Decoding the language of clinical attachment: What every hygienist needs to know
What you'll learn in this article
-
The critical difference between clinical attachment level and clinical attachment loss—and why it matters for diagnosis
-
How software “auto-corrections” can misrepresent periodontal health and complicate staging and grading
-
Why understanding apical migration is essential for accurate assessment and effective treatment planning
Listen to the article on our podcast!
Part 1 of 3
In periodontal assessment and treatment, clinical attachment levels play a pivotal role in determining the health of the periodontal tissues.1 However, confusion often arises in differentiating between clinical attachment level and clinical attachment loss—two terms that, though related, have distinct meanings and implications for diagnosis. Understanding this difference is crucial for accurately assessing the severity of periodontal disease and for establishing appropriate treatment plans.
A common challenge in modern practice lies in the automatic correction of clinical attachment levels by many periodontal charting software systems. These systems often default to using probing depth as a substitute for clinical attachment loss, which can lead to significant inaccuracies. In essence, this software “auto-
correction” falsely indicates that a patient has experienced clinical attachment loss when in reality, probing depth alone does not account for the true loss of attachment tissue. This error distorts the assessment and complicates the classification of patients, particularly when trying to determine if a patient may be diagnosed with irreversible periodontal disease.
So, why does this matter? Understanding the nuances of clinical attachment and apical migration is more important than we may realize. For many of us, these terms are often used interchangeably without fully grasping their impact on diagnosis and treatment. It is easy to overlook how apical migration of the junctional epithelium and a stable clinical attachment level are not the same thing. However, many clinicians overlook this distinction, which results in inaccurate staging and grading of periodontal disease.
A thorough reexamination of core periodontal concepts is essential to ensure clarity and consistency in clinical application. A deeper understanding of these principles supports accurate assessment and promotes more effective, evidence-based patient care.
In this three-part article series, we will examine how emerging technologies—particularly advancements in artificial intelligence—are contributing to a deeper understanding of anatomical structures and periodontal architecture, thereby refining our diagnostic and treatment capabilities.
By reinforcing foundational knowledge and integrating current advancements, the goal is to strengthen clinical decision-making and improve patient outcomes. So, let’s dive in and uncover the truth behind clinical attachment—together.
Clinical attachment level and clinical attachment loss
While many resources describe clinical attachment level (CAL) and clinical attachment loss (CAL) as the same, it’s important to note that using these terms interchangeably can lead to confusion.
In a healthy periodontium, the clinical attachment level is considered optimal. This level is measured from the cementoenamel junction (CEJ),2 which serves as a stable, nonmoving reference point for anchoring the epithelial attachment to the tooth surface. In this state of health, there has been no clinical attachment loss—the epithelium remains securely anchored to the CEJ, and there is no detachment of the collagen fibers from the root surface.3
Similarly, in a state of gingivitis, there is no clinical attachment loss. While the relative attachment level remains optimal, indicating no downward migration of the attachment, other probing parameters, such as pocket depth, may show changes. These changes are typically due to pseudopocketing, where the gingival margin appears enlarged but there is no actual loss of attachment. This condition may present with deeper pocket depths, but the attachment remains intact.
Thus, it’s crucial to differentiate between a healthy periodontium, where CAL is optimal and there is no attachment loss, and a periodontal disease state, where clinical attachment loss would be observed as a result of the detachment and apical migration of the junctional epithelium. Understanding this distinction ensures that periodontal health is accurately assessed and appropriately managed.4
Apical migration of the junctional epithelium
Apical migration refers to the downward movement of the junctional epithelium along the root surface of the tooth. This process occurs in response to inflammation and is a hallmark of periodontal disease. As the junctional epithelium migrates apically, it detaches from the tooth surface, which results in clinical attachment loss. Unlike in health, where the attachment remains stable at the CEJ, apical migration signifies the loss of attachment and the gradual deepening of periodontal pockets.
The junctional epithelium plays a critical role in maintaining the integrity of the attachment of the gingival tissues to the tooth. It forms a protective barrier against bacterial invasion, and its location at the CEJ in a healthy state is essential for periodontal health. When inflammation sets in, the junctional epithelium starts to migrate apically, signaling the loss of attachment and the progression from gingivitis to periodontitis. This migration is a key factor in the development of periodontal pockets, which are deeper areas of bacterial accumulation, further exacerbating the condition.
Apical migration is distinct from clinical attachment, which refers to the position of the attachment apparatus (the junctional epithelium and connective tissue fibers) relative to the CEJ. As previously noted, in a healthy periodontium the junctional epithelium is securely anchored at or near the CEJ, with no migration or loss of attachment. Clinical attachment represents the ideal, where there is no detachment from the root surface.
Understanding apical migration as clinical attachment loss and its distinction from determining optimal versus suboptimal clinical attachment levels is crucial for accurately diagnosing and staging periodontal disease. It is the shift from attachment stability to apical migration that marks the transition to irreversible tissue damage, and it serves as the foundation for more advanced periodontal interventions.
Periodontal anatomy and confusion in staging and grading of periodontal disease
The distinction between clinical attachment level and apical migration plays a significant role in the accurate staging and grading of periodontal disease. However, this difference is often misunderstood or misinterpreted, leading to confusion that can impact diagnosis and treatment planning.
When periodontal charting software or clinical assessments use probing depth as a proxy for clinical attachment level, it fails to consider that true clinical attachment level is determined by whether there is apical migration of the junctional epithelium.5 In automated systems, probing depths alone may appear to create clinical attachment loss, but without understanding the true clinical attachment loss that occurs with apical migration, a clinician may be led to an incorrect diagnosis.
For example, in cases of gingivitis, probing depths may increase due to pseudopocketing caused by gingival swelling, but there is no actual loss of attachment. In these cases, attachment loss is not present, even though the probing depths are greater than usual. Oftentimes, we consider a greater probing depth to be a “deeper” depth, when in this example, the presence of disease is not one that includes apical migration and attachment loss; using an automated system indicating the pocket depth is also the clinical attachment level may falsely lead the clinician to stage and grade a case of gingivitis.
Additionally, using apical migration as the only metric for diagnosing disease can complicate the understanding of disease progression. Clinicians who use clinical attachment loss alone may create confusion when determining whether a patient is in a stage of active disease or in a state of periodontal stability with recession but no further attachment loss. As a result, clinicians may misinterpret the stage of disease, potentially overdiagnosing patients who are stable or underdiagnosing those with active disease.6
Understanding clinical attachment level in various diagnoses
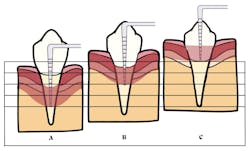
Interdental clinical attachment loss is preferred for staging and grading periodontal disease, because it offers a more accurate and consistent assessment of tissue destruction than probing depths alone (figure 1).
Consistency in measuring this coronal gingival margin has been shown to be limited, with significant variability among clinicians.7 The location of the gingival margin relative to the CEJ can differ depending on the stage of passive eruption. In periodontally healthy individuals, the gingival margin typically extends about 2 mm above the CEJ at midfacial sites and ranges between 2 mm and 3.5 mm at interproximal areas. Certain conditions, such as gingival overgrowth or altered passive eruption, may further increase this coronal gingival dimension.
In terms of grading periodontal disease, confusion around apical migration can impact the ability to assess disease risk accurately. Grading assesses the rate of disease progression based on risk factors and clinical attachment loss. However, without recognizing the role of quantifying the amount of apical migration over a determined spectrum of time, clinicians may misclassify patients as having a high or low rate of progression.
Ultimately, recognizing the true attachment loss from apical migration and distinguishing it from other factors such as pseudopocketing is essential for properly understanding if staging and grading of active periodontal disease is appropriate for diagnostics. The confusion surrounding these terms and their impact on measurements can undermine the accuracy of diagnosis, treatment planning, and ultimately, patient outcomes. Understanding these nuances ensures that clinicians can make more informed, precise decisions about how to manage periodontal health effectively.
Part two of this series will dive into the clinical application of staging and grading, the advancement of technology in integrating diagnostic decisions, and the opportunity for clinical practitioners and educators to better scrutinize their role in understanding clinical attachment level/loss.
Editor's note: This article appeared in the October 2025 print edition of RDH magazine. Dental hygienists in North America are eligible for a complimentary print subscription. Sign up here.
References
- Pihlstrom BL. Measurement of attachment level in clinical trials: probing methods. J Periodontol. 1992;63(12 Suppl):1072-1077. doi:10.1902/jop.1992.63.12s.1072
- Clark DC, Quee TC, Bergeron MJ, Chan ECS, Lautar-Lemay C, De Gruchy K. Reliability of attachment level measurements using the cementoenamel junction and a plastic stent. J Periodontol. 1987;58(2):115-118. doi:10.1902/jop.1987.58.2.115
- Dannan A. The clinical attachment revisited: a clinical opinion introducing the (A-LEVEL), (A-GAIN), and (A-LOSS). Mathews J Dent. 2024;8(1):44. doi:10.30654/MJD.10044
- Michalowicz BS, Hodges JS, Pihlstrom BL. Is change in probing depth a reliable predictor of change in clinical attachment loss? J Am Dent Assoc. 2013;144(2):171-178. doi:10.14219/jada.archive.2013.0096
- Barbosa VL, Angst PDM, Stadler AF, Oppermann RV, Gomes SC. Clinical attachment loss: estimation by direct and indirect methods. Int Dent J. 2016;66(3):144-149. doi:10.1111/idj.12218
- Mdala I, Olsen I, Haffajee AD, Socransky SS, Thoresen M, de Blasio BF. Comparing clinical attachment level and pocket depth for predicting periodontal disease progression in healthy sites of patients with chronic periodontitis using multi-state Markov models. J Clin Periodontol. 2014;41(9):837-845. doi:10.1111/jcpe.12278
- Wang IC, Chan HL, Johnson GK, Elangovan S. Assessment of negative gingival recession: a critical component of periodontal diagnosis. Appl Sci. 2022;12(14):7015. doi:10.3390/app12147015
About the Author

Marianne Dryer, MEd, RDH
Marianne Dryer, MEd, RDH, is a dynamic speaker, educator, and consultant in curriculum development. She has lectured nationally and internationally on periodontal instrumentation with a focus on ultrasonic technique, risk assessment, infection prevention, and radiology technique. Her experience in dentistry spans more than 30 years. She is currently the Director of Dental Sciences at Cape Cod Community College. She is a graduate of Forsyth School for Dental Hygienists, Old Dominion University, and received her master’s in education from St.Joseph’s College of Maine. Contact her at [email protected] or through her website at mariannedryer.com.

Katrina M. Sanders-Stewart, MEd, BSDH, RDH, RF
A clinical dental hygienist, author and international speaker, Katrina is passionate about elevating the dental profession by creating an undeniable movement that educates, encourages, and empowers the profession to rise in its power. Known as the “Dental WINEgenist™,” she pairs her desire for excellence in the dental industry with her knowledge and passion for wine. She is the Clinical Liaison for Hygiene Excellence at AZPerio, founder of Sanders Board Preparatory and has been published in various publications including RDH Magazine and Dental Academy of Continuing Dental Education. Recently, Katrina proudly received the University of Minnesota Distinguished Alumni Award and the 2024 Sunstar Award of Distinction. @TheDentalWINEgenist [email protected].