Ethical decision making
The role of ethics in dental hygiene education
By Jennifer S. Sherry, RDH, MSEd, and Emily E. Arbeiter, RDH, BSDH
Dental hygiene students are faced with ethical decisions every day. Also, ethical situations can involve academic integrity and the ability to “do what is right.” It is the student’s ethical responsibility to report the clinical findings to the patient and to provide accurate assessment of their dental condition. The ramifications of cheating include not only harm to the student, but also breakdowns in academic integrity within health professions education may result in substandard or inappropriate patient care because the dishonest student does not acquire the knowledge base or clinical experience necessary to deliver high-quality care.1
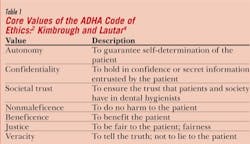
According to the American Dental Hygienists’ Association (ADHA), the bylaws state the purpose of this association shall be to improve the oral health of the public and to advance the dental hygiene profession and to uphold the highest standard of care. The Dental Hygiene Code of Ethics is meant to influence us throughout our careers.2,3 The core values of the ADHA Code of Ethics are critical to understand for anyone in the dental hygiene profession (see Table 1). A code of ethics recognizes the following three relationships: professional and client, professional and professional, and professional and society. The public has strong expectations for appropriate professional behavior.5
The Principles of Ethics and Code of Professional Conduct of the American Dental Association states the dental profession holds a special position of trust within society. Society grants the profession certain privileges that are not available to members of the public at large.6 The Commission on Dental Accreditation (CODA) and the American Dental Association (ADA) have also set standards for educators and dental hygiene students at universities and colleges to use to pattern their curriculum and to be able to evaluate their patients in a professional and complete manner. These standards will provide a framework for clinical practice that focuses on the provision of patient-centered comprehensive care.7 Also, the American Dental Education Association (ADEA) policy statements call for formal instruction in ethics and professional behavior with the goal of making the students aware of acceptable professional conduct in instructional and practice settings.8,9
Legal Terminology and Ethical Training
Since the dental record contains continuous documentation of patient oral conditions and treatment, this is the primary tool used in the evaluation of patient care.10 The old adage is true: If you did not write it down, it did not happen. A mutual relationship exists between the adequacy of record-keeping and the adequacy of patient care.10,11
Second, legal concerns are a reality of dental practice, and adequate records provide documentation for legally complicated cases. Appropriate risk management strategies, including accurate and complete records, are essential in the practitioner’s defense. Third, responsibility for demonstrating the provision of quality care is an impossible task without good record-keeping.10 More than anything else, the quality of your records can make or break a successful legal defense.12 This can ultimately affect the practitioner’s future, both professionally and personally.
Accordingly, as required by the Commission on Dental Accreditation of the American Dental Association, all dental and dental hygiene educational programs have developed competencies and related evaluation mechanisms for the domain of professionalism and ethics.10 Authentic evaluation is designed to measure students’ performance in the context of situations they will encounter in practice as licensed care providers.13 While the association between ethics and patient care is an obvious and important one, ethical sensitivity and behavior are also necessary before students begin their clinical experiences.14 Also, training faculty to be consistent in the feedback they give regarding students’ performance is important to reinforce core values and ethical principles taught throughout the curriculum. This could reduce the students’ and evaluators’ uneasiness with subjectivity and improve students’ acceptance of this aspect of authentic evaluation.13
Clinical faculty needs to exhibit ethical behaviors and encourage or even invite students to imitate these professional actions. Faculty members are often practitioners themselves and should serve as role models for students. The clinical faculty can have a potentially greater influence on dental and dental hygiene students’ learning in clinic than in classroom settings.15,16 Because of this relationship, it is imperative that clinical faculty members recognize ethical issues and wrongdoings and take appropriate action.
Overall, clinical teaching qualities of significance to the students include rapport (such as availability, approachability, and student-patient relationships), role modeling, and feedback.15 Grading or evaluating performance during these “teachable moments” requires rigorous justification by the faculty to demonstrate that ethics and professionalism are not irrelevant to practice, but rather vital practical and professional skills.13
Clinical faculty need to understand that students have pressure from clinical and didactic courses, and they may feel overloaded in some situations, which causes them to feel like cheating is their only option. Competitive pressures can cause some students to behave unethically. Service to others needs to be emphasized and rewarded, and ethical behavior needs to be recognized as much as, if not more than grade point average, or GPA. Just as importantly, students need to be offered alternatives to cheating that address the threat of failure.17 Also, clinical faculty needs to convey that it is acceptable to gain help or ask questions. Some students may feel this makes them look incompetent.
Office Procedures
Early risk management courses taught dentists the importance of recording treatment. This evolved into the “records, records, records” mantra. By writing everything in the record, there would be a basis for a good defense if the dentist were sued. Then came the “inform before you perform” mantra. A solid defense could be developed for alleged malpractice by informing patients of the benefits, risks, alternatives, and costs related to a procedure, and receiving their consent to perform the procedure.18
This also holds true for the dental hygienist. Not only should we keep good records and inform patients, but we also should include them in the diagnosis and decision-making process with regard to the proposed treatment plan. By educating patients through proper mutual discussion, patients learn what their actual dental needs are and will be able to take part in their treatment plan’s decision-making process.18
Dental offices should also update the medical history at subsequent visits to ensure there are no changes that would update the planned procedure or treatment plan. A good set of radiographs and a thorough caries examination, which should include a treatment plan, are good ways to start record-keeping for risk management and are a basis for patient communication.18
Today’s risk management must take into account not only defensive record-keeping, but also educated-patient treatment planning based on evidence of need for proposed dental treatment.18 The practitioner should not rely on records that were gathered previously because they could be incorrect. This would be detrimental to the patient’s safety and well-being and this could have a negative impact on their dental and medical health. Patients should continue to be informed about their choices for dental care as well as options so they can make informed decisions regarding treatment. Evidence-based dentistry is becoming the new buzzword and patients deserve that information. Remember to keep the patient’s best interests in mind when sequencing the treatment according to his or her dental health needs and financial concerns.18
Students and Ethical Decision Making Practices
As we know, students are diligent and try to work on many clinical requirements and attempt to complete them in a timely manner. Their intentions, at the time, may not be to cheat or deceive, but if they choose to document another student’s work or fabricate inaccurate clinical data collection or do not collect data at all and falsify patient records, this choice could prove to be a dangerous and deadly one. It could also hamper the ability to treat the patient effectively and efficiently if a medical emergency arises.
Ethical dilemmas as they relate to patient care are an unavoidable component of health care as delivered by all types of practitioners. A dramatic change in the health care paradigm has been the emergence of allied health care providers.19 Instead of dentists making all of the ethical decisions for the practice, now it has evolved into the dental hygienists having some responsibility for assuming some additional decision making roles. This makes it even more critical to ensure these professionals have the adequate educational background to make sound and ethical decisions for their offices as well as their patients.
For dental hygiene programs, this is an issue that needs to be addressed at the program level and it begins with the program director as well as the faculty.
Documentation practices and proper record-keeping are vital to the success of dental hygiene students. If they maintain integrity and morals as far as this is concerned, they will be successful and trusted professionals. There should be more strict guidelines and professionalism courses in dental hygiene schools so students know the importance of these tasks. Also, the dental hygiene faculty should embrace the students and be excellent role models to instill good practices in patient care. Pave the way and the students will follow your example!
Students should be held accountable if they choose to falsify records or knowingly document data on a patient incorrectly. Strict policies should be instilled and enforced in dental hygiene programs. If the students learn this early in the curriculum, they will be more apt to carry these values into the clinical practice setting. It is also important to make sure students know the normal and abnormal appearance of oral tissues and are able to properly document their findings. The students may not feel confident in detecting and recording such information, so this is the responsibility of the clinical faculty as well as the didactic faculty. Keep in mind, some students are more hands-on and some are visual learners. It is imperative to incorporate both learning styles in dental hygiene courses.
Students have a responsibility to care for their patients and promote the strategies of oral health and disease prevention. If the student is able to foster these skills while in school, hopefully there will be enough knowledge base and consistency to carry them on to clinical practice. We must be able to hold our heads high at the end of the day and be able to say we did our very best to maintain ethical and sound professional conduct. Our patients deserve the best care possible and should be treated with dignity and respect. SF
Jennifer S. Sherry, RDH, MSEd, is an assistant professor at Southern Illinois University’s School of Allied Health in Carbondale, Ill. She can be contacted at [email protected]. Emily E. Arbeiter, RDH, BSDH, is a 2010 graduate of the Southern Illinois University Dental Hygiene Program.
References
1. Muhney KA, Gutmann ME, Schneiderman E, DeWald JP, McCann A, Campbell PR. The prevalence of academic dishonesty in Texas dental hygiene programs. J Dent Educ. 2008; 72(11):1247-60.
2. American Dental Hygienists’ Association. 2007-2008 Bylaws Code of Ethics [Internet]. American Dental Hygienists’ Association; [cited 2009 Mar 5]. 1 p. Available from: http://www.adha.org/downloads/ADHA-Bylaws-Code-of-Ethics.pdf.
3. Daniel SJ, Harfst SA,Wilder RS. Mosby’s Dental Hygiene: Concepts, Cases, and Competencies. 2nd ed. Dolan J, editor. St. Louis (MO): Mosby, Inc; 2008. p. 43-44.
4. Kimbrough VJ, Lautar CJ. Ethics, Jurisprudence and Practice Management in Dental Hygiene. 2nd ed. Cohen M, editor. Upper Saddle River (NJ): Pearson Prentice-Hall; 2007. p. 20.
5. Darby ML, Walsh MM. Dental Hygiene: Theory and Practice. 3rd ed. Dolan JJ, editor. St. Louis (MO): Saunders; 2010. p. 1183.
6. Maitland RI. Disturbing trends in dental education. J Esth Restor Dent. 2006; 18: 307-309.
7. American Dental Hygienists’ Association. Standards for clinical dental hygiene practice. Access. 2008; 22(5): 1.
8. Sharp HM, Kuthy RA. What do dental students learn in an ethics course? An analysis of student-reported learning outcomes. J Dent Educ. 2008; 72: 1450-1457.
9. American Dental Education Association. ADEA policy statements (as revised and approved by the 2008 ADEA House of Delegates). Part I, Section B: ethics and professionalism. J Dent Educ. 2008; 72(7): 813.
10. Osborn JB, Stoltenberg JL, Newell KJ, Osborn SC. Adequacy of dental records in clinical practice: a survey of dentists. J Dent Hyg. 2000; 74(4): 297-306.
11. Haring JI, Howerton LJ. Dental Radiography: Principles and Techniques. 3rd ed. Rudolph P, editor. St. Louis (MO): Saunders; 2006. p. 159.
12. Speidel TM, Jerrold L. Record keeping to avoid or defend lawsuits: A defense attorney’s perspective. Am J Orthod Dentofacial Orthop. 2004; 125: 754-756.
13. Christie CR, Bowen DM, Paarmann CS. Curriculum evaluation of ethical reasoning and professional responsibility. J Dent Educ. 2003; 67(1): 55-63.
14. Berk NW. Teaching ethics in dental schools: Trends, techniques, and targets. J Dent Educ. 2001; 65(8): 744-750.
15. Schonwetter DJ, Lavigne S, Mazurat R, Nazarko O. Students’ perceptions of effective classroom and clinical teaching in dental and dental hygiene education. J Dent Educ. 2006; 70(6): 624-635.
16. Tedesco LA, Garlapo DA, Albino JE, Conny DJ, Wood RH. Dimensions of effective preclinical teaching. J Dent Educ. 1982; 46: 639-645.
17. Koerber A, Botto RW, Pendleton DD, Albazzaz MB, Doshi SJ, Rinando VA. Enhancing ethical behavior: views of students, administrators, and faculty. J Dent Educ. 2005; 69(2): 213-224.
18. Graskemper JP. A new perspective on dental malpractice: practice enhancement through risk management. J Am Dent Assoc. 2002; 133: 752-57.
19. Duley SI, Fitzpatrick PG, Zornosa X, Lambert CA, Mitchell A. Dental hygiene students’ attitudes toward ethical dilemmas in practice. J Dent Educ. 2009; 73(3): 345-357.
Past RDH Issues