Trigeminal neuralgia: The suicide disease
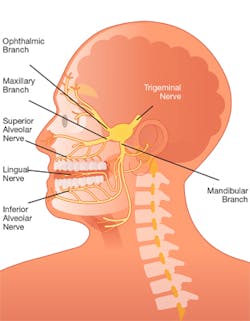
Trigeminal neuralgia (TN) is characterized by excruciating pain in the distribution of one or more branches of the fifth cranial nerve. In fact, it is considered to be the worst pain known to medicine.
I became inspired to write about TN because my late mother and her brother were both afflicted with the condition, and in the past month at my office, I saw two patients on two consecutive days, both of whom suffer from TN. Yet, throughout my 30-plus years of clinical practice, I had never before encountered any other cases. Since TN tends to be diagnosed in middle- to older-aged women, as hygienists, we will potentially come in contact with the huge demographic of baby boomer patients who may be affected by this awful disease. It makes sense for us to learn as much as we can about it.
TN is a rare condition. The pain typically lasts only seconds, but while it is happening, the person suffering will find it to be unbearable. Hence, it has been given the nickname, “the suicide disease.” While not considered fatal, many who suffer from this condition attempt or complete suicide, with a suicide completion rate1 of approximately 25% (double that of the general population).2
Having observed my mother diagnosed with TN in her 50s and watching what she had to endure was gut-wrenching for me. My uncle, who was a dentist practicing in Rhode Island, underwent surgery early in life, which afforded him a permanent solution from the outset. I will discuss treatment options later in this article.
What is the cause of this debilitating condition? Most experts agree that the etiology is segmental demyelination of trigeminal sensory nerves in the nerve root or brain stem. The demyelination is due to chronic compression of the nerve root where it exits from the pons.3
There can also be a link to those with multiple sclerosis. Incidence is approximately 4 per 100,000 of the population, which gradually increases with age. The average age of onset is 60. Rarely is anyone diagnosed before 40 years of age.3
The pain occurs in episodes; individuals can go days, months, and even years being pain free. Yet, certain triggers can set off the pain. As clinical hygienists at chairside treating patients with TN, it behooves us to understand more, as this can have a profound impact on our treatment. Yawning, speaking, chewing, brushing teeth, and simply touching one’s face can all potentially set off what has been described as an electric lightning bolt of intense pain. Think about an extraoral fulcrum you might use during instrumentation. Even the lightest, featherlike finger-rest could prove to be disastrous as perceived by TN patients. The intense pain is typically unilateral, lasting several seconds to several minutes, and can occur a few times a day or hundreds of times a day.
The diagnosis of TN is based on history alone, after hearing the patient’s reported description of the pain. Remission can occur but the periods between relapses seem to shorten as the individual ages. The condition can lead to depression because daily life activities can be so impaired. Experts find that symptoms worsen over time and become less responsive to medication, despite dosage increases and the addition of other agents.4
What constitutes treatment success for TN? There are different definitions of success depending on whether the treatment intervention is medical or surgical. If at least half of pain relief compared to baseline readings occurs with pharmacological therapy, this is considered success. However, with surgical studies, measurements are different. Complete pain relief is the goal, so this would be considered treatment success.
Carbamazepine is considered the gold standard for initial medical treatment of TN symptoms. Carbamazepine has been shown to increase pain relief compared with a placebo, but it also increases adverse effects such as drowsiness, dizziness, rash, liver damage, and loss of muscle control. All of these are potential causes for concern.
My mother underwent regular blood work to evaluate her liver enzymes when she took this medication, but thankfully she had none of the adverse side effects. Studies evaluating durability of response with carbamazepine are few. The consensus of experts suggests that it may have a greater than 50% failure rate for long-term (five to 10 year) pain control.4
One interesting relevant factor is that it is considered unethical to test other drugs potentially beneficial to treating the disease simply because to give a person a placebo in a clinical trial and have him or her endure the consequences of having no potentially effective medication would be intolerable. Of note, my mother gained 12 years of relief before carbamazepine stopped working for her.
Based on the strength of published evidence, carbamazepine remains the best supported standard medical treatment for TN. Other medications include oxcarbazepine as another first-line therapy. Lamotrigine and baclofen are considered second-line treatments.
If and when medications are no longer effective or tolerated, surgical options that are considered the most promising alternatives include microvascular decompression, stereotactic radiofrequency lesioning (one type is Gamma Knife radiosurgery), and percutaneous rhizotomies. The goal of surgery is either to stop a blood vessel from compressing the trigeminal nerve or to sever the nerve that’s causing the pain.
With microvascular decompression (MVD), the neurosurgeon will make an incision behind the ear on the side that is experiencing pain, exposing the trigeminal nerve. The surgeon then relocates or removes any blood vessels that are compressing the nerve and may insert a small pad to prevent contact with the nerve. If no blood vessels are compressing, the surgeon will perform a rhizotomy, which actually severs the nerve. Aside from normal surgical risks, another concern is facial paralysis that may be temporary or permanent as a consequence of the surgery. There is a strong international consensus that MVD represents the gold-standard surgical procedure for TN and that, patient’s condition allowing, MVD is the procedure of choice for medically intractable TN.5
Stereotactic radiofrequency lesioning is a less invasive procedure than microvascular decompression. A radiologist and neurosurgeon work together to pinpoint the precise location of the nerve, and then high heat is used to destroy only the pain portions. This will leave other sensation intact, theoretically. Finally, stereotactic radiosurgery is employed. This is a noninvasive specialty that does not involve cutting. Beams of highly focused radiation are directed at the trigeminal nerve. The radiation beam damages the trigeminal nerve but does not destroy it completely. The Gamma Knife is one type of stereotactic radiosurgical treatment; it is painless and can be performed on an outpatient basis.
Another treatment that is considered “last line” is a percutaneous rhizotomy, which is the implantation of a pain stimulator beneath the skin on the back of the head. This stimulator sends electrical impulses along the nerve channel, which confuses it from being able to carry pain. The stimulator runs on batteries that must be changed over time.
Neurosurgeons consider each individual case before recommending the approach most likely to provide relief. Each surgical method has pros and cons. The age of the patient when diagnosed with TN and the disease progression and severity are all factors to be considered, as well as any risk factors. A substantial proportion of those who undergo invasive procedures indicates that the majority of these patients will require further or repeated treatments in the future. In a study sponsored by Biogen, overall data indicated a high burden-of-illness associated with TN and its treatment and unmet needs with current therapies.6
When I treated the two patients afflicted with TN in my office, I was very apprehensive. It was important for me to be aware of the vicinity of each of their trigger points so that I might steer clear. One patient was 80 years old and had been taking anti-seizure medication as treatment for a decade. Of late, her medication had become less effective. I was able to share with her my mother’s experience with that same medication, as well as her ultimately successful surgical intervention. The other patient was 63 and had been recently diagnosed with TN. She was also taking carbamazepine, and her condition seemed to be well under control.
I noted inflammation in the gingival tissues of the trigger point area (No. 11 facial) in the 80-year-old patient, who admitted that she avoided brushing there because she was so fearful about setting off the pain. This was around No. 11 facially. I was able to gently debride her. The challenge for this patient in terms of her self-care, as well as for any clinician working in the area, is that there is no consistency as to whether or not the pain will happen. I am grateful my two hygiene sessions with these patients were uneventful.
When my mother decided to have surgery at age 90, it was due to the fact that her quality of life had deteriorated to the point of abysmal. A once-robust five-foot-six, 145-pound woman had certainly lost some of her vertical dimension as a natural part of the aging process, but because chewing food was a trigger that would often set off her pain, she ate minimally and, as a consequence, had lost a significant amount of weight. Her pain control medications had long since ceased affording her any degree of relief, and after a consult with a neurosurgeon, she finally made the decision to go forward with surgery. She was advised that there was a possibility of permanent, facial paralysis in one or more areas of her face. Although she was concerned, my sister and I encouraged her to go ahead with surgery because we felt that her life could only improve.
My sister accompanied my mother to the Gamma Knife treatment. Although I was 250 miles away in New Jersey, I was determined to help my mother feel comfortable during the procedure. Because I am a Reiki master, I was able to send Reiki energy to her from the moment she entered the surgical suite and during post-op. Mom later told my sister that, even though she was extremely apprehensive, she was completely comfortable and had no recollection of pain.
I remember speaking to my sister as Mom was being driven home. Apparently, Mom was talking and laughing, and was able to eat soft foods within a couple of hours of the treatment. Ironically, her learned behaviors while eating had been based on years of complete tenuousness about the impact chewing could potentially have on her pain, and it was almost impossible for her to completely get away from that.
Even postsurgery, chewing food would continue to be slow and ever guarded, with a hand that would go up near her left cheek as if to shield herself from the agony she had come to know so well. Thankfully that pain never returned, and time without it helped her to normalize to some extent. My mother gained some of her weight back, and while she lived only seven months after the surgery, she spent those months relishing some of the foods she loved and had lived without for so long.
My recommendation to anyone who is suffering from this horrible disease would be to consider surgical intervention. Anecdotal evidence from numerous respondents who ultimately chose surgery appears to be that they overwhelmingly express regret about not choosing intervention sooner. I wish that had been the case for my mother. Life is short and precious, and eating good foods is one of the remaining joys that should not have to be curtailed for any of us in our elder years. I wholeheartedly recommend the neurosurgeon, Emad Eskandar, MD, of Massachusetts General Hospital, from the bottom of my heart as the individual who had such a positive impact on my mother’s life.
References
1. Tavernise S. U.S. suicide rate surges to a 30-year high. The New York Times website. https://www.nytimes.com/2016/04/22/health/us-suicide-rate-surges-to-a-30-year-high.html?_r=0. Published April 22, 2016.
2. Why trigeminal neuralgia is considered the “suicide disease.” Arizona Pain Specialists website. https://arizonapain.com/trigeminal-neuralgia-suicide-disease/. Published September 26, 2016.
3. Chen G, Wang X, Wang L, Zheng J. Arterial compression of nerve is the primary cause of trigeminal neuralgia. Neurol Sci. 2014;35(1):61-66. doi: 10.1007/s10072-013-1518-2.
4. Zakrzewska JM, Linskey ME. Trigeminal neuralgia. BMJ Clin Evid. 2014;2014:1207.
5. Burchiel KJ. Trigeminal neuralgia: new evidence for origins and surgical treatment. Neurosurgery. 2016;63(suppl 1):52-55. doi: 10.1227/NEU.0000000000001276.
6. Wu N, Lee J, Zakrzewska, Werneburg B, Hoffman D, Liu Y. Trigeminal neuralgia: pharmacotherapy and surgical treatment patterns in the United States. J Pain. 2017;18(4)(suppl):69S. doi: https://doi.org/10.1016/j.jpain.2017.02.352.
Eileen Morrissey, MS, RDH, is a practicing clinician, educator, speaker, and writer. She is an adjunct dental
hygiene faculty member at Rowan College at Burlington County. Eileen lectures nationally. Contact her at [email protected] or (609) 259-8008. Visit her website at eileenmorrissey.com.
About the Author
Eileen Morrissey, MS, RDH
Eileen Morrissey, MS, RDH, is a practicing clinician, educator, speaker, and writer. She is an adjunct dental
hygiene faculty member at Rowan College at Burlington County. Eileen lectures nationally. Contact her at [email protected] or (609) 259-8008. Visit her website at eileenmorrissey.com.