The buzz about Botox: What dental hygienists need to know
The popularity of cosmetic procedures has increased significantly over the last decade. According to the American Society of Plastic Surgeons, 13,281,235 minimally invasive cosmetic procedures—such as neuromodulator injections, soft tissue filler injections, and chemical peels—were performed by their members in 2020.1 Of note, plastic surgeons were not the only health-care professionals who performed these minimally invasive procedures. In 2018, the American Society for Dermatologic Surgery reported that 2.1 million injections of neuromodulators were administered by dermatologists.1 Additionally, physicians, physician assistants, registered nurses, and dentists all may perform minimally invasive procedures depending on their state laws.
The most popular of these cosmetic injections is botulinum toxin, or Botox as it is commonly referred. Botox is a pure neurotoxin produced by the anaerobic bacteria Clostridium botulinum. It paralyzes muscles by obstructing the nerve impulses that produce muscular contraction. Botox use has increased, and now is widely used in both cosmetic dentistry and for therapeutic purposes. In recent years, an increasing number of patients have benefited from the Botox treatments they receive at their dentist’s office.2
You may also be interested in ... Dental hygienists and Botox: It's complicated
The word botulism can invoke images of severe illness and even death; however, when used locally and for specific disorders, Botox is incredibly safe. Most side effects are transient and minor. The most frequently reported adverse effects are transitory muscle spasms, anxiety in new patients, and headaches that may be related to the injection technique for a variety of reasons, including periosteal damage or intramuscular hematomas.3
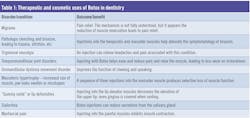
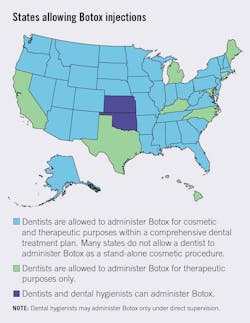
The FDA first approved Botox in 1989 to treat hemifacial spasm; in 2000, it was approved to treat cervical dystonia.1 Since then the therapeutic and cosmetic uses for botulinum toxin have increased. There are several dental-related conditions that botulinum toxin treats with much success, though the mechanism of action is not always thoroughly understood (table 1).3-6 Currently, only certain health-care providers who receive appropriate and approved training may administer Botox. Within dentistry, it varies from state to state whether a dentist can administer Botox cosmetically or therapeutically.
Adverse effects of Botox
Adverse effects associated with Botox are typically mild, but side effects after the injection—such as erythema, edema, pain, ptosis (drooping) of eyelid or brow, ecchymosis (bruising), and muscle weakness—can occur. Most adverse effects are identified as mild and temporary.7 Allergic and hypersensitivity reactions have been reported due to usage of Chinese botulinum toxin stereotype A.8 Hypersensitivity or pseudoallergic reactions must be reported.
Other mild adverse reactions include development of a short-term headache. This could be due to the initial muscle spasms that occur followed by complete paralysis or perhaps due to a deep muscle hematoma.7,8 In rare cases, there have been reports of flulike symptoms and nausea. Muscle atrophy is a possible side effect with long-term use of Botox. Contraindications are limited and include any hypersensitivity to botulinum toxin and infection in or around the injection area.2,3
Training required to administer Botox
States vary significantly in their allowance of Botox administration. Interest is growing, however, and many states have made a provision for it in the state’s practice act for dentists (less so for dental hygienists). For example, in Oregon, a dentist can administer botulinum toxin type A and dermal filler to treat a condition that falls within the scope of practice of a licensed dentist. The educational requirements for many of the states that allow Botox administration include successfully completing a minimum of 20 hours in a hands-on course that includes administration of Botox and dermal fillers. The provider may also need to be approved by the Academy of General Dentistry Program Approval for Continuing Education (AGD PACE) or the American Dental Association Continuing Education Recognition Program (ADA CERP).9 The American Dental Association recognizes the American Academy of Facial Esthetics (AAFE) as the premier choice for training/continuing education in Botox and dermal fillers. The ADA, partnering with the AAFE, holds a live-patient, two-day course in Chicago. The ADA includes a disclaimer that not all states permit dentists to administer botulinum toxin, and dentists should consult their state dental board before performing any related procedures. Some dental schools will bring in an outside expert, such as Esthetic Skin Institute or AAFE, to host a two-day hands-on training course.
Botox laws by state
Research into this topic reveals the incredible variability and lack of clarity around whether dentists are permitted to administer Botox. Most state practice acts do not specifically have language regarding its administration. In most states, dentists choose to administer Botox based on the state’s laws and rules not specifying the topic one way or the other. In other words, the law does not say a dentist cannot administer Botox. At the same time, there may be no specific provision for administering Botox within the state laws and rules. In this gray area, dentists may choose to seek further training either by becoming certified through the AAFE or other hands-on CE courses.
Some states do provide guidance and may specify that only oral surgeons can administer Botox, or that general dentists may administer Botox but only for dental-related issues such as TMJ. Still other states specify Botox is allowed as long as the dentist is practicing “within the scope of dentistry” and Botox is part of a comprehensive dental treatment.10 A simple Google search reveals most states contain dental practices that advertise both cosmetic and therapeutic Botox procedures.
Our research included reaching out to state dental boards to clarify this topic. One state board of dentistry stated: “The board does not have an official position on Botox/dermal fillers. Licensees are required to review their practice act and use their professional judgment to determine whether or not they are permitted. It is likely highly dependent upon the factors of what the [injection] is being used for; that is to say, is it being used to treat a patient within a treatment plan?” (personal correspondence).
Botox and dental hygienists
Though the number of dentists who administer Botox has increased significantly over the last decade, dental hygienists have not made much progress on this front. Several states have proposed legislation or tried to initiate a rule change by the dental board, with little success. A common argument made in favor of dental hygienists administering Botox involves the similarity in education between a registered nurse and a registered dental hygienist. Notably, many states allow nurses to administer Botox; however, unlike nurses, dental hygienists must have detailed knowledge of head and neck anatomy upon graduation. In most states, dental hygienists are very comfortable performing intraoral injections, which is a skill most nurses do not have.
There have been significant advocacy movements at the state level. Nevada was the first state to allow dental hygienists to administer Botox under the direct supervision of a dentist. However, Lancette VanGuilder, BS, RDH, stated in an interview in 2016, “a social media post ruined the movements as it was published before the Nevada Dental Hygienists’ Association prepared an official public comment.” We contacted VanGuilder who is a Nevada hygienist and past ADHA District XII Trustee and asked her about the updates regarding Botox advocacy. She responded: “As far as progress, there has been none. In the Nevada legislature, they have continued to restrict providers who can administer, and there is not a culture to authorize any new providers; we have been unable to secure a bill sponsor for the last six years (three sessions) to even present it for a law change” (personal correspondence). She said the administration of Botox remains on Nevada’s legislative agenda.
In Oregon, Lisa Rowley, MS, RDH, past advocacy director for the Oregon Dental Hygienists’ Association, stated that there has been great interest in Botox administration among dental hygienists in Oregon, but the Oregon Board of Dentistry has not regulated any changes on this topic.9 According to ODHA, RDHs and Botox are in the top five for advocacy movements in Oregon in 2023 (personal correspondence).
Our research revealed only two states that currently allow dental hygienists to administer Botox under the direct supervision of a dentist. The Kansas Dental Board approved dental hygienists to administer Botox under the direct supervision of a dentist in August 2022.11 In 2023, Oklahoma began allowing dental hygienists to administer Botox. To our knowledge these are the only two states that have made provisions for dental hygienists.
Editor's note: An earlier version of this article incorrectly stated that dental hygienists in Massachusetts are allowed to administer Botox. The article has been updated to remove this error, and to add Oklahoma to the list of states that allows RDHs to administer Botox.
This article appeared in the August 2023 print edition of RDH magazine. Dental hygienists in North America are eligible for a complimentary print subscription. Sign up here.
References
- Pearlman RL, Wilkerson AH, Cobb EK, et al. Factors associated with likelihood to undergo cosmetic surgical procedures among young adults in the United States: a narrative review. Clin Cosmet Investig Dermatol. 2022;15:859-877. doi:10.2147/CCID.S358573
- Azam A, Manchanda S, Thotapalli S, Kotha SB. Botox therapy in dentistry: a review. J Int Oral Health. 2015;7(Suppl 2):103-105.
- Serrera-Figallo MA, Ruiz-de-León-Hernández G, Torres-Lagares D, et al. Use of botulinum toxin in orofacial clinical practice. Toxins (Basel). 2020;12(2):112. doi:10.3390/toxins12020112
- Capehart KL, Mollica AG, Young N. Migraines and Botox: what dental assistants need to know about introducing migraine care in the practice. Dent Assist. 2018;87(5):10-12.
- Nayyar P, Kumar P, Nayyar PV, Singh A. BOTOX: broadening the horizon of dentistry. J Clin Diagn Res. 2014;8(12):ZE25-ZE29. doi:10.7860/JCDR/2014/11624.5341
- Witmanowski H, Blochowiak K. The whole truth about botulinum toxin – a review. Postepy Dermatol Alergol. 2020;37(6):853-861. doi:10.5114/ada.2019.82795
- Sethi N, Singh S, DeBoulle K, Rahman E. A review of complications due to the use of botulinum toxin A for cosmetic indications. Aesthetic Plast Surg. 2021;45(3):1210-1220. doi:10.1007/s00266-020-01983-w
- Careta MF, Delgado L, Patriota R. Report of allergic reaction after application of botulinum toxin. Aesthet Surg J. 2015;35(5):NP102-NP105. doi:1093/asj/sju105
- Scope of practice. Oregon Board of Dentistry. Accessed April 10, 2023. https://www.oregon.gov/dentistry/pages/scope-practice.aspx
- Choi YJ. Does the scope of dentistry include facial esthetic procedures such as botulinum toxin injection or laser treatment? J Am Dent Assoc. 2022;153(2):98-99. doi:10.1016/j.adaj.2021.10.008
- Dental and dental hygiene application by credential. Meeting minutes. Kansas Dental Board. August 2022. https://www.dental.ks.gov/docs/default-source/default-document-library/application-by-credential-(2021)c64a3d600997623f8994ff0000a74f6d.pdf
About the Author

Tala Alkhatib, BSDH(c)
Tala Alkhatib, BSDH(c), will graduate in 2023 from the School of Dental Hygiene at Pacific University in Hillsboro, Oregon.
Updated July 6, 2023

Saheleh Ansarizadeh, BSDH
Saheleh Ansarizadeh, BSDH(c), will graduate in 2023 from the School of Dental Hygiene at Pacific University in Hillsboro, Oregon.
Updated August 3, 2023

Michelle Mendoza Nicolas, BSDH
Michelle Mendoza Nicolas, BSDH(c), will graduate in 2023 from the School of Dental Hygiene at Pacific University in Hillsboro, Oregon.
Updated August 3, 2023
Lesley Harbison, MS, RDH, EPDH
Lesley Harbison, MS, RDH, EPDH, is an assistant professor in the School of Dental Hygiene at Pacific University in Hillsboro, Oregon. She has been practicing clinical dental hygiene for 20 years in various offices, including periodontal, general, and direct access care. In 2019 she earned a master’s degree in dental hygiene at Idaho State University. Her professional interests include increasing access to care, the geriatric population, ethics and empathy in dental hygiene, and advancing the dental hygiene profession.
Updated July 6, 2023