scoring-Systems.pdf
5. Sunstar. GUM Hydral. https://us-professional.gumbrand.com/gum-hydral-for-xerostomia-relief
About the Author

Amber Auger, MPH, RDH
Amber is a dental hygiene clinician, international speaker, and hygiene director who specializes in nonsurgical periodontal therapy, heart-centered education, and efficiency. Through her signature program, Thrive in the OP and Thrive Chairside Summit, she equips hygienists with evidence-based systems to elevate patient outcomes, confidence, and production. Amber blends clinical expertise with practical strategies to help dental teams implement sustainable, science-driven protocols. She can be reached at amberauger.com.