Coding for TMD
Evidence-based TMD diagnosis and treatment benefits from expanded insurance coverage
By Patti DiGangi, RDH, BS, and Christine Taxin
Significant changes to the way dentistry is being practiced have recently been set in motion by two influential factors — science and evidence-based decision-making. An estimated 10% to 15%, about 10 million Americans, are affected by temporomandibular muscle and joint disorders (TMD). Accurate evidence-based diagnosis is the best method to determine appropriate treatment. The question is whether dental or medical insurance will cover this important care. Determining and documenting dental-medical necessity is the basis for successful coding. All dental team members have a role in determining dental-medical necessity.
Dental-medical necessity defined
Medical-dental necessity isn't as complicated as it might appear. Our tools for successfully identifying the clues to the most accurate medical-dental necessity are:
- Providing the most appropriate service
- Diagnosis that is consistent with the symptoms
- Treatment that is consistent with the diagnosis
- Treatment that is not primarily for the convenience of the patient or provider
- Treatment that is good medical/dental practice
Medical-dental necessity is not age based, nor is it static. Each individual has different risks and medical-dental necessity. The idea of medical-dental necessity shouldn't be foreign to dental professionals. It simply requires documenting the reason a diagnostic or therapeutic procedure is needed.
--------------------------------------------------------------------
More articles
- Coach’s Corner for Dental Coding: New code for periodontal irrigation
- Coding Coach's Corner: The hygienist’s role in dental insurance coding
- 4 Coding Tips to Stop Leaving Money on the Table
--------------------------------------------------------------------
Clues to help determine medical-dental necessity
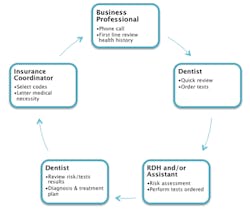
Good detective stories begin with the investigators checking a location, looking for clues related to the origin of the crime. Dental professionals and health-care providers must take on the role of investigator. The mouth is the portal of entry to our bodies, and when searched thoroughly, it can reveal clues to our patient's health status. Every case is different. Discovering the clues to TMD medical necessity takes the entire team (see Figure 1).
Evidence-based diagnosis
The first evidence-based diagnostic criteria to differentiate the most common forms of TMD and reach accurate diagnoses grounded in scientific evidence were published in February 2014. They are designed to help health professionals in North America, Europe, and Australia. The National Institute of Dental and Craniofacial Research website (rdc-tmdinternational.org/TMDAssessmentDiagnosis/DCTMD.aspx) has a complete list of evidence-based diagnostic instruments accessible for download. These tools are intended for use in both clinical and applied research settings, and will continue to evolve with practitioner input.
The National Dental Practice-Based Research Network (PBRN) is conducting a practice-based study on the management of TMD. PBRN (nationaldentalpbrn.org) is a network to gather practical science for the benefit of real, everyday clinical practice. Any practitioner can sign up to add to this body of evidence. There is no fee to enroll and no membership fee. All that is needed is Internet access and email. Internet access will be an important part of the research process. PBRN is currently recruiting practitioners and subjects to further explore the use of the EBD TMD criteria for a 2015 study.
A sample of TMD Pain Screener (see Figure 2) is one of the many accessible individual instruments, forms, and protocols that are part of the Complete TMD Instruments. Though these basic risk assessment questions are simple, they provide the basis of dental-medical necessity.
Basic data gathering and risk assessment determine the types of diagnostic tests that lead to diagnosis. The information from the tests along with the diagnosis leads to appropriate treatment planning. Risk and diagnostic tools will be used more widely in the future as a way to correctly diagnose a patient's health prior to recommending treatment. This is standard in medicine, and dental practitioners should also be testing first and determining medical-dental necessity before recommending a treatment plan.
Current TMD therapies
Treatment for TMD ranges from doing nothing (symptoms may resolve on their own) to full-blown surgery, and everything in between, from over-the-counter medications to bite guards, orthotic appliances, stress management, Botox injections, physical therapy, and more.
Botox therapy for TMD is not as well known to some hygienists. An excellent course on this subject, "Botulinum Toxin for Frontline TMJ Syndrome and Dental Therapeutic Treatment," can be found on IneedCE (ineedce.com). Whatever therapy is chosen must be supported by medical-dental necessity documentation for consideration under dental and/or medical plans.
State laws vary
Dental practices that routinely treat TMD have found that coverage is sometimes denied from dental and medical providers. Laws and rules for insurance vary from state to state. This denial has been challenged based on the fact that TMJ is a modified hinge-type joint between the mandible and the temporal bones and is no different than other joints in the body. Though treated most often by dental care professionals, TMD should not be excluded from coverage. Every state insurance commission has reviewed TMD within the medical coverage. Figure 3 shows the New York Insurance Department 2006 response to a request from a dental office after being denied coverage.
Over 20 states have added laws to cover TMD. This is one of the many reasons it is important to check with the payer to determine if coverage is available, and if so, what is covered and in what order.
Dentistry must move to an evidence-based diagnostic-centered care model in order to interact with the rest of health care through electronic health records. Coding is at the forefront of this process. Accurate diagnoses grounded in supportive scientific evidence that clearly determine the dental-medical necessity for the selected care is the best way to optimize coverage. Coding for TMD diagnostics and treatment involves the entire team.
Team cycle to determine dental-medical necessity Figure 1
Source: DentalCodeology: Jump Start Diagnostic Coding (DentalCodeology.com)
TMD-Pain Screener Figure 2
1. In the last 30 days, how long did pain last in your jaw or temple area on either side
a. No pain
b. Pain comes and goes
c. Pain is always present
2. In the last 30 days, have you had pain or stiffness in your jaw upon waking up
a. No
b. Yes
3. In the last 30 days, did the following activities change the pain (make it better or worse) in your jaw or temples on either side
a. Chewing on hard or tough food
i. No
ii. Yes
b. Opening your mouth or moving your jaw forward or to the side
i. No
ii. Yes
c. Jaw habits such as holding teeth together, clenching, grinding, or chewing gum
i. No
ii. Yes
d. Other jaw activities such as talking, kissing, or yawning
i. No
ii. Yes
Copyright Gonzales UM. No permission required to reproduce, display or distribute.
State of New York Insurance Coverage for the Nonsurgical Treatment of Temporomandibular Joint Disorders 2006 Figure 3
Q: May a health insurer exclude coverage for the nonsurgical treatment of TMJ disorders?
A: A health insurer may not specifically exclude coverage for the nonsurgical treatment of TMJ disorders. When assessing whether coverage for a TMJ disorder is available under a medical policy, the health insurer must make a factual determination on a case-by-case basis as to whether the TMJ disorder is dental or medical in nature. If the condition is determined to be medical, the health insurer must provide coverage, subject to the terms of the contract. If the condition is dental in nature, the insurer may exclude coverage based upon the permissible dental exclusion in Section 52.16(c) of N.Y. Comp. Codes R. & Regs. tit. 11, Part 52 (Regulation 62).
Q: May a dental insurer exclude coverage for the nonsurgical treatment of TMJ disorders?
A: It depends upon the terms of the insurance contract.
Q: If a dental insurer denies coverage entirely for the nonsurgical treatment of TMJ disorders, must the dental insurer apply the insured's payment toward satisfying the annual deductible under the dental policy?
A: It depends upon the terms of the insurance contract. However, dental insurers do not typically apply the costs of uncovered services toward satisfying any deductibles required by the contract.
Excerpt from: http://www.dfs.ny.gov/insurance/ogCO2006/rg060808.htm
PATTI DIGANGI, RDH, BS, holds a publishing license with the American Dental Association for Current Dental Terminology, and is an American Dental Association Evidence-Based Champion. CHRISTINE TAXIN has extensive training and experience in both dental and medical coding based on her roles as the administrator of a critical care department at Mt. Sinai Hospital, and management of a comprehensive multispecialty dental practice. Taxin and DiGangi's book, DentalCodeology: Jump Start Diagnostic Coding, is available at DentalCodeology.com.
Past RDH Issues