It’s time to get comfortable discussing HPV
The day started out like a normal Wednesday, work in the morning and then a trip to Trader Joe’s. I almost didn’t go; my to-do list was long, and the 36-mile round trip would take time away from checking things off that list, but the little voice inside my head was telling me to go.
There’s butter lettuce, and then there’s Trader Joe’s butter lettuce, so it’s always the first thing on my list. Moving through the aisles, I filled my basket with other favorites. With a full grocery cart, I headed to the shortest checkout line. Watching the two young men who were checking and bagging the customers ahead of me was a treat; they were engaging and obviously enjoying their day at work—you could sense the smiles under their masks. As the customers ahead of me left, the checkers turned to me with bright eyes peeking over their masks and said, “How are you today? Thank you for coming in!” After exchanging pleasantries, the checker asked what I do for work. I told him I’m a dental hygienist, and I speak and educate on oral cancer. With that, he stopped scanning my groceries and said, “That’s really specific; I’ve never heard of that. I’m glad neither of us smokes; we won’t ever get that cancer. Do you have any fun or interesting facts or information to share with us about oral cancer?”
From butter lettuce to oral sex
Now I knew why that little voice was telling me to go to Trader Joe’s that day. For reasons unknown to me, I was supposed to share information with these young men. It was the perfect scenario: two young, nonsmoking, white males who believe they are not at risk for oral cancer asking me to share information with them. They didn’t know my passion for this, and sure didn’t know what was about to be shared with them! I said, “I would love to share! Thank you for asking. What we now know is that the human papillomavirus (HPV) is the main cause of oropharyngeal cancer. It’s cancer in the back of the mouth, typically in the tonsils and back part of the tongue, and those most at risk are white, nonsmoking males. We also know that HPV now causes more of this cancer than it does cervical cancer.”1
More from this author:
- Skin cancer screening: A dental hygienist's life-saving responsibility
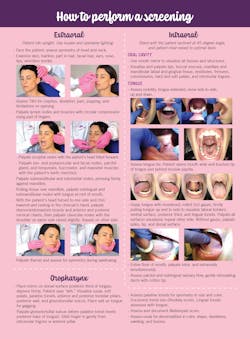
- The Cotten Method of Screening
- The state of oral and oropharyngeal cancer screening in our profession
By this time, the young man bagging my groceries had stopped bagging. Both young men were intent on knowing more and very surprised to learn about this cancer and to find out they could be at risk. They said they had heard about HPV and cervical cancer but not about it causing cancer in the mouth. Both continued to ask questions, wanting more information, including how HPV gets in the mouth, and specifically what they can do to help reduce their chance of getting this cancer. I shared with them that HPV is transmitted through skin-to-skin contact, orally through oral sex, and possibly through open mouth, deep, aggressive kissing. I recommended protection during oral sex just as with conventional sex. We also discussed the HPV vaccine, which they had both had; however, they didn’t know much about it and didn’t know it could aid in protecting them from persistent HPV infections, which could possibly result in cancer. It wasn’t an awkward conversation; they were truly curious and wanted more information, and I was thrilled to get to share this information with them. They both said that they go to the dentist regularly.
Many opportunities to educate
In the last 12 years of being immersed in raising awareness about HPV and oral and oropharyngeal cancer, I wish I’d kept track of the number of conversations like this that have occurred, inside and outside of the operatory. There are simply too many to recall. Another recent conversation took place while in line for Donny Osmond’s VIP preshow in Las Vegas, again with a nonsmoking male. He was in line holding a place for his wife while she was getting ready. He, too, had many questions and asked about transmission of HPV to the mouth. He stated he was aware of HPV causing cervical cancer, but not cancer in the mouth. He was most curious about what signs and symptoms to watch for and what to do if he noticed any of those. We discussed these, and I recommended he see an ear, nose, and throat specialist (ENT) for further investigation if he ever experiences any persistent signs and symptoms.
Also, while writing this article, a phone conversation with a business colleague in his 60s about my work in oral cancer prompted him to inquire further about HPV and how it gets in the mouth. He thought he knew but wanted a little more clarification. And just last week while listening to a radio program with a respected physician as the guest, the topic of HPV was brought up. The physician mentioned HPV and its association with cervical cancer and mentioned the HPV vaccine. However, the vaccine was only referenced in relation to preventing cervical cancers, not head and neck cancers or the other cancers associated with persistent HPV infections. It was a missed opportunity for a large listening audience to learn more about other HPV cancers.
It’s purely my opinion, but I think people inquire further about oral cancer and HPV because they don’t hear much about it in the media, or even in their medical and dental offices. The messaging for cancers such as breast cancer, colon cancer, and cervical cancer is intentional in the media and respective medical offices, but not so much for oral cancer. Dentistry needs to be more intentional about educating and raising awareness about HPV and oral and oropharyngeal cancers.
What we now know is this: the number of HPV-associated head and neck cancers has surpassed the number of HPV-associated cervical cancers. Unfortunately, the messaging about HPV is still focused on cervical cancer.2
Lessons learned
I’ve learned a few things during my years of work in raising awareness about HPV and oral cancer through conversations with patients and the public.
First, if the public is going to be educated and aware of HPV and its association with head and neck/oropharyngeal cancer, it will come from dental professionals. In fact, it is our ethical responsibility to share this information about “our cancer.” If they don’t hear it from us, where else? It’s okay, even essential, to talk about the transmission of HPV via oral sex, its association with head and neck cancers, and the availability of the HPV vaccine that can aid in reducing persistent HPV infections associated not only with oropharyngeal and cervical cancer but also anal, penile, vaginal, and vulvar cancers.
Society is open to hearing this information. The public wants to know how to help prevent cancers and recognize the signs and symptoms for the earliest detection. Most are still of the belief that tobacco is the only risk factor for oral and head and neck cancers. Patients and the public deserve to know this information so they can make informed decisions for themselves about their oral health. This does not need to be a knee-to-knee conversation; the optimal time to share information is during the extraoral and intraoral evaluation (EOIO). Information can also be shared in newsletters the dental office sends to patients, in social media posts, and in brochures and flyers in the office.
The public and some medical and dental professionals are misinformed about HPV. It is still the common belief that HPV is most associated with causing cervical cancer and the purpose of the HPV vaccine is to help prevent cervical cancers in females. Statistics released by the US Cancer Statistics Data Briefs, No. 26 in December 2021 based on data from 2014–2018 reveals that there are approximately 10,600 cases of oropharyngeal cancer in males and 1,800 cases of oropharyngeal cancer in females each year that are attributable to HPV types 16 and 18.2 The US FDA added prevention of oropharyngeal cancer to the HPV vaccine’s indication: “The human papillomavirus (HPV) recombinant 9-valent vaccine (Gardasil 9) received FDA approval for an expanded indication to include the prevention of oropharyngeal and other head and neck cancers caused by HPV types 16, 18, 31, 33, 45, 52, and 58.”3
People are listening! The public and our patients are listening, and they are looking for health-care professionals to share our expertise and have courageous conversations about critical health information. When I first started sharing information about HPV with my patients 12 years ago, I would bring it up when I was palpating the occipital nodes behind them so I wouldn’t have to look at them. I was very uncomfortable with this conversation at first; however, I knew it was vital information to my patients’ oral and systemic health and it needed to be shared. During your clinical appointments, find the time and place that is most comfortable for you.
Our job doesn’t end when we take off our scrubs. Be open to spontaneous conversations regarding essential information about HPV and oral cancer. In a recent conversation with Katrina Sanders, MEd, she eloquently said, “Irene Newman, the first dental hygienist—her job was not to improve production and close more cases. Her job was to be a patient advocate and educate the community.” I’m encouraging you to be like Irene Newman: be an advocate and educate the community, share the tremendous amount of knowledge, expertise, and lifesaving information you possess about “our cancer,” not only with patients, but the general public as well.
Call to action
If you are uncomfortable or lack confidence in sharing information about HPV or feel you need more knowledge, find a mentor, do some research, and be your own advocate to gain the knowledge you need. Recruit your entire dental team or dental service organization (DSO) to establish a positive, informative culture around HPV and oral cancer. Make it your mission to save lives through sharing critical information with patients and the public. Perform a thorough EOIO evaluation on every patient, tell them what you’re doing, and use that time to efficiently share information and raise awareness about what we now know concerning HPV and oral cancer.
Get yourself started with a practitioner HPV fact sheet and patient HPV fact sheet.
Editor's note: This article appeared in the March 2022 print edition of RDH magazine. Dental hygienists in North America are eligible for a complimentary print subscription. Sign up here.
References
- HPV/oral cancer facts. The Oral Cancer Foundation. https://oralcancerfoundation.org/ understanding/hpv/hpv-oral-cancer-facts/
- Cancers associated with human papillomavirus, United States—2014–2018. U.S. Cancer Statistics Data Briefs, No. 26. Centers for Disease Control and Prevention. December 2021. https://www.cdc.gov/cancer/uscs/about/data-briefs/no26-hpv-assoccancers- UnitedStates-2014-2018.htm
- FDA adds prevention of oropharyngeal cancer to HPV vaccine’s indication. AAP News. May 2021. https://www.fda.gov/media/150779/download
About the Author

Susan Cotten, BSDH, RDH, OMT
Susan Cotten, BSDH, RDH, OMT, is dentistry’s oral cancer coach, 2018 Sunstar/RDH Award of Distinction recipient, and developed The Cotten Method™ of Screening for oral, oropharyngeal cancer, and other head and neck concerns. With more than 30 years as an RDH, Susan provides in-office training, speaking, and hands-on workshops to deepen confidence in a comprehensive screening, reduce liability, and increase early detection. Determined to have a world Oral Cancer Free™, her course is available online through the National Network of Healthcare Hygienists. Reach her at [email protected].