Cost-effectiveness of dental hygiene care
Hygienists should offer a dollar value to preventive dental care
by Howard M. Notgarnie, RDH, EdD
The Centers for Disease Control and Prevention (CDC) recognizes professional dental hygiene care as a cost-effective measure toward health.1 The National Center for Chronic Disease Prevention and Health Promotion reported that 68.5% of adults visited a dentist or dental clinic in 2008, and of those, 69.0% had their teeth cleaned.2 These figures, along with similar findings in other years, indicate that less than half of the U.S. population receives care from a dental hygienist in any given year.
The lack of regular preventive care is consistent with a high prevalence of caries. According to the survey by the National Center for Chronic Disease Prevention and Health Promotion, in all but 10 states more than half of the children in third grade have a history of caries, and in all but 11 states fewer than half of the students at that grade level have sealants.2 The CDC estimated that the total cost of U.S. dental care in 2010 was $108 billion. The CDC has been investigating the scientific support for prevention-based oral health care strategies at the community level, including infection control procedures in dental clinics, and the detection of oral cancer.
In addition, the CDC highlighted successful legislative and community efforts that have improved consumer access to fluoridated water, school-based sealant programs, Medicaid funding, and decreased restrictions to dental hygiene services.1 Published research should demonstrate how dental hygiene care benefits consumers.
Costs of treatment
Karp addressed the burden health care costs pose for elderly patients and their families. Extended families lose over $60 billion a year in income not earned at their jobs because they are taking care of relatives with chronic illnesses. Although many people do not spend exorbitantly on health care as they age, a married couple on average spends 50% of their annual income on one spouse’s last year of life. In contrast, seven years prior to death, only 15% of a couple’s income is spent on health care in one year. The burden is proportionately worse on people living in poverty; however, medications to manage illness can reduce overall health care costs and reduce the number of families that fall into poverty because of health care expenses.3
Karp also identified loss of income as the most prominent factor in loss of wealth associated with disease. Illness decreases net worth partly because of the cost of disease intervention, but largely because of the decreased earning potential that accompanies disease. Illness also deters employees from allocating earnings to retirement savings for fear of not having that money available for health care costs. Furthermore, inaccurate estimation of future health care costs leads people to avoid the risky investments essential to wealth accumulation. In addition, some employees delay retirement to avoid losing health insurance. In essence, a strong relationship exists between health and wealth.3
Restriction of professional practice is a cause of artificially high health care costs. Schansberg, in an evaluation of “ObamaCare” health care reform, suggested that flaws in the existing legislation fail to address underlying structural problems in financing of and access to care. Licensing by regulation appears to protect the public from incompetent practitioners, but it has the primary effect of reducing competition for members of those professions that control regulation. By having control of other professions’ work, physicians and dentists maintain a monopoly over the services within their purview. Lack of competition leaves consumers few choices for comparison shopping, and consequently, practices are at liberty to reduce the performance of the services they provide despite high costs.
In contrast, voluntary credentialing systems would put power in the hands of consumers, whose interest in value for services would place an economic pressure on practitioners to offer services at a high quality and low price. Schansberg therefore recommended eliminating the restrictions on practice settings, ownership, and authority to practice by skilled health professionals.4
Bourgeault pointed out that potential clients should be able to recognize the diversity of health services and practitioners available, and to choose prevention and early intervention rather than waiting for an overtly diseased state to seek treatment.5 Dental hygienists in control of their profession can decrease the cost of health care with early intervention, which has the potential to prevent high spending on correcting or managing illness. Cobban, Edgington, and Clovis emphasized the importance of research in creating a theoretical basis for dental hygiene care.6 The economic value of dental hygiene care to clients is one area in which increased research would be worthwhile.
Potential research methods
The dental hygiene profession needs to increase its knowledge base through research. Spolarich, Gadbury-Amyot, and Forrest emphasized research as an asset, even to students and practitioners who have no interest in becoming researchers. In contrast to functioning in a programmed, technical status, dental hygienists must use research to support evidence-based decisions in clinical practice. A focus on research also fosters intellectual development and socialization of dental hygiene students as knowledge-based experts. Research helps the profession grow in status among health professions, while providing career development for dental hygiene instructors.7
A critical advantage research provides to the profession is the justification consumers and policy makers have for supporting access to dental hygiene services.8 The dental hygiene profession has a duty to identify research methods that demonstrate the efficacy of dental hygiene services, and to implement those research methods.
With the growing cost of health care in the U.S., consumers, policymakers, and the industry have an interest in identifying the most cost-effective methods of diagnosis and treatment. Pearlroth, Goldman, and Garber found that substantial savings in health care costs are available through selective use of technology. Using new technologies and expensive equipment tends to raise the cost of care without improving its effectiveness. They described comparative effectiveness research as a method of determining the value of procedures in the health care industry.
The traditional method of clinical research focuses on efficacy by comparing a drug’s effectiveness in an experimental setting with the use of a placebo. In contrast, comparative effectiveness research entails comparing two therapeutic modalities in clinically realistic situations. This method not only reduces the cost by demonstrating the low value of potentially costly medications and procedures, but also improves care by demonstrating the most effective treatment for a particular condition.9
In their study, Pearlroth et al. used aggregated data to compare the average cost of nontreatment to five methods of treatment for recently diagnosed prostate cancer in people who had been diagnosed by biopsy examination a year earlier as not having cancer. In addition, Pearlroth et al. compared the current total cost to society of treating prostate cancer with that of the most cost effective method. The findings showed that although all treatments were equally effective, there was a large difference in overall costs among various treatment modalities. The least costly treatment saved consumers $7,300 compared with the second cheapest treatment, and saved $46,900 compared with the most expensive treatment. Given the proportions of each method used in the U.S., society could save between $1.7 billion and $3 billion each year on that one disease alone.9
This analysis could be an effective model for the value of dental hygiene care. Gadbury-Amyot et al. emphasized the importance of developing a theoretical foundation for dental hygiene practice. That theoretical foundation comes in the form of research,8 and an important part of what research shows is that society experiences a net reduction in cost as a result of receiving that care. In particular, a similar approach to Pearlroth et al.’s study to determine the cost-effectiveness of dental hygiene care may be to compare the overall cost to consumers for dental care, with the variable being their use of services by dental hygienists for generalized, moderate periodontitis.
The choices of many consumers and practitioners are: 1) wait until symptoms appear before seeking care, 2) prophylaxis every six months, 3) root planing followed by periodontal maintenance every three months, and 4) referral to a periodontist for surgery.
Another example of research that can differentiate benefits and costs of treatment is a meta-analysis. A meta-analysis is a systematic review of data from many studies. Brazzelli et al. performed a quantitative meta-analysis of data from research on the effectiveness of adding an ozonating agent to remineralization treatment or sealants of noncavitated carious lesions. Some studies demonstrated improved effectiveness of remineralization and sealants in non-cavitated pit and fissure caries, but other studies showed that ozone lacked effectiveness on noncavitated root surface caries. The analysis reflected insufficient data to conclude on the overall effectiveness of adding ozone to the treatment protocol.
Because Brazzelli et al. found insufficient economic data comparing treatment with and without ozone, they used the Markov model to analyze data presented by the manufacturer, along with industry expectations of disease progression to determine the cost savings. The Markov model entails reviewing a hypothetical progression of a disease state among a cohort of patients. Standards are used to calculate the proportion of patients whose diseases progress to a particular state over a given time. The researchers speculated that adding ozone to the remineralization protocol is not cost effective for pit and fissure lesions, but has the potential to be cost effective for root surface lesions.10 Naturally, empirical data provides a more reliable picture of the expected benefits of a particular treatment modality.
Dental hygienists should develop original and meta-analytic studies that demonstrate effectiveness and cost-effectiveness of care that entails prevention and early intervention of disease. From the standpoint of public policy, such knowledge fosters efficiency in public health, justifies treatment modalities offered by dental hygienists, and justifies the authority the profession seeks in regulatory reform. On an individual level, knowledge of a treatment’s effectiveness and cost provides dental hygienists with the information they need to recommend a procedure.
An important concept of cost-effectiveness that dental hygienists should understand is finance. Clients often decline dental hygiene care as too costly, especially if they lack insurance or insurance does not fully reimburse expenses. Failure to accept prevention and early intervention care frequently results in deterioration of health and increase in cost of care. When comparing the cost of minimally invasive treatments now with more expensive and invasive treatments in the future, financial calculations provide an accurate comparison. Financial calculations include accounting for all costs and savings associated with accepting or declining treatment, and accounting for the time value of money using a discount rate.
For example, a person might visit a dental hygienist after a year without preventive care. Documentation from the prior office may indicate healthy gingiva and no evident caries. By performing an assessment, the dental hygienist now identifies plaque in areas floss fails to reach because calculus blocks the client’s otherwise thorough home care techniques. In the areas retaining plaque, the dental hygienist diagnoses gingivitis, and in one area, decalcified tooth structure at risk of progressing to a cavity on a tooth already compromised by a large restoration. A reasonable treatment plan for that new client is a prophylaxis and fluoride treatment every six months, and bitewing radiographs once a year. The average cost for those services is $385 per year in the Los Angeles area.11
A person who declines that treatment might return five years later needing a crown and root planing, followed by periodontal maintenance four times each year, which is $3,980 for the first year, and $990 each year after that.11 In addition, the person will probably need to miss two hours of work for each trip to the dental office, which would be only four hours each year if only preventive treatment was needed. In contrast, the person waiting five years will need to take off 16 hours of work the first year and eight hours each year thereafter. At the average rate of $23 per hour, according to the Bureau of Labor Statistics12, a client seeking preventive care has an opportunity cost of $92 from not working those four hours. The person who needs a crown and nonsurgical periodontal treatment five years later may lose $368 the first year and $184 each year afterwards from lost work.
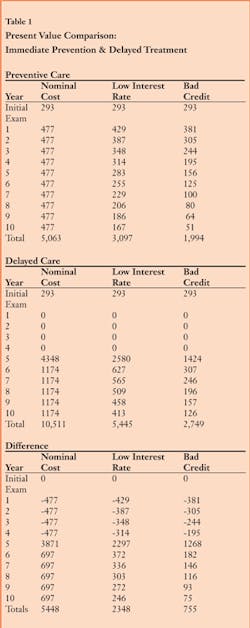
For the sake of simplicity, assume direct care and missed hours at work are the only two costs that vary between prevention-oriented clients and those who delay treatment. The nominal difference in cost over a 10-year period is $5,448. However, when considering the time value of money, the difference in present value of the cost of delaying treatment is not that bad. The client who does not start spending money for treatment until five years after the initial examination has that money in hand to invest or needs to borrow that much less money. So, a more accurate measure of cost is to calculate the net present value of the costs over those 10 years. The present value of money spent or earned in the future is calculated based on a discount rate, which can be looked at as the amount of interest a client would earn if he or she put it into the next best investment. Assume a person spending money on dental care uses a credit card to pay for services and considers the next best investment to be not borrowing money. Based on a recent survey, average credit card interest rates varied from 11% to 25% for debtors with bad credit ratings.13 The present value of money is calculated by the following formula: PV = CFn/[(1+i)n].
PV = present value of money to be spent at one or more particular times
CFn = cash flow at a particular time in the future
n = time, in years from the present, at which an expense will be incurred
i = discount rate
The interest a person would pay if he or she borrowed money on a credit card at an interest rate of 11% or at a bad rate of 25% is figured into the calculations as the discount rate to determine the present value for expenses each year. Table 1 demonstrates a comparison between the present value of starting and continuing preventive services now and the present value of treatment five years from now. If the cost of care ended after four years of the initial exam, delaying treatment would be beneficial from a cost perspective to the client. However, people can count on continuing costs for health needs throughout their lives. The additional net present value for the first 10 years after an exam when care is delayed comes to $2,348 assuming a low discount rate, and $755 assuming a high discount rate.
Dental hygienists hope to educate patients to help people reduce their expenses. These are speculative costs based on conservative assumptions of disease progression. Identifying the average progression of various diseases with and without dental hygiene care is incumbent on our profession. Knowledge of that progression would give colleagues and clientele accurate information to confirm the present value of treatment recommendations and the decision to accept or reject those recommendations.
Although dental hygienists’ interest as health professionals is in maintaining health and minimizing disease, adding a monetary value to care adds information in the arsenal with which members of the profession can educate clients on the value of services. Also, making these calculations might convince policymakers to increase dental hygienists’ scope of practice, practice settings, and authority regarding diagnoses and treatment plans. The need for accurate financial data might also encourage policymakers to require dental clinics to report which specific practitioners provide treatment, rather than attributing all procedures to the practice owner.
Howard M Notgarnie, RDH, EdD, practices dental hygiene in Colorado. He has eight years of experience in professional association leadership and five years of teaching experience.
References
1. Centers for Disease Control and Prevention. (2011). Oral health: Preventing cavities, gum disease, tooth loss, and oral cancers at a glance 2011. Washington, DC: Author. Retrieved Oct. 14, 2011, from http://www.cdc.gov/chronicdisease/resources/publications/AAG/doh.htm
2. National Center for Chronic Disease Prevention and Health Promotion. (2010). Oral Health Indicators. Washington, DC: United States Department of Health and Human Resources. Retrieved Oct. 14, 2011, from http://www.cdc.gov/nohss/
3. Karp F. (2007). The health and retirement study: Growing older in America. Bethesda, MD: National Institute on Aging. Retrieved Oct. 14, 2011, from http://www.nia.nih.gov/ResearchInformation/ExtramuralPrograms/BehavioralAndSocialResearch/HRSfull.htm
4. Schansberg DE, (2011). Envisioning a free market in health care. Cato Journal, 31(1), 27-58.
5. Bourgeault IL, (2006). The provision of care: Professions, politics, and profit. In D. Raphael, T. Bryant, & M. H. Rioux (eds.), Staying alive: Critical perspectives on health, illness, and health care (pp. 263-282). Toronto, Ontario, Canada: Canadian Scholars’ Press.
6. Cobban SJ, Edgington EM, Clovis JB, (2008). Moving research knowledge into dental hygiene practice. Journal of Dental Hygiene, 82(2), 1-10.
7. Spolarich, Gadbury-Amyot, Forrest (2009). Research issues related to education. Journal of Dental Hygiene, 83(2), 79-83.
8. Gadbury-Amyot CC, Doherty F, Stach DJ, et al. (2002). Prioritization of the national dental hygiene research agenda. Journal of Dental Hygiene, 76(2), 157-166.
9. Pearlroth DJ, Goldman DP, Garber AM, (2010). The potential impact of comparative effectiveness research on U. S. health care expenditures. Demography, 47, S173-S190.
10. Brazzelli M, McKenzie L, Fielding S, et al., (2006). Systematic review of the effectiveness and cost-effectiveness of HealOzone® for the treatment of occlusal pit/fissure caries and root caries. Health Technology Assessment, 10(16), i-xi, 1-96.
11. Braces Info. (2010). Find the average cost of dental care in Los Angeles, California. Retrieved Oct. 26, 2011, from http://www.bracesinfo.com/dentalcosts/us/ca/los-angeles.html
12. Bureau of Labor Statistics. (2011). Occupational earnings tables: United States, December 2009 – January 2011. Washington, DC: Author. Retrieved Oct. 26, 2011, from http://www.bls.gov/ncs/ncswage2010.htm#Wage_Tables
13. Tomasino K. (2011). Rate survey: Credit card interest rates hold steady. Austin, TX: Credit Cards.com. Retrieved from http://www.creditcards.com.
Past RDH Issues