Osteoporosis
When Jan Britt went to her periodontist, Dr. James Boyle, in Powder Springs, Ga., she expected the usual perio maintenance visit. Instead, she says, “My dentist looked beyond the obvious on the dental X-rays and could see dramatic changes in my jaw bone density.”
With a family history of osteoporosis, the diagnosis wasn’t a total shock, but it was advanced enough to require a visit to her doctor, a bone density test, and eventually, medication. Like many other systemic diseases, it can’t be accurately diagnosed from dental X-rays alone, and not every person with osteoporosis will have oral signs. However, an alert dental professional may indeed notice changes over time in jawbone density in a panoramic X-ray.
The disease is insidious, taking years to develop. It rarely offers any symptoms until the first bone fracture from a sudden bump or fall. Although enormous strides have been taken to reverse bone loss in the past few years, the statistics for this disease remain staggering. According to the National Osteoporosis Foundation, the disease is a major health threat for an estimated 44 million Americans. The NOF estimates about 10 million individuals have the disease (8 million are female), while another 34 million are at risk for osteoporosis with low bone mass and related bone fractures. Although thought of as a disease of the elderly, it can be diagnosed at any age. The economic burden of osteoporotic fractures is also great. In 1995, the NOF reported that these fractures were the cause of 432,000 hospital admissions, 2.5 million physician visits, and 180,000 nursing home admissions. The direct cost of osteoporotic fractures is estimated to be $18 billion per year.
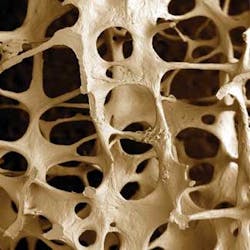
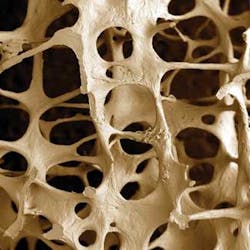
The body’s bones are continually changing, with a constant removal of old bone and a subsequent replacement with new bone. When this delicate balance of bone breakdown and rebuilding is altered, possibly through menopause or advancing age, more bone is broken down than rebuilt. The changes within cancellous bone as a consequence of bone loss leave large areas of unsupported bone, as the individual trabecular plates within the bone are lost. These appear as dark holes in a radiograph instead of the white, filigree, or lined appearance of denser bone. The consequence of this imbalance is a disordered skeletal architecture, reduced bone mass, and increased fracture risk.
People with osteoporosis and periodontal disease have a double whammy - periodontal disease appears clinically to be more progressive and destructive. Although the link between periodontal disease and osteoporosis is identified, the bone of contention is why. Does low mineral density make the bones more susceptible to breakdown from periodontal disease, or does the inflammation from perio disease make the bones break down?
Dr. Richard H. Carmona, the U.S. Surgeon General, issued a first-ever report about bone health in October 2004 to increase awareness of osteoporosis and other bone-weakening diseases with the general public, health-care professionals, and legislators. The report states: “Bone health is critically important to the overall health and quality of life of Americans.” He has a “bone” to pick with the American public because not enough bone-health practices are being carried out, even though much is known about and can be done to stop the progress of osteoporosis. Government estimates in the report say one-half of Americans over age 50 will run the risk of fractures in 2020 from osteoporosis unless they get enough calcium (1,200 mg per day), vitamin D (400 to 800 IU per day), and physical activity (weight-bearing exercise). Surgeon General Carmona said in a statement, “Osteoporosis isn’t just your grandmother’s disease. We all need to take better care of our bones. The good news is that you are never too young or too old to improve your bone health. With healthy nutrition, physical activity every day, and regular medical checkups and screenings, Americans of all ages can have stronger bones and live longer, healthier lives.”
By age 20, the average woman has 98 percent of her skeletal mass. Calcium is critical for heart health and if not ingested, it will be taken out of the bones. In the years following menopause, a woman can lose up to 20 percent of her bone mass, making her more susceptible to osteoporosis. Fractures may heal completely or may lead to chronic pain, disability, and death. One-third of patients with a hip fracture will fracture the opposite hip, and up to 25 percent of hip-fracture patients require long-term or rehab care. Of those with past hip fractures, only 40 percent fully regain the level of independence. Eating foods rich in calcium and vitamin D, maintaining a healthy weight, and engaging in weight-bearing activity at least 30 minutes each day are recommendations to maintain bone health. Reduce the risk of falls by removing household items that may lead to tripping or falling, improve ambient lighting, and have regular vision testing.
No bones about it, the sooner the disease is detected, the better the prognosis for the patient. But when people are unaware of the disease, the testing, available medications, or preventative measures, it’s rather difficult to expect the disease statistics to change. Many patients who experience unexpected fractures have no idea their fracture is an indication of a larger problem. McNeil Nutritionals did a study and found that only 23 percent of women are even aware they should have at least 1,000 mg of calcium a day.
The hope is that the Surgeon General’s report will help make a difference. Tommy G. Thompson, U.S. Secretary of Health and Human Services, added: “This report will shape the way we approach, talk, and act about bone diseases. The more we learn, the more we realize that so many diseases are preventable, from obesity to many types of cancer and now bone disease.”
Jan Britt may not have expected the news she received when she visited her periodontist, but she is grateful that he took the time to review her X-rays so closely. Osteoporosis is a quiet disease that we should all be aware of and watching for in our patients and ourselves. RDH