Snoring. It affects the snorer, the bed partner, and most likely everyone else in the house—maybe even the neighbors! Adult males have the worst reputation, but females are not exempt from trumpeting in the night. Laugh and the world laughs with you; snore and you sleep alone!1
There are two kinds of snoring: open mouth and closed mouth. Snoring in the noninebriated person occurs for many reasons. For instance, if the tongue falls back into the airway in a back sleeper, snoring results. Back sleeping seems to be the epitome of sleep posture according to chiropractors, but the downside is that it lends itself to snoring.
What does the tongue do?
There seems to be an anatomical misconception in dentistry that a tongue-tie ties the tongue out of the airway. This is incorrect. The tongue is almost alwaysMore about snoring:
In 2013, Dr. Christian Guilleminault (a pioneer in sleep medicine) penned a paper posing the theory that obstructive sleep apnea (OSA) in nonobese children is a disorder of orofacial growth.2 There’s no arguing that dentistry is uniquely qualified to manage the development of the craniofacial respiratory complex (CFRC), so creating a face that doesn’t result in sleep apnea is our first job. The CFRC development hinges on the tongue’s mobility to rest on the palate. If it can’t reach the palate, the entire system starts to break down.
Restriction in the tongue can contribute to extra choking as the swallow is affected when the tongue cannot undulate properly to transition the bolus of food from the oral phase to the pharyngeal phase. This may create the cute, reassuring sounds of sleeping infants, but it is a potential risk for pediatric OSA.3,4
Can weaning stop snoring?
As a child grows and weans from breastfeeding (which also contributes to facial development), feeding on pureed food from a spoon deprives the muscles in the oropharynx adequate development to sustain an open airway. The sight of a baby’s throat constricting and their little eyes bugging as they expel a piece of food sends most mothers into a panic. But that’s actually a time for a celebration—the throat is working! The book Baby-led Weaning5 helps guide parents through the trials and tribulations of home growth of the CFRC.
In children, adolescents, and teens, the cost of snoring is immeasurable. Increases in ADHD, learning disabilities, and executive function developmental delays lead to court costs and lost time at work, not to mention suicidal ideation.6-9
Can vitamins fight snoring?
There are many ways to improve sleep or avoid sleep apnea. Dr. Stasha Gominak has become an accidental sleep pioneer. During a fruitful career in neurology treating patients with migraines, she discovered many were on C-PAP (continuous positive airway pressure) therapy. She chased the rabbit down the hole to find a complex thread of low vitamin D levels. When the vitamin levels were raised back to normal, a new symptom of high anxiety occurred, which was solved by repairing the balance of B-complex and the intestinal microbiome.10
What’s a dental hygienist or dentist going to do with patients who snore? Remembering that there’s a correlation between OSA and periodontal disease is something to keep in the forefront of your mind.11 A lab test for blood values of vitamin D could be a start, but there is something even simpler.
10,000 throats, er, airways
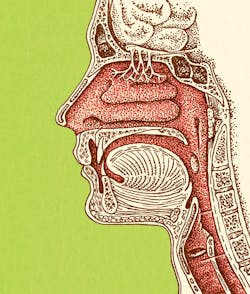
Many of us have seen 10,000 throats or more throughout our careers, yet we’ve never really appreciated the throat as “the airway.” Two clinical observations can lead dental providers to a differential diagnosis of obstructed airway: the Friedman score and the Mallampati score. Both require an open mouth, one with the tongue at normal rest in the mouth and the other with the tongue extended.
We hear about the Mallampati score most often—with the tongue out. It can be observed very simply during the oral cancer screening. Do you see the uvula? Do you see any black space around the uvula? No? That’s a Mallampati score of IV.12 In myofunctional therapy, we regularly tone and balance the muscles of the oropharynx, including the tongue, to open the airway.13 A referral to an orofacial myofunctional therapist (OMT) is good practice. There may be local or remote practicing OMTs, or as a stopgap, implementing a tool that can motivate those muscles during a normal human activity may be a solution to simple snoring.
The perfect swallow?
The perfect swallow starts with the tongue tip against the premaxilla. Precise coordination of the tongue, cheeks, soft palate, and the rest of the muscles lining the tunnel to the stomach are activated. Like a slow-motion whip, the blade of the tongue undulates to the middle third, which moves the fluid or bolus backward onto the posterior third and down into the esophagus, passing by the epiglottis covering the trachea, and on into the stomach.
There are more than 20 muscles involved in swallowing. The oral phase of swallowing is voluntary. Once the food or drink enters the pharyngeal phase, tactile receptors in the oropharynx shift the swallow to involuntary. The soft palate raises to close off the nasopharynx. Any of these muscle combinations can become weak over time from disuse or swallowing pureed foods like smoothies or veggies in pouches. Exercising these swallowing muscles can improve the muscle tone of the airway.
OMTs use many different tools, postures, and maneuvers, including balloons, corks, and toothbrushes, to activate the neuromuscular mechanics that keep the muscles from drooping. The REMastered Sleep bottle can fast-track muscle strength by forcing the muscles in the oropharynx to tone and hold the airway open. The bottle’s engineered silicone nozzle is designed to put the water onto the middle of the tongue, which can substantially improve the Mallampati score. The tip has a hole or slit that only opens under suction. The suction created by the lips around the nozzle and lowering the tongue draws the water up the straw and forces the hole to open. Lifting and exercising the soft palate can be part of the solution to a high Mallampati score.
Are you in an airway practice?
If the dental practice focuses on sleep or airway, the dentist is often interested in delivering a device that opens the airway by moving the lower jaw forward. These devices are often lab-fabricated and may take weeks to be delivered. During that wait time, the muscles of the snoring complex could be toning. Early anecdotal reports reveal patients find the REMastered Sleep nozzle easy to use all day, and their snoring reportedly decreases after about two weeks of habitual use (drinking two full bottles a day).
Mouth taping may also be a first defense against snoring. Made popular by author James Nestor in his book Breath: New Science of a Lost Art,14 mouth taping has gained a lot of popularity. It’s not for everyone, and to be done safely there are several things to consider. Check out the August 2021 issue of RDH magazine15 for a complete article on this topic. While useful for improving sleep quality by holding the mouth closed, mouth taping does little to build up the muscles of the oropharynx.
Snoring isn’t cute in babies, and it’s not normal in adults. It is an indication of upcoming problems that range in severity and impact on the quality of life. As we find reasons for snoring in the growth and development of the snoring complex, we must solve problems for our patients as soon as they are detected. Toning the muscles is the first step of the treatment plan from physicians and dentists. Orofacial myofunctional devices such as nozzles on a bottle can be part of the solution.
Editor's note: This article originally appeared in the March 2022 print edition of RDH.
References
- Burgess A. “Laugh and the world laughs with you, snore and you sleep alone.” Snore Quotes. Accessed September 26, 2021. https://quotes.yourdictionary.com/author/anthony-burgess/141027#snore
- Huang YS, Guilleminault C. Pediatric obstructive sleep apnea and the critical role of oral-facial growth: evidences. Front Neurol. 2013;3:184. doi:10.3389/fneur.2012.00184
- Guilleminault C, Huang YS. From oral facial dysfunction to dysmorphism and the onset of pediatric OSA. Sleep Med Rev. 2018;40:203-214. doi:10.1016/j.smrv.2017.06.008
- Collado MC, Katila MK, Vuorela NM, Saarenpää-Heikkilä O, Salminen S, Isolauri E. Dysbiosis in snoring children: an interlink to comorbidities? J Pediatr Gastroenterol Nutr. 2019;68(2):272-277. doi:10.1097/MPG.0000000000002161
- Rapley G, Murkett T. (2019) Baby-led Weaning: The Essential Guide to Introducing Solid Foods and Helping Your Baby to Grow Up a Happy and Confident Eater. The Experiment; 2010.
- Lee CH, Kim YJ, Lee SB, Yoo CK, Kim HM. Psychological screening for the children with habitual snoring. Int J Pediatr Otorhinolaryngol. 2014;78(12):2145-2150. doi:10.1016/j.ijporl.2014.09.026
- Bonuck K, Rao T, Xu L. Pediatric sleep disorders and special educational need at 8 years: a population-based cohort study. Pediatrics. 2012;130(4):634-642. doi:10.1542/peds.2012-0392
- Bonuck K, Freeman K, Chervin RD, Xu L. Sleep-disordered breathing in a population-based cohort: behavioral outcomes at 4 and 7 years. Pediatrics. 2012;129(4):e857-e865. doi:10.1542/peds.2011-1402
- Chattu VK, Manzar MD, Kumary S, Burman D, Spence DW, Pandi-Perumal SR. The global problem of insufficient sleep and its serious public health implications. Healthcare (Basel).2018;7(1):1. doi:10.3390/healthcare7010001
- Gominak SC. Vitamin D deficiency changes the intestinal microbiome reducing B vitamin production in the gut. The resulting lack of pantothenic acid adversely affects the immune system, producing a “pro-inflammatory” state associated with atherosclerosis and autoimmunity. Med Hypotheses. 2016;94:103-107. doi:10.1016/j.mehy.2016.07.007
- Latorre C, Escobar F, Velosa J, Rubiano D, Hidalgo-Martinez P, Otero L. Association between obstructive sleep apnea and comorbidities with periodontal disease in adults. J Indian Soc Periodontol. 2018;22(3):215-220. doi:10.4103/jisp.jisp_38_18
- Friedman M, Hamilton C, Samuelson CG, Lundgren ME, Pott T. Diagnostic value of the Friedman tongue position and Mallampati classification for obstructive sleep apnea: a meta-analysis. Otolaryngol Head Neck Surg. 2013;148(4):540-547. doi:10.1177/0194599812473413
- Carrasco-Llatas M, O’Connor-Reina C, Calvo-Henríquez C. The role of myofunctional therapy in treating sleep-disordered breathing: a state-of-the-art review. Int J Environ Res Public Health. 2021;18(14):7291. doi:10.3390/ijerph18147291
- Nestor J, Krupnik A. Breath: The New Science of a Lost Art. AB Publishing; 2021.
- Gutkowski SB. How mouth taping can be key to achieving healthy nasal breathing. RDH magazine. August 10, 2021. https://www.rdhmag.com/pathology/article/14206557/how-mouth-taping-can-be-key-to-achieving-healthy-nasal-breathing
About the Author
Shirley Gutkowski, BSDH, RDH
Shirley Gutkowski, BSDH, RDH, is the owner and primary practitioner at Primal Air LLC, located in Sun Prairie, Wisconsin. She and her team of RDH OMTs see most of their patients online. Primal Air is a three-part practice that not only serves the needs of patients but also gives OMT-trained RDHs a place to learn and practice the science of OMT. Gutkowski can be reached at [email protected].
Updated February 3, 2022