So many dental products: Which ones to recommend?
There are numerous posts on countless social media forums asking about relief and preventive recommendations for people undergoing cancer treatment. There are also numerous inquiries for products for people who have moderate to severe xerostomia due to polypharmacy, Sjögren’s, lichen planus, and other ailments. While several of the recommended products are great, many answers online do not address the root of the problem.
While these conditions have similarities, they’re all quite different. The treatments are also different, and what works for one patient may not work for another. What exactly is the goal when making product recommendations?1 Likely, it is preventing decay.
Read more articles like this one
Tipping the balance toward remineralization
Hydroxyapatite: A way to brush your teeth with their natural components?
To get to the root of the problem, here’s what we need to ask patients.
- What is the cause of the decay?
- Do you see signs of xerostomia?
- Have you tested for acceptable salivary output?
- Is there demineralization? (Why? Is it poor oral health (OH) habits or other dietary habits, such as sucking on candies or consuming acidic beverages?)
- Have you tested the oral pH?
Many of these conditions are symbiotic, meaning they’re dependent on each other. The first step is to determine the goal of the outcome.
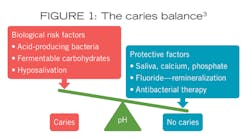
Remineralization consists of redepositing the lost calcium and phosphate ions that leeched out of the enamel about 20 minutes after exposure. This process needs a neutral environment in which to occur. CAMBRA2 recommendations state that by adjusting the protective factors—increasing the saliva, increasing the available calcium and phosphate ions, using fluoride and remineralization therapy with possible antibacterial therapy—the scale can be tipped to a no caries zone (Figure 1).
Remineralization works wonders
A great alternative is to incorporate a remineralization paste or cream into the home-care routine. If a lesion has not cavitated into the dentin, it’s possible to remineralize the enamel and prevent further breakdown of the tooth structure. The enamel can then become stronger and free from erosion.
Adding remineralization pastes or creams to the oral care routine supports the remineralization process and strengthens the teeth. These products also neutralize the acids in the oral environment and smooth roughened tooth surfaces that can trap bacteria and acids in the enamel defects. Open dentin and enamel tubules often lead to sensitivity. Remineralization pastes and creams coat and close off the tubules, effectively desensitizing the tooth. The pastes use hydroxyapatite to redeposit the leeched calcium and phosphate ions into the tooth surface.4
Delivery of these remineralization products is easy. It can be done at home with a toothbrush, a cotton tip applicator, or one’s finger. Another method preferred by many is customized trays. Many people already possess whitening trays that can be used for this purpose. All oncology patients should be using customized trays as part of their treatment plan.
Tray use is convenient as they can be worn while performing other tasks. Placing the paste or creams in trays provides a longer contact time with the teeth if worn overnight or a few hours. To optimize the success of a remineralization paste or cream, it is recommended the person not eat or drink for 30 minutes after application. Using trays overnight makes this procedure more attainable.
Remin Pro by Voco is one of the leading remineralization creams that contains nanohydroxyapatite, fluoride, and xylitol. It contains more fluoride (1,450 ppm) than other brands.5 The nanohydroxyapatite restores the mineral balance and xylitol has cariostatic properties. Remin Pro contains no milk proteins, which is contraindicated for those who have a true allergy risk. Remin Pro comes in three flavors,6 with melon the flavor of choice when treating oncology patients.
Patients suffering with xerostomia, enamel demineralization, and the subsequent high caries risk have diverse needs due to age, lifestyles, and comorbidities. Their needs can also change over time with an exacerbation of illness, stress, or even physical limitations. It becomes important for practitioners to have a variety of options available so that recommendations can be individualized.
Disclosure: Voco is a financial supporter of RDH magazine.
Editor's note: This article appeared in the March 2023 print edition of RDH magazine. Dental hygienists in North America are eligible for a complimentary print subscription. Sign up here.
References
- Potts K. The 5 questions you should ask first if you suspect your patient has dry mouth. October 25, 2016. DentistryIQ. https://www.dentistryiq.com/dental-hygiene/patient-education/article/16352713/the-5-questions-you-should-ask-first-if-you-suspect-your-patient-has-dry-mouth
- Hurlbutt M, Young DA. A best practices approach to caries management. J Evidence Based Dent Prac. 2014(14):77-86. 10.1016/j.jebdp.2014.03.006
- Young DA, Featherstone JD. Caries management by risk assessment. Comm Dent Oral Epidemiology. 2013;41(1):e53-e63.
- Arifa MK, Ephraim R, Rajamani T.Recent advances in dental hard tissue remineralization: a review of literature. Int J Clin Pediatr Dent. 2019;12(2):139-144. 5005/jp-journals-10005-1603
- Walsh LJ. Contemporary technologies for remineralisation therapies: a review. Int Dent. 2009;11(6):6-16.
- Nourolahian H, Iman P, Fatemeh M. The effect of Remin Pro on the microhardness of initial enamel lesions in primary teeth: An in vitro study. Dent Res J. 2021;18(1):16. 10.4103/1735-3327.311423
About the Author

Kris Potts, BS, RDH, FAADH
Kris Potts, BS, RDH, FAADH, has been a member of the ADHA, and a Fellow with the American Academy of Dental Hygiene and the American Academy for Oral Systemic Health. After achieving certifications in caries management, sleep care coordination, and oncology care, Kris acts as a key opinion leader in the dental industry. She is a published author and international speaker. Her company, Oral Health Promotion Strategies, provides resources, product information, education, and coaching services for health professionals, consumers, advocacy and support groups.