Preventive care and a fixed implant denture
Dear Dianne,
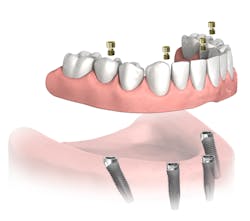
I have been temping full-time for the past six months. This week I received a call from a dentist’ office where I had temped, and he told me that one of the patients I saw was very upset after I cleaned her teeth. The patient has a permanent fixed-implant full upper denture, as well as crowns and implants on her lower arch. She is a geriatric patient with poor oral hygiene. She had indicated that she didn’t floss often, and there was a moderate amount of plaque underneath her denture on the upper, in addition to calculus and moderate plaque along the gumline.
I was not given instructions on what to do or not do, so with one hour to spend on this patient, I used regular dental hygiene instruments along with a power scaler to flush out the plaque and blood under her upper denture. I used coarse polish to polish her upper denture (which I have been doing for years).
After the patient left the office, she called back to say that her dentures felt different, something about a “space” that wasn’t there before. The dentist had her come back in to the office, but he didn’t see anything broken or damaged with her upper denture or anywhere in her mouth.
Now I am questioning myself about what I could be legally responsible for if the patient decides to file a complaint. My notes from that day are very generic, and I don’t feel confident in the fact that I used coarse polish to polish her dentures.
What should I do when given an hour for denture wearers? What is the proper way to clean stains, calculus, and plaque from dentures? What are the dos and don’ts with patients like this?
I don’t feel confident in what I used or what I did to give this patient the best care. Plus, I felt embarrassed about asking the dentist when I am supposed to be knowledgeable (I have nine years of experience as a registered dental hygienist).
I look forward to hearing your professional advice.
Respectfully,
Needing Answers, RDH
Dear Needing,
Across the country, there are all kinds of dental practices, from state-of-the-art everything, implant-only practices, to small bread-and-butter practices that focus mainly on restorations and palliative care. In between those two extremes is a wide continuum of dental practices that offer many levels of care. A hygienist typically will become proficient in offering preventive care to patients in the practice where he or she is employed. If the doctor does not recommend or provide implant dentistry, obviously the hygienist will lack insight into preventive care for implants. Further, in a temp situation, you never know what you might see. So, you are not at fault for being unsure about the correct protocol. Many of your colleagues have never seen a fixed implant denture in a patient’s mouth.
There are two other problems related to preventive care and implant patients. First, there appears to be considerable disagreement among doctors who place implants as to the best cleaning methods. For example, some say to teach patients to floss, while others say to avoid floss. Second, some say it’s OK to probe, while others say to avoid probing implants.
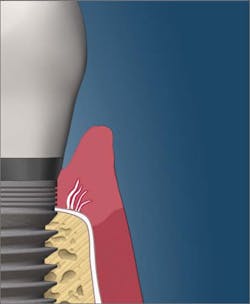
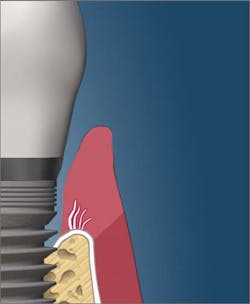
The dean of students at the Toronto College of Dental Hygiene, Boris Pulec, DDS, wrote an interesting article titled, “Tell your patients to stop flossing and your hygienist to stop checking pocketing.”1 Dr. Pulec has placed thousands of implants, and he states that there are several causes of peri-implantitis, including traumatic oral self-care. According to his article, “Many dental practices instruct their patients to floss the dental implants the same way they floss natural teeth. Break the contact and then force it into the pocket from both sides and move back and forth. The floss is thin and the pressure is high enough to easily break any peri-implant soft-tissue seal. In this seal, the junctional epithelium still attaches to the implant surface via hemidesmosomes, but the gingival fibers do not insert into the implant as they do with natural teeth.” This same article also recommends against probing dental implants, as the probe can penetrate the fragile soft-tissue seal and create pathways “through which opportunistic bacteria can gain access to bone and propagate its loss (figures 1 and 2).”
An article published in Clinical Oral Implants Research suggests that the small shards of floss that are inadvertently left after flossing implants is a possible cause of peri-implantitis. In the study, 10 cases of peri-implantitis were presented. Nine of the cases completely resolved with the cessation of flossing.2
Another question that emerges is whether it is permissible to use ultrasonic scalers on implants. Dr. Pulec and others believe that the vibration created by power scalers has the potential to loosen implant screws, which can cause dental implant failure. Other periodontists feel that the power scaler is permissible if used very gently and carefully.
Most of us were taught that great care must be exercised not to scratch the implant. Two types of implant scalers, titanium and resin, are available. My experience with resin scalers is they are about as useful as using the side of a credit card to scrape calculus. Titanium scalers are somewhat better, but I’ve seen calculus on the necks of implants that was all but impossible to remove without using the power scaler. Everybody agrees that the calculus has to be removed.
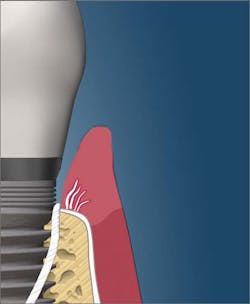
John A. Hodges, DDS, runs a practice dedicated solely to dental implant services in Covington, Washington. He wrote an interesting article that was published in DentistryIQ in June 2018, titled “Hygiene protocol for full-arch All-on-4 fixed bridges.”3 In the article, Dr. Hodges discusses some aspects of preventive care as well as how denture design can affect the hygienist’s ability to clean (figure 3).
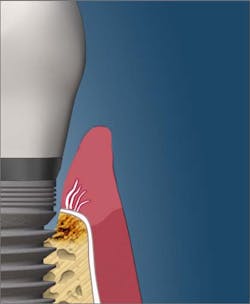
The design of the implant denture can be problematic. Dr. Hodges shares that when the implant denture has a concave intaglio surface, it creates a hygienic nightmare for the patient that can lead to inflammation, fungal infections, and denture fracture (figure 4).
If the denture is designed with a convex intaglio, it will be easier to keep clean (figure 5).
As we are aware, some people are more prone to calculus buildup than others. If a patient builds up calculus on a provisional appliance, it is certain that there will be calculus buildup on the final fixed appliance. In those cases, Dr. Hodges recommends removal of the appliance when necessary to facilitate cleaning. However, frequent removal has the potential of damaging the thread pattern in the implant, which may necessitate the replacement of expensive implant screws (figure 6).
Both Drs. Hodges and Pulec feel that the use of a Waterpik is a good and acceptable way to help with home care, but only on low power. High power has the potential to damage the soft-tissue seal.
Here are some tips to remember when providing preventive care for implant denture patients that I have learned from experts:
1. The denture can be scaled with titanium or stainless steel instruments if there are deposits that need to be removed.
2. Use titanium scalers to scale around implants.
3. You can use the side of a power scaler tip to break up calculus on the outside of a denture, but you must exercise extreme caution. Never use the tip; you may create stress fractures in the acrylic or porcelain.
4. Use intraoral polishing burs or stones to remove tenacious calculus on the denture, and then use porcelain or acrylic polishers intraorally to polish the adjusted areas.
5. Polish the denture with a nonabrasive acrylic polishing paste, such as diatomaceous earth or silica paste. For heavy stain on acrylic, Dr. Hodges recommends using slow-speed intraoral porcelain polishers or even slow-speed Brownies and Greenies.4
6. Home-care instructions for patients should include items designed to facilitate cleaning around implants. Soft toothbrushes, Sulcabrushes, and rubber tip stimulators are excellent choices for home care (figures 7, below, and 8, above). Teaching patients about Waterpik use on medium to low power is also a good method for removing food debris and keeping the tissue healthy.
8. Flossing under fixed bridges has been recommended for several years, but there appears to be a growing body of evidence against flossing due to the possibility of shredding. It would be most prudent to ask the doctor what he or she recommends. There is also disagreement among implant doctors about using power brushes that vibrate. Again, ask the doctor for his or her preferences.
I agree with you that polishing the denture intraorally with coarse paste was not a good idea. It would have been better to have used something nonabrasive that is designed for acrylic, such as a silica paste or diatomaceous earth.
According to my friend, Susan Wingrove, BS, RDH, an expert on implant maintenance, Preventech has a fine grit paste, called Next, that is pumice free and contains less-abrasive diatomaceous earth (jeweler’s rouge). Ivoclar Vivadent’s fine grit paste is also pumice free and contains silica.6,7 Both products are kinder to all restored tooth surfaces and dental implants than pumice.
Another way to polish is by using a special subgingival polishing device that uses glycine powder. Subgingival air polishing with glycine powder has been found to be efficacious for treating peri-implantitis.8 Glycine is a naturally occurring amino acid and used by the human body to build up proteins. It is water soluble and has a nonsalty, pleasant taste.
Most likely, the “space” that the patient noticed was created where you removed calculus. Many of us have had experiences with patients who remark that they can feel “holes” in between their teeth when we remove big chunks of calculus.
The clinical dilemma you faced had more to do with a lack of experience rather than a lack of skill. My hope for you is that, in the future if you are faced with a similar experience, you will not feel embarrassed to ask the dentist if there are any special considerations, given you have not previously seen a patient like this. There’s no shame in discreetly asking if there are any special considerations.
If the patient files a complaint against you with your state board (which I doubt will happen), you might be required to answer some questions. But since the doctor did not find any problems after you provided care, I don’t think you have any worries.
The dilemma you shared provided an opportunity for me to do research on how to provide preventive care appropriately for patients with fixed implant dentures. My sincere appreciation goes to all of the clinicians and companies that provided input for this article. Information about this topic is continuing to evolve as the number of people with implant-supported dentistry continues to grow.
All the best,
Dianne
References
1. Pulec B. Tell your patients to stop flossing and your hygienist to stop checking pocketing. Dentalimplantlife.com website. http://www.dentalimplantlife.com/articles/dentalimplantlife.com_Non-Flossing-article.pdf. Published 2012.
2. van Velzen FJJ, Lang NP, Schulten EAJM, ten Bruggenkate CM. Dental floss as a possible risk for the development of peri-implant disease: an observational study of 10 cases. Clin Oral Implants Res. 2016;27(5):618-621. doi:10.1111/clr.12650
3. Hodges JA. Hygiene protocol for full-arch All-on-4 fixed bridges. DentistryIQ website. https://www.dentistryiq.com/clinical/implantology/article/16367646/hygiene-protocol-for-fullarch-allon4-fixed-bridges. Published June 27, 2018.
4. Abrasives. Shofu Dental Corporation website. https://www.shofu.com/en/products/abrasives/stones
5. IoTech International home page. https://iotechinternational.com/
6. Wingrove S. Wingrove Dynamics home page.
7. Preventech home page. https://preventech.com/
8. Sahm N, Becker J, Santel T, Schwarz F. Non-surgical treatment of peri-implantitis using an air-abrasive device or mechanical debridement and local application of chlorhexidine: a prospective, randomized, controlled clinical study. J Clin Periodontol. 2011;38(9):872-878. doi:10.1111/j.1600-051X.2011.01762.x
DIANNE GLASSCOE WATTERSON, MBA, RDH, is an award-winning author, speaker, and consultant. She has published hundreds of articles, numerous textbook chapters, and three books. Her new DVD on instrument sharpening is now available on her website at wattersonspeaks.com under the products tab. Visit her website for information about upcoming speaking engagements. She may be contacted at (336) 472-3515 or by email at [email protected].
About the Author
Dianne Glasscoe Watterson, MBA, RDH
DIANNE GLASSCOE WATTERSON, MBA, RDH, is a consultant, speaker, and author. She helps good practices become better through practical analysis and teleconsulting. Visit her website at wattersonspeaks.com. For consulting or speaking inquiries, contact Watterson at [email protected] or call (336) 472-3515.
Updated June 30, 2020