Dental hygiene lasers: Why you should use lasers
HOW TO STAY FOCUSED ON DENTAL HYGIENE APPLICATIONS
BY LISA DOWST-MAYO, RDH
Lasers and dental hygiene — what a hot topic these days! You almost can’t open a dental publication without seeing some article published on dental lasers. In 2008, RDH published an article I wrote discussing dental lasers for the dental hygienist. At that time, lasers were starting to gain notice in our field. These days, laser use is becoming more of a standard of care than just some cool new tool. The number of dentists and dental hygienists utilizing laser technology in their private practices has doubled since 2008. Doubled in only four years – that is an incredible statistic! Imagine what will happen in the next four years! If you are someone who has not jumped on this bandwagon of technology yet, then this article is for you. If you are someone who has starting integrating lasers into your clinical armamentarium but are still struggling to feel comfortable with all its many uses, then this article is also for you.
A lot has changed in the world of lasers since 2008. It’s these advancements and laser modifications that encouraged me to write this piece for RDH. Lasers are an ever-changing field, just like dentistry. New products are flooding the market every year, which can make it difficult for the busy clinician to make the right research-based decisions in technology purchases.
Personally, lasers have changed the way I practice dental hygiene. I am excited to share some of my experiences with fellow RDH readers. I work full-time as a clinical dental hygienist in a general dental practice utilizing laser technology. I am also a mom and a freelance writer and lecturer. I’ve noticed the laser courses I teach in my home state of Texas have started to grow each year, so I know firsthand that there is an increase in people wanting laser information. I do not work for a laser company and am not compensated by any corporate entity for discussing certain lasers. This freedom allows me to have an unbiased view of all products on the dental laser market to share with my audiences.
I am a person who always wants to “pay it forward,” as the saying goes. I was given some truly unique opportunities to learn more than the average clinician about lasers since my 2008 publication. A fellow RDH by the name of Connie Lorich invited me to visit Ivoclar Vivadent’s headquarters to receive hands-on laser training when they launched their Navigator diode laser. She is the associate manager in professional communications at Ivoclar. She shared her laser knowledge with me and I got to use Ivoclar’s new Navigator laser on a pig jaw and have a tutorial on laser physics with one of their technology experts! It was a once-in-a-lifetime experience and I will be sharing a lot of the knowledge they provided me in this publication.
Incorporating lasers into my clinical practice has yielded so many positive results for my patients. I have noticed a decrease in postop discomfort following my scaling and root planing as well as better bleeding indices, improved tissue color/contour changes, and reattachment occurring at a faster rate than when I was doing traditional SRP with no laser integration. I am able to decrease overall costs for my patients by charging a less expensive flat rate for laser therapy alongside SRP than what we were charging for antibiotic therapy (Arestin, Atridox, PerioChip, for example). I have met hygienists in other states who use their lasers for cutting soft tissue, and they report similar positive clinical experiences as well. Unfortunately, in Texas, we are not permitted to cut on hard or soft tissue, so my laser use is limited to sulcular debridement and bacterial reduction only. But even with those limitations, I feel I could not live without my laser. Research has shown mixed results when it comes to laser use as an adjunct to SRP. To date, there is no definitive research that proves, without a shadow of a doubt, laser use as an adjunct to SRP is superior to SRP alone. We all know that individual clinical results cannot always be supported by long-term, longitudinal, systematic research. Just because the research is mixed in the laser world does not mean lasers are not beneficial for our patients.
I want to leave you with one last piece of advice before we dive into laser science. At many of the CE courses I teach, I meet fellow RDHs who feel intimidated by new technology or are scared of spending a lot of money on a piece of equipment they are not 100% sure will do what they want or what their sales rep promises. Here is my pearl of wisdom when someone is faced with fear or doubt: As long as you stay focused on doing the greater good and avoid harming your patients, then you are staying within the oath you took when you became a dental hygienist. If there is technology that may help your patients, then why not try it? Laser use is not rocket science — it’s based on elementary physics. A laser is, by far, the easiest piece of equipment I have worked with in my career as a clinician — far easier than learning to remove calculus in a sulcus that is bleeding, covered by gum tissue, on roots I cannot see that are sticky and difficult to access with today’s equipment! All RDHs say amen!
LASER SCIENCE
There is always one constant in regard to lasers, and that is the science and physics behind the technology. I am going to give you a crash course in laser physics so you can get a good foundation for knowing which laser may work best in your practice. Without this basic knowledge, specific laser use and principles will be impossible to understand and you will just be shooting in the dark when deciding which laser to spend thousands of dollars on. The physics behind lasers can get tedious to read and difficult to understand, so I am going to simplify all that science into a few paragraphs. This way you will be able to make educated decisions about your laser purchase.
A laser is defined as a nondivergent, man-made, monochromatic, electromagnetic energy of one wavelength. It is a single color of light (monochromatic). Laser light is produced when an atom becomes excited, thus emitting a photon which is the elementary particle responsible for electromagnetic phenomena. The photon, as we learned in radiology class, is the carrier of electromagnetic radiation of all wavelengths. This photon then produces the coherent, focused, concentrated ray of light.
A laser’s effect in the mouth is dependent on three things: a laser’s wavelength, where the laser light falls on the light spectrum, and the target tissue with which the laser interacts.
- Wavelength — This is the only parameter the practitioner cannot adjust on their lasers. Lasers come in many different wavelengths, and those wavelengths are generally measured in nanometers (nm). Wavelengths are absorbed by the tissue at varying degrees, which will correlate to the laser’s depth of penetration, and therefore determines its overall accuracy and precision in the mouth.12 Generally speaking, for most soft tissue procedures, the wavelengths used by dental hygienists range from 800 to 2,940 nm. For example, diode lasers, which are the most commonly used lasers by RDHs, come in either 810 nm, 910 nm, or 980 nm wavelengths.
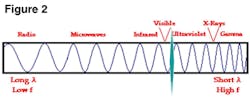
- Light spectrum — In addition to wavelength, where a laser falls on the light spectrum will greatly influence its properties. Most dental lasers fall into the infrared zone, which is just to the left of visible light. Some are deep into the infrared zone and others are closer to the junction of visible light (see Figure 1).
Here’s the short and sweet of what to take away from the light spectrum. Anything left of visible light, e.g., dental lasers, will produce longer wavelengths and lower frequencies. Anything right of visible light will produce shorter wavelengths and higher frequencies, (X-rays, for example). Anything left of visible light is nonionizing energy, and conversely, anything to the right is ionizing (see Figure 2). We use both energies in dentistry. Think of it this way: When we take X-rays, we are using ionizing energy, and when we use lasers, the light is nonionizing. Ionizing energy penetrates deeply into biological tissue, which is what we want when we take X-rays. Nonionizing energy just causes excitation and heating of tissues. I will discuss this heating of tissues in more detail in a moment. Just know this for right now: Heat is not a bad thing. Excessive, uncontrolled heat is a bad thing, and was responsible years ago for damaging oral tissues.
- Target tissue: For simplicity’s sake, let’s talk about dental tissues as two different types: hard and soft. All tissues contain certain chromophores. Hard tissue chromophores consist mainly of water, hydroxyapatite, and collagen. Soft tissue chromophores consist mainly of water and hemoglobin (Hb). Laser light is absorbed differently by these particular chromophores. A hard tissue laser is used for cutting on bone, and a soft tissue laser for cutting on gum tissue. A soft tissue laser is a poor choice for trying to remove decay from a tooth. The light energy from a soft tissue laser is poorly absorbed by hydroxyapatite and collagen. Conversely, the light energy of soft tissue lasers, which generally have lower wavelengths (800-1064 nm), is well absorbed by water and Hb (see Figure 3). If a clinician attempts to use a laser for a procedure to which it is not well suited, there will be damage to the surrounding structures.
When discussing lasers, heat is a not a bad word. Yes, all lasers produce heat — that is their primary mechanism of action. If a clinician is using a laser appropriately, with the correct setting and on the intended target tissue, then the heat produced will be helpful and not harmful. I could find a way to hurt myself with a paper clip if I did not know how to use it correctly. I could injure my patients with a Cavitron if I am not using it with the correct settings, tip angulation, and pressure. Lasers are no different. If you are not using the correct settings for your procedures or you are attempting to use a laser on inappropriate tissue, then yes, you will cause damage. With lasers, the most notable damage will be heat. Early on in laser science and experimentation, heat damage was an issue. Researchers were finding damage to the tooth pulp, dentin, cementum, or sometimes surrounding tissues in certain trials. With the knowledge and research that has been ongoing since the 1960s, most notably the advancements in laser technology that took place during the 1980s, the damage to tooth, pulp, or tissue is all but eliminated.
LASER USE IN SRP PROCEDURES
Clinical laser technique is the easiest for dental hygienists to master. The hand motion you use while in the pocket and how you angle and position the laser fiber tip is very similar to using a Cavitron. When you insert a Cavitron tip subgingivally, you use horizontal and vertical strokes with light pressure. You adapt the tip to the root structure to remove the calculus. Lasers are exactly the same, with two exceptions. Instead of angling the laser tip toward the tooth, you angle it away from the tooth, toward the tissue. Secondly, instead of removing calculus, you are removing diseased, necrotic tissue and dark-pigmented bacteria, such as periodontal pathogens. Most current research supports the use of lasers as an adjunct to SRP, not in lieu of it.2 There are some laser companies claiming clinicians no longer have to scale away calculus because their laser removes it all. To date, literature does not support this claim and the FDA does not endorse it. Scaling and root planing is still recommended, even when you are lasing soft or hard tissue.
The procedure for using a laser as an adjunct to SRP is as follows:1,4
1. Prerinse with antimicrobial mouth rinse
2. Provide anesthesia as needed
3. Ultrasonic instrumentation
4. Hand instrumentation
5. Laser bacterial reduction. The clinician measures the periodontal pocket, inserts the laser fiber directed toward the tissue and down to pocket depth minus 1 mm. So, in a 6 mm pocket, the laser fiber is inserted to 5 mm. This allows for laser energy to penetrate the tissue and reduce bacterial load without the fiber actually touching the base of the pocket.
6. Postop instructions to patient11
INDIVIDUAL LASERS
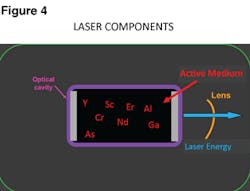
To date, no laser system has yet received the American Dental Association’s highest endorsement, the ADA Seal of Acceptance. However, many dental lasers are FDA-approved for various procedures. Lasers are generically named based on the chemical, elements, molecules, and compounds found within what we call the active medium (AM). The AM is the very core of any laser and is where the energy is directed (see Figure 4). When the elements of the AM become excited or stimulated,
certain wavelengths are produced. For example, if the AM is comprised of a gas, we call it a CO2 laser — and when that gas is stimulated by a photon, it produces a wavelength of 10,600 nm. If the laser is comprised of semiconductor wafers, we name it based on the metals found in the wafer. There can be multiple layers of metals such as gallium, aluminum, indium, or arsenic in the AM, or solid rods of garnet crystal grown with various combos of yttrium, aluminum, scandium, or gallium to which an element such as chromium, neodymium, or erbium is added.5 When crystals are added, we say the laser has been doped. Below is a list of dental lasers with their acronyms spelled out:
Hard Tissue Lasers
- Er:YAG Erbium-doped Yttrium Aluminum Garnet
- Er,Cr:YSGG Erbium, Chromium doped Yttrium Scandium Gallium Garnet
Soft Tissue Lasers
- Diode: AlGaAs Aluminum Gallium Arsenide 810 nm
- Diode: InGaAs Indium Gallium Arsenide 940-980 nm
- Nd:YAG Neodymium-doped Yttrium Aluminum Garnet
- Nd:YAP Neodymium-doped Yttrium Aluminum Perovskite
- CO2 Carbon dioxide
The most commonly used laser by dental hygienists is the diode laser. It is more cost effective than most other lasers on the market. It does the job you need it to do and is user friendly. There are multiple companies manufacturing diode lasers, and within those companies there are often multiple diodes to choose from. Some models have been around for years and now the company is offering new and improved models. Newer models come with easier-to-use features but the science behind them is the same. Many times the newer models come with touch screen technology such as the Navigator I mentioned earlier from Ivoclar Vivadent. Diode lasers come in a wide range of wavelengths. The most common are 810 nm, 940 nm, and 980 nm. If you refer to the diagram again that shows chromophore absorption rates, you see that the absorption rates of diodes differ, but in the broad spectrum of laser light and energy, they are not drastically different. I have used many of these diodes and found similar clinical results with varying wavelengths. Research has never been able to prove that one particular wavelength of laser is superior to another.2 I believe that clinicians need to find the lasers they are most comfortable with. If you are comfortable and confident in your armamentarium, then you will be successful with its use and results.
Another popular line of soft tissue lasers on the market are the Nd:YAG and Nd:YAP lasers. Their wavelengths are 1,064-1,340 nm. If you refer back to the light spectrum diagram or the absorption of chromophores diagram, you will see diodes and neodium lasers have similar wavelengths and absorption rates. Neodymium lasers, as a result, have similar uses to diodes.16
However, the PerioLase, an FR Nd:YAG laser manufactured by Millennium, performs a patented procedure called LANAP (Laser Assisted New Attachment Procedure). LANAP is showing clinical results of being able to regrow cementum, bone, and PDL in some cases. It is the only laser on the market to receive FDA approval, claiming “cementum-mediated new periodontal ligament attachment to the root surface in the absence of long junctional epithelium.”8,9,10,11 The clinical trials of this laser are interesting, and as a dental hygienist, any laser that can claim regrowth of anything a patient has lost due to periodontal disease will get my attention.
In the end, what will ultimately determine which laser you purchase for your office needs to be based on what you plan to do with it. Here are some helpful tips to keep in mind when considering laser purchasing:
- Find out how much disposable items cost for your laser. For example, does you laser come with individual fiber tips or a cord of fiber? How much does it cost for more fiber or tips?
- Is training and certification included in the price you pay for your laser?
- Will the company come in and train all employees on the laser?
- What is the cost and procedure for maintenance of your laser, should it ever have a problem?
- What is the warranty and what does it cover?
Dentistry is at the forefront of laser use and we are so lucky to be practicing in a time where this type of advanced technology is affordable. Laser use is fun and exciting and I encourage you to at least consider its possibilities for your patients. Good luck with your future laser purchase, education, and integration! RDH
LISA DOWST-MAYO, RDH, graduated with highest honors from the Caruth School of Dental Hygiene at Baylor College of Dentistry in 2002. She is an active member of the American and Texas Dental Hygiene Associations and has held various leadership positions in her local components since she graduated. She has published articles in both Access and RDH magazines and lectures on dental lasers, contemporary periodontal therapies, and the dental treatment for patients with AD/HD. She currently resides in San Antonio with her husband and two young babies who keep her very busy. Lisa practices clinical dental hygiene at Dominion Dental Spa, the office of Dr. Tiffini Stratton, DDS.
COMMON DENTAL HYGIENE PROCEDURES WITH LASERS
Lasers can be used in every specialty of dentistry and for a wide range of procedures. Since this article is focusing on laser use specific to dental hygiene, I am going to focus on soft tissue procedures. Dental hygienists all over the world use lasers for various procedures, depending on their state’s/country’s laws.1,11,15
- Pit and fissure sealants — The laser light disinfects the grooves to prevent contamination, which aids in sealant placement.
- Adjunct to scaling and root planing procedures — Laser light helps decontaminate pockets, decreasing the numbers of periodontal pathogens and removing diseased or granulation tissue. The laser light is effective in eliminating dark-pigmented bacteria, which is the primary bacteria we are trying to eliminate in periodontal disease.
- Aphthous ulcer treatment — This is achieved by a process known as biostimulation. You do not make direct contact with your target tissue when you biostimulate. The laser fiber is held a couple of millimeters away from the ulcer on the tissue. You direct the laser energy at the ulcer and the patient will start to feel immediate pain relief. The ulcer will heal almost overnight and some research claims if you biostimulate an area one time, another ulcer will never appear in that area again. It is thought the laser energy increases collagen growth, and osteoblastic and fibroblastic activity. This leads to rapid wound healing and anti-inflammatory effects in the tissue.
- Whitening — Laser photons initiate a photochemical activator and increase the enamel response to hydrogen peroxide.2
- Decay prevention — Lasers are thought to increase the enamel uptake of fluoride ions.3,20 This is not FDA approved as of yet for caries prevention.14 It is believed the laser will help fuse the inorganic components of enamel and vaporize the organic components, thus producing a less porous surface that is more resistant to demineralization.
References
1. Angelov N, Pesevska S, Nakova M, Gjorgoskil I, Ivanovski K, Angelova D, Hoffman O, Andreana S. “Periodontal Treatment with a Low-Level Diode Laser: Clinical Findings.” General Dentistry. September/October 2009: 510-513.
2. Cobb C. “Lasers in Periodontics: A Review of the Literature.” J.Periodontol. April 2006; 77(4): 545-564.
3. Chen H. “The Effects of Lasers and Fluoride on the Acid Resistance of Decalcified Human Enamel.” Photomed Laser Surg. June 2009; 27(3): 477-552.
4. Coleton S. “The Use of Lasers in Periodontal Therapy.” General Dentistry. Nov/Dec 2008: 612-616.
5. Coluzzi D. “Fundamentals of Lasers in Dentistry: Basic Science, Tissue Interaction, and Instrumentation.” Journal of Laser Dentistry, Compendium of Laser Dentistry. 2008.
6. Dean B. “Using the Er,Cr:YAGG Laser.” Concepts in Laser Periodontal Therapy. 2005.
7. Gregg R, McCarthy D. “Eight Year Retrospective Review of Laser Periodontal Therapy in Private Practice.” Dentistry Today. Feb. 2003; 22(2): 1-4.
8. Gregg R, McCarthy D. “Laser ENAP for Periodontal Bone Regeneration.” Dentistry Today. May 1998; 17(5):1-3.
9. Gregg R, McCarthy D. “Laser Periodontal Therapy for Bone Regeneration.” Dentistry Today. May 2002; 21(5):1-4.
10. Harris D, Gregg R, McCarthy D, Colby L, Titl L. “Laser-Assisted New Attachment Procedure in Private Practice.” General Dentistry. Sept-Oct 2004; 52(5).
11. Harris D, Gregg R, McCarthy D, Colby L, Titl L. “Sulcular Debridement with Pulsed Nd:YAG.” Lasers in Dentistry VIII, Proceedings of SPIUE Vol. 4610(2002). Available at http://www.millenniumdental.com/research/jan-02.html.
12. Institute for Laser Dentistry. “Laser Wavelength.” Institute for Laser Dentistry. 2000-2002. Available at http://www.laserdentistry.ca/faq/laser_wave.html.
13. Keanna G. “Biological Dentistry. New Health Insight, A New Frontier in Healthcare.” Jan-Feb 2006. Available at ww.newhealthinsight.com/index.php/Biological-Dentistry/Non-Surgical-Laser-Gum-Treatment.html.
14. Lewis R. “Lasers in Dentistry.” FDA Consumer Magazine. Jan-Feb 1995. Available at www.fda.gov/bbs/topics/CONSUMER/CON00296d.html.
15. Matthews DC. “Seeing the Light – The Truth about Soft Tissue Lasers and Nonsurgical Periodontal Therapy.” J.Can.Dental Assoc. 2010; 76:a30.
16. Neill M, Bader H. “Clinical Efficacy of the Nd:YAG Laser for Combination Periodontitis Therapy.” Practical Periodontics and Aesthetic Dentistry. August 1997; 9(6):1-9.
17. Polansky R, Haas M, Heschl A, Wimmer G. “Clinical Effectiveness of Photodynamic Therapy in the Treatment of Periodontitis.” J. Clin Periodontol. 2009; 36: 575-580.
18. Ramos de Oliveria R, Schwartz-Filho H, Novas A, Garlet G, de Souza R, Taba M, de Souza S, Ribero F. “Antimicrobial Photodynamic Therapy in the Non-Surgical Treatment of Aggressive Peridontitis: Cytokine Profile in Gingival Crevicular Fluid, Preliminary Results.” J Periodontol. 80(1): 98-105.
19. Sanderson J. “Dental Laser Basics.” Dental Health Network. 1997-2007. Available at www.dental-health.com/dental_laserbasics.html.
20. Sobral MA, Lachawski KM, DeRossi W, Braga SR, Ramalho KM. “Effect of Nd:YAG Laser and APF on Bovine and Human Enamel Submitted to Erosion/Abrasion or Erosion Only; an in vitro preliminary study.” Photomed Laser Surg. Oct 2009; 27(5): 709-713.
21. Yukna R, Carr R, Evans G. “Histologic Evaluation of an Nd:YAG Laser-Assisted New Attachment Procedure in Humans.” Internal Journal of Periodontics & Restorative Dentistry. Nov. 2007; Vol.27: 577-587.
Past RDH Issues