Preparing for influenza: Dental care providers are urged to help prevent spread of flu
by Noel Kelsch, RDHAP
In life there are very few things we can really predict. But there are two things we can do to help mold the future: preparedness and actions.
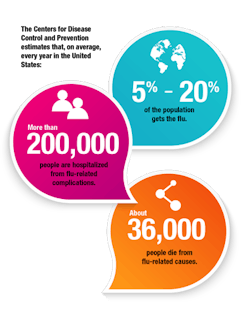
Influenza (flu) is an area that is ever-changing and unpredictable. The flu is a contagious respiratory illness caused by influenza viruses. It can infect the nose, throat, and lungs and cause mild to severe illness. Serious outcomes of flu infection can result in hospitalization or death. Some people-such as older people, young children, and people with certain health conditions-are at high risk for serious flu complications.
It's not possible to predict what this flu season will be like for a number of reasons. While flu spreads every year, the timing, severity, and length of the season usually varies from one season to another.1 Even the timing of the flu is not something that stays the same. In the past, it has peaked between December and February, but activity can start as early as October and end as late as May.
Cross-contamination: This disease can be spread in a number of ways: direct contact with mucous membrane; cross-contamination with clinical contact surfaces; and droplet transmission including sneezing and coughing, spreading the pathogens by large particle droplets that are carrying the microorganisms.
Most experts think that flu viruses are spread mainly by droplet transmission. People with flu can spread it to others up to six feet away. These droplets can land in the mouths or noses of people who are nearby or possibly be inhaled into the lungs. Less often, a person can get the flu by touching a surface or object that has flu virus on it, and then by touching his or her own mouth or nose or other mucous membrane.2
Period of contagiousness: Any health-care worker with flu symptoms should isolate, stay home, and get well. Flu can be transmitted one day before symptoms appear; that is why vaccinations are so important.
After developing symptoms, infected individuals are contagious for five to seven days. Some people, especially young children and those individuals with weakened immune systems, might be able to infect others for an even longer time. Infected individuals are instructed not to report to work or, if at work, to stop patient-care activities, don a facemask, and promptly notify their supervisor and infection control/occupational health personnel before leaving work. They are to be excluded from work until at least 24 hours after they no longer have a fever (without the use of fever-reducing medicines such as acetaminophen). Those with ongoing respiratory symptoms should be considered for evaluation by occupational health personnel to determine appropriateness of contact with patients.3
During that time, dental health-care personnel (DHCP) should not be working in the health-care setting or exposing others to the disease.4 Another issue here is the fact that people can be infected with the flu virus but have no symptoms. During this time, those persons may still spread the virus to others.5
Since health-care providers may never know that we are developing the flu and may be exposing high-risk clients, we are all asked to take vaccinations.
As DHCP, we all have the responsibility to do no harm. Our choices in vaccinations can directly impact the public. Yet one study found that only 31.6% are getting vaccinated in the dental setting for the flu.6 The CDC's Advisory Committee on Immunization Practices (ACIP) reported that the best way to protect against influenza is to receive an influenza vaccination every year. While anyone can get vaccinated, health authorities make specific recommendations for those at higher risk of complications. This includes adults 50 and older, children 6 months through 18 years of age, and anyone with a chronic medical condition (for example, asthma, diabetes, heart disease). Health-care workers, parents, and others who live or work around people at increased risk of influenza should get vaccinated as well to help reduce the risk of spreading the virus to susceptible people. Individuals with severe hypersensitivity to eggs and those who have had a previous vaccine-associated allergic reaction should avoid immunization.
The National Foundation for Infectious Diseases reassures that influenza vaccines have proven to be very safe.7 The inactivated vaccine has been available in the United States since the 1940s. It is approved for use in all persons six months of age and older. Mild and transient local reactions (for example, soreness, indurations) are the most common adverse events associated with inactivated vaccine. Systemic symptoms (for example, fever, malaise, chills) are rare (less than 1% of vaccine recipients) and usually transient, lasting one to two days.
The live attenuated vaccine has been available for use in the United States since 2003. It is approved for use only in healthy persons ages 2 to 49. ("Healthy" indicates persons who do not have an underlying medical condition that predisposes them to influenza complications.) The live attenuated vaccine is not approved for use in anyone outside this age range or persons with asthma, reactive airway disease, or other chronic pulmonary or cardiovascular conditions, metabolic disease (e.g., diabetes), renal disease, hemoglobinopathies (e.g., sickle cell disease), immunosuppression, and children receiving long-term aspirin therapy. Anyone receiving the live vaccine should avoid close contact with immunocompromised persons for 21 days.8,9
All high-risk persons should be vaccinated annually. For optimal protection, the following persons should be vaccinated annually:
- Adults 50 years of age and older
- Children 6 months through 18 years of age
- Children younger than 9 years of age being immunized for the first time will require two vaccines at specific intervals (see prescribing information for product used for acceptable dosing intervals)
- Health-care workers
Prevention: Inform patients ahead of time that if they have flu symptoms, they should not come into the dental setting for elective treatment. Educate staff about the symptoms and institute a program for evaluation of the patient's symptoms. All staff should be trained to look for and evaluate symptoms:
- Fever (It's important to note that not everyone with influenza will have a fever.)
- Cough
- Sore throat
- Runny or stuffy nose
- Body aches
- Headache
- Chills
- Fatigue
- Sometimes diarrhea and vomiting
The Centers for Disease Control and Prevention says, "Patients with an acute respiratory illness may present for dental treatment at outpatient dental settings. The primary infection control goal is to prevent transmission of disease. Early detection of a suspected or confirmed case of influenza and prompt isolation from susceptible persons will reduce the risk of transmission. To prevent the transmission of respiratory infections in health-care settings, including influenza, respiratory hygiene/cough etiquette infection control measures should be implemented at the first point of contact with a potentially infected person."
There are many things we do have control of in health care. Vaccination, developing an action plan, and preventive measures can help us all do no harm. RDH
Action plan: Review with the entire staff!
- Elimination of potential exposures (for example, deferral of ill patients and source control by masking coughing individuals).
- Engineering controls that reduce or eliminate exposure at the source without placing primary responsibility of implementation on individual employees.
- Routine cleaning and disinfection strategies used during influenza season can be applied to the environmental management. Use of barrier protection and hospital grade disinfectants according to label direction is a must. Find more information at cdc.gov/ncidod.
- Administrative controls including sick-leave policies and vaccination that depend on consistent implementation by management and employees.
- Patient and dental health-care workers should perform hand hygiene (hand washing with nonantimicrobial soap and water, alcohol-based hand rub, or antiseptic hand wash) after contact with respiratory secretions and contaminated objects/materials.
- Personal protective equipment (PPE) for exposures that cannot otherwise be eliminated or controlled. PPE includes gloves, surgical facemasks, respirators, protective eyewear, and protective clothing (gowns). Limit the areas that PPC is allowed.
- Encourage all dental health-care personnel to receive seasonal influenza vaccinations.
- Use patient-reminder calls to identify patients reporting influenza-like illness and reschedule nonurgent visits until 24 hours after the patient is free of fever, without the use of fever-reducing medicine.
- Identify patients with influenza-like illness at check-in; offer a facemask or tissues to symptomatic patients; follow respiratory hygiene/cough etiquette (see CDC guidelines); and reschedule nonurgent care. Separate ill patients from others whenever possible if evaluating for urgent care.
Stay up-to-date: Guidance on seeing any patients with symptoms can be found in the October 2006 "Interim Guidance on Planning for the Use of Surgical Masks and Respirators in Healthcare Settings during an Influenza Pandemic" (pandemicflu.gov/plan/healthcare). Most offices will need to refer to the hospital setting with dental care facilities, because they do not have the air filtration (airborne infection isolation room with negative pressure air handling with six to 12 air changes per hour) or required personal protective equipment such as an n95 mask.
NOEL BRANDON KELSCH, RDHAP, is a syndicated columnist, writer, speaker, and cartoonist. She serves on the editorial review committee for the Organization for Safety, Asepsis and Prevention newsletter and has received many national awards. Kelsch owns her dental hygiene practice that focuses on access to care for all and helps facilitate the Simi Valley Free Dental Clinic. She has devoted much of her 35 years in dentistry to educating people about the devastating effects of methamphetamines and drug use. She is a past president of the California Dental Hygienists' Association.
References
1. http://www.cdc.gov/flu/about/season/flu-season-2014-2015.htm
2. http://www.cdc.gov/flu/about/disease/spread.htm
3. http://www.cdc.gov/flu/professionals/infectioncontrol/healthcaresettings.htm
4. http://www.cdc.gov/flu/keyfacts.htm
5. http://www.cdc.gov/flu/about/disease/spread.htm
6. Wicker S1, Rabenau HF, Betz W, Lauer HC. Attitudes of dental health-care workers toward the influenza vaccination. 2012 Jul;215(4):482-486. doi: 10.1016/j.ijheh.2011.08.005. Epub.
7. Glezen WP. Serious morbidity and mortality associated with influenza epidemics. Epidemiol Rev 1982;4:25-44.
8. Jackson LA, Holmes SJ, Mendelman PM, et al. Safety of a trivalent live attenuated intranasal influenza vaccine, FluMist, administered in addition to parenteral trivalent inactivated influenza vaccine to seniors with chronic medical conditions. Vaccine 1999;17:1905-1909.
9. Izurieta HS, Haber P, Wise RP, et al. Adverse events reported following live, cold-adapted, intranasal influenza vaccine. JAMA 2005;294:2720-2725.