Protecting the practice from malpractice
What you write - or don't write - in the patient's chart can be the difference in winning or losing a malpractice suit. Follow these '10 commandments.'
by Dianne D. Glasscoe, RDH, BS
Malpractice. The very word strikes fear in the hearts and minds of all health-care providers. In fact, every dentist can anticipate at least one lawsuit in his or her practice lifetime.
The legal concept of "respondeat superior" (which is Latin for "Let the master answer") states that the doctor is legally responsible for the errors and omissions of staff members. Therefore, if a dental hygienist (or assistant) commits an act of malpractice, the dentist/employer is held responsible. How ever, any member of the dental staff may be held accountable for negligence or harm done to a patient. As dental hygienists, we have a professional obligation to help our employers avoid liability, especially in the area of dental charting.
The dental chart
The dental chart is a legal document, and it is the first line of defense in a malpractice suit. When a patient decides to file a lawsuit against a dentist, the dental chart becomes the single, most important piece of information relative to the suit.
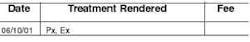
One common error in charting is failure to record thoroughly the events of the appointment. For example, in our haste to stay on schedule, we simply forget to record that we did an oral-cancer screening. Later, if the patient develops oral cancer, he may accuse the doctor of failure to diagnose. The doctor or hygienist may say to a jury that an oral-cancer screening is done on every patient. However, in the eyes of the jury, if it was not written in the chart, it was not done. Here is an example of an inadequate chart entry:
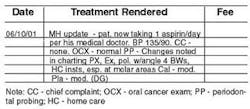
Although this hygienist may have been quite thorough in delivering care, the chart does not reflect that. Here is a better chart entry:
In this chart entry, everything that was done in the appointment is recorded. In addition, the recorder initials the entry. Since many different people write in the patient chart, it is important that each entry be initialed. Good, thorough chart entries provide valuable information to the next clinician that treats this patient. (If there are multiple doctors in the practice, the doctor that checks the patient also should be identified.) The message here is to chart defensively.
Another common dental-charting error is skipping lines between entries. Sometimes, clinicians write with large strokes that take several lines. However, chart entries should be written with small enough strokes that they can be contained within the space provided, and no lines should be skipped. The reason for this is to prevent the opportunity for inserting information after a lawsuit is initiated.
Follow the commandments!
Some valuable information about dental charting is contained in the book, Malpractice - What They Don't Teach You in Dental School, by Jeffrey J. Tonner, J.D. (PennWell Books, 1996). What follows is a listing, with examples, of Tonner's "10 Commandments of Dental/Legal Char ting."
1. Never, ever alter or amend charts. The single most common cause of punitive damages in a dental malpractice suit is altering the chart. Never use correction fluid to correct an entry. Instead, mark out the incorrect entry with a single line (so that it can still be read) and initial it. Also, do not go back and add to entries already made to make them appear contemporaneous with the events in question. Juries may perceive such added entries to be fraudulent and deceptive. Additionally, do not mark in margins or write below the last line. Doing so can cause juries to wonder why the text was not formatted within the lines.
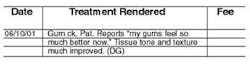
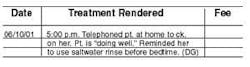
2. Use quotation marks to chart patient compliments. This is especially important when making follow-up telephone calls after a difficult or invasive procedure. Example:
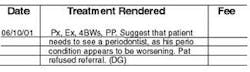
3. Chart patient noncompliance. This is extremely important for hygienists. Sometimes, we refer patients to specialists, but the patient refuses to go. Example:
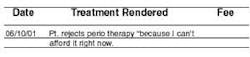
In addition, we need to chart a patient's refusal to follow recommendations. Periodontal problems are a recurring area of patient neglect. Often, good dental procedures are compromised by:
• poor oral hygiene
• continued smoking
• failure to regulate diabetes
• failure to follow specific instructions
Most practitioners will chart the first few instances of neglect, but then tire of the endless repetition. A quick referral to previous charting is an efficient alternative - i.e., "Pt. again warned as per (date of previous chart entry)."
4. Spend an extra five minutes charting bad or unanticipated results. Don't rush through your charting. If time is a problem, review the chart at the end of the day when you have no distractions. This gives you time to gather your thoughts and record certain appointments thoroughly and accurately, especially on those "unusual" patients.
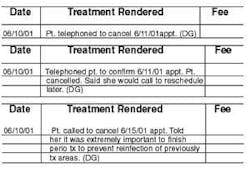
5. Make chart entries consistent with the appointment book. With most dental software and computer scheduling, the patient's name must be on the schedule to make a chart entry. However, with manual appointment books, entries can be erased and changed. If the treatment dates in the chart do not match the appointment- book entries, doubt may be cast on the reliability of the doctor's records. If the patient is being seen as an emergency patient, that should be recorded in the chart. In addition, all cancellations should be written in the patient's chart.
6. Use dental lab personnel for difficult crown and bridge.
7. Place follow-up telephone calls for difficult or invasive procedures. My rule-of-thumb has always been to call any patient that required anesthesia for the visit that day. If the patient was seen after 3 p.m., take the patient's telephone number home with you and call after dinner.
8. Chart alternative/recommended treatment plans. The 'ADRA' abbreviation stands for advantages, disadvantages, risks, and alternatives. This abbreviation minimizes charting, yet fulfills legal requirements. This is especially important for hygienists who spend copious amounts of time discussing treatment options with patients. In addition, when patients reject certain treatment options, that should be charted.
9. Dentists should review charting by hygienists and assistants. Any hygienist or assistant entries should be made before the dentist's entries. In addition, everyone should use the same abbreviations and charting methods.
10. Update the patient's medical status for each visit. Patients do not usually volunteer information about taking a new medication or a change in their medical history since their last visit. Make it a habit to ask, "Have there been any changes in your medical history since we last saw you?" Use the abbreviation "NCMH" (no changes in medical history) to designate no changes.
As the most highly trained auxiliaries in the practice, it is our professional responsibility to our employers and patients to practice to the professional standards under which we were educated. Anything less is simply not acceptable.
Dianne D. Glasscoe, RDH, BS, is a professional speaker, writer, and consultant to dental practices across the United States. She is CEO of Professional Dental Management, based in Lexington, N.C. To contact her, call (336) 472-3515 or send e-mail to [email protected].
Case History: periodontal neglect
The plaintiff was a 55-year-old school teacher who had been under the almost continuous care of a general dentist in Florida from 1963 until 1995. During her 32-year course of treatment by the defendant, the plaintiff diligently and almost religiously returned to the office for periodic prophylaxes. These cleanings were performed by the defendant and not by a dental hygienist. In 1970, the defendant took a full-mouth series of dental X-rays, as well as taking bitewing X-rays at many of the patient's cleaning visits.
The patient was never told about the onset or progression of periodontal disease until December 1995, when she developed a periodontal abscess and the defendant made a new full-mouth series of X-rays. Even then, the dentist didn't tell her about her periodontal disease, but, instead, referred her to a periodontist who "had to tell her the bad news." The plaintiff lost several teeth and required four quadrants of periodontal surgery.
This case was settled during the presuit investigation period for the defendant's policy limits of $100,000.
(Used with permission from The Dentalaw Group, Boyd Shepherd, DDS, J.D., 16514 Canyon Chase Dr., Suite 200, Houston, Texas 77095)
Case history: Failure to diagnose
Plaintiff was a 45-year-old, telephone-company network technician who had been under the continuous care of his general dentist from 1975 until 1995. Plaintiff was compliant and diligent about his oral hygiene and followed all dental advice given by the dentist-defendant: i.e., when plaintiff was told he needed restorations, he had them done; when he was told he needed a root canal, he had it done; when he was told he needed a bridge, he had it done.
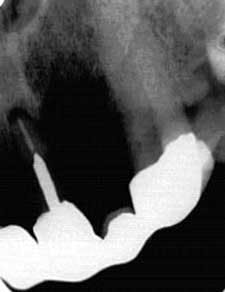
The plaintiff developed periodontal disease, which progressed until some of his teeth had no bony support. The plaintiff was never told about the onset or progression of periodontal disease until he visited a different dentist for a "second opinion," at which time he was told to "run, don't walk, to a periodontist." The plaintiff lost teeth and required four quadrants of periodontal surgery and expensive crown-and-bridge restorations.
The case settled during a mandatory pretrial mediation conference for $125,000.
The middle picture was taken one month after the patient's last visit to the defendant, at which time he was told he was "in fine shape."
(Used with permission from The Dentalaw Group, Boyd Shepherd, DDS, J.D., 16514 Canyon Chase Dr., Suite 200, Houston, Texas 77095)
Case History: Failure to diagnose
The patient was a 39-year-old male smoker with poor oral hygiene. While cleaning his teeth, the hygienist discovered a 2 mm lesion on the right lateral border of the tongue. It was duly charted. Later in the same appointment, the general dentist reviewed the charting and examined the lesion, but said nothing to the patient. He diagnosed it as inconsequential and benign.
The parties then agreed that his severe periodontal disease should be addressed by a specialist. The patient was referred to a periodontist. In 15 visits over the next seven months, root-planing and scaling were performed in each quadrant of the mouth. At no time did the periodontist detect any lesion.
During the periodontal treatment, the patient also visited the general dentist three times for routine maintenance and prophy checkups. Nothing unusual was detected.
Nine months later, the general dentist noted a 1.5 centimeter lesion, again on the right lateral border of the tongue. The patient was instructed to monitor the situation closely and return if it did not resolve immediately. Two weeks later, the patient reappeared with the same condition. An oral surgeon biopsied the lesion the following day. The diagnosis was squamous cell carcinoma.
Within weeks, surgeons performed a hemi glossectomy, removing the right half of the tongue. The usual course of radiation therapy followed. The prognosis was considered good.
The patient and his wife filed a malpractice action, naming both the general dentist and the periodontist as defendants. The damages at that time were his medical expenses, several months of lost wages, loss of half the tongue, pain and suffering, and loss of marital relations. The plaintiffs claimed that the first and final lesion was one and the same and the dentists had failed to detect it over a combined 20 visits. Specifically, it was advanced that the two dentists either had neglected to perform an oral-cancer screening during any particular visit or had performed the screening using improper techniques.
As time progressed, the patient's condition deteriorated. Shortly before trial, the cancer metastasized to his liver and lungs. He died during the six-week trial, and his widow continued the case. After more than two days of deliberations, the jury found against both dentists and awarded nearly $1.1 million to the surviving widow, two minor boys, and the plaintiff's parents. The dentists appealed the verdict. Three years later, the state Supreme Court reversed the award and ordered a new trial. The matter was then settled. Nevertheless, the parties suffered through the long and, often acrimonious, trial, appeal, and settlement process. More than seven years elapsed between the time the complaint was filed and the final settlement was reached.
(Used with permission, Malpractice - What They Don't Teach You in Dental School, Jeffrey Tonner, J.D., 1996, PennWell Books, Tulsa, Okla.)