Tethered oral tissues: Signs, symptoms, and assessments
Kory Nieuwkoop, BS, RDHAP
New mothers are some of my favorite recall patients. As hygienists, we are great at informing first-time parents about the importance of their own oral health throughout pregnancy and the oral health of their little ones. As hygienists, we constantly remind parents of tips and tricks that help to keep the oral cavity healthy of their children, especially newborns and toddlers.
However, not many of us ask new parents how the baby is really doing. Are feedings going well, is the baby sleeping throughout the night or waking up every few hours, and lastly, does the baby seem happy and comfortable? We care how these new mothers and fathers are really doing because their health is affected, but also because these questions open the door for early detection of commonly misdiagnosed congenital oral anomalies.
Examples of an infant lip tie with slight lip callus formation, heart-shaped tongue tip due to tight ankyloglossia, and minimal vertical lift
Tethered oral tissues (TOTs) can include ties of the tongue, lip, and even buccal tissues. This is when the frenulums are short and/or thick and limit movement of tongue, lips, or cheeks.1 Between 4% and 10 % of newborns were diagnosed in 2005, but as awareness has increased, we have seen a growth in diagnoses as well. In 2014, diagnoses had grown to 20%; in 2017, the increase became so large that people called it (wrongfully) a fad.2 It is three times as common in males as females and studies show it can be hereditary also. As health-care professionals become more aware of oral anomalies assement, not only will diagnoses increase, but also options for early treatment.
Oftentimes, these anomalies produce symptoms that are misdiagnosed as acid reflux, colic, and even failure to thrive—all of which have treatments that will not help with the true condition itself. Babies who have one or more of these oral anomalies show symptoms of poor, difficult latch or popping off frequently when breastfeeding; gumming or chewing while nursing; gasping for air or clicking or wheezy sounds while nursing; and excessive drooling. This leads to excessive air swallowing during feedings, causing hiccups and gassiness, which can in turn cause colic and reflux issues.3
Infants can also become sleep deprived due to falling asleep during feedings only to wake up shortly after to nurse again. When the baby is not getting enough nutrients during feedings, he or she has poor weight gain, and in some cases this can become so extensive that the baby is diagnosed with failure to thrive—what new parent wants to hear that?
A tie in a toddler showing rounded tongue tip, anterior ankyloglossia with minimal vertical lift, and beginning effects on lower anteriors
This is not just uncomfortable for the child, though. Mothers of newborns with oral anomalies also suffer. They suffer from discomfort while nursing; blanched, cracked, blistered, or even bleeding nipples; plugged ducts, thrush, and mastitis due to the baby being unable to fully drain the breast. Most new mothers are already tired just from the adjustment of having a newborn, but can suffer from sleep deprivation since babies with TOTs need to be nursed more often and wake up every two to three hours to do so.3 This can lead to low milk supply, and eventually the mother may stop breastfeeding altogether while the infant is still very young.
Many mothers and their families manage to get through this stage without a proper diagnosis (for example, by bottle feeding), but that does not mean the symptoms just go away. As the baby ages, more problems associated with these oral anomalies present themselves. As the baby begins to develop teeth, the lack of movement can lead to increased caries risk due to being unable to clear the mouth of milk and food debris.
Gaps between teeth, TMJ dysfunction, and bruxism can be present. Difficulty eating and pronounced gag reflux are also more common. Once children become old enough to talk, walk, and do things for themselves, the symptoms become less bothersome unless there is a speech impediment, which is often treated with speech therapy, which again does not look at the root of the problem.
Today, there are many adults with oral anomalies. Signs and symptoms include being more likely to have mouth breathing, enlarged adenoids and tonsils, snoring, and sleep apnea issues. When feeding and breathing are affected, the brain will often overcompensate to protect these functions, leading to other body issues such as posture, chronic back and neck pain, and chronic stress due to poor sleep.3
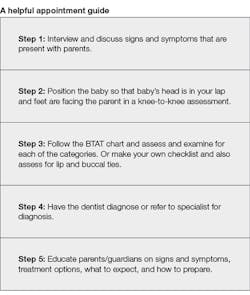
When I see these patients, I think to myself, “What can I do to help this mama out?” This comes down to early diagnosis, and as hygienists, we can be a part of the health-care team to provide correct assessments. Hygienists can correctly assess for tongue and lip ties and report findings to the dentist, who can diagnose and treat or refer the patient out for treatment.
This process begins at initial contact with expectant mothers. Educate and inform soon-to-be mothers on the signs and symptoms to watch for associated with oral anomalies. Then when you are seeing mothers with newborns, you can again inform and educate—but also investigate. Ask questions to determine if the baby may or may not have some of these signs and symptoms. Know that a mother will know best if something feels off, and she knows her own personal symptoms during breastfeeding as well.
Minimal tongue protrusion and lip callus formation
The best position to assess a baby is knee to knee, with the baby in your lap looking toward mom, much like if the baby was in your dental chair. Signs of an upper lip tie include a lip callous or the upper lip being connected to the maxillary gingiva without free movement. This is often the cause of poor or no latch.
Anterior and posterior ankyloglossia can be seen by amount of lift in the tongue, and if the frenum is attached at the gingiva ridge or the tip of tongue. Posterior ankyloglossia is a bit harder to diagnose, but is best detected with palpitation of the frenum. It is easiest to see the severity of ankyloglossia when the baby cries. Another way to detect ankyloglossia is by the way the latch feels to the mother and the sucking pattern. Posterior ankyloglossia often prevents a baby’s or toddler’s posterior tongue muscles from working properly, a common cause of choking and gagging. You will be able to feel the tongue muscles or lack of latch depending on where the tie is located. The Bristol Tongue Assessment Tool (BTAT) is a simple outline of what to look for when assessing for ankyloglossia.4
If TOTs are determined, the patient should then be sent for diagnosis and further consultation of treatment options. Treatment options are often based on severity of the ties, if symptoms are present, and if benefits outweigh the risk. Frenectomy via laser is the most common, and said to be the most effective.1 However, there will be several weeks of post-treatment therapy, which is done every four to six hours each day for best results.
References
1. Canadian Agency for Drugs and Technologies in Health. Frenectomy for the Correction of Ankyloglossia: A Review of Clinical Effectiveness and Guidelines. CADTH Rapid Response Reports. https://www.ncbi.nlm.nih.gov/books/NBK373454/. Published June 15, 2016. Accessed November 14, 2018.
2. Ghaheri B. Diagnosing tongue-tie in a baby is not a fad. Dr.Ghaheri.com. https://www.drghaheri.com/blog/2014/2/17/diagnosing-tongue-tie-in-a-baby-is-not-a-fad. Published February 18, 2014. Accessed November 14, 2018.
3. Hanson D. Effects of oral restrictions (tongue and lip ties). Dr. Dan Hanson website. http://www.drdanhanson.com/healthy-tips/effects-of-oral-restrictions-tongue-and-lip-ties. Published June 10, 2016. Accessed November 14, 2018.
4. Ingram J, Johnson D, Copeland M, Churchill C, Taylor H, Emond A. The development of a tongue assessment tool to assist with tongue-tie identification. Arch Dis Child Fetal Neonatal Ed. 2015;100(4):F344-8.
Kory Nieuwkoop, BS, RDHAP, studied public health at Westminster College and graduated from College of Southern Idaho’s dental hygiene program. She currently works clinically as a licensed dental hygienist with more than three years of experience, and she teaches pharmacology at a local dental hygiene school. She has a passion for prevention and whole-body health. Hobbies include triathlons, fitness, and being an aunt.