The Perio-Systemic Link
by Deborah M. Lyle
An examination of the evidence about periodontal infections and adverse pregnancy outcomes raises the question: Can intervention reduce risk?
Preterm birth (PTB) is a primary cause of perinatal complications (morbidity) and infant deaths (mortality from birth to one year) in the United States. Preterm birth often results in low birthweight (LBW) infants and a multitude of medical and neurological complications. Preterm birth is defined as a live birth before 37 weeks of gestation. It is further broken down into moderately preterm (32 to 36 weeks) and very preterm (under 32 weeks).1
Low birthweight is defined as less than 2,500 grams or 5 pounds. Additional classification includes moderately low birthweight (1,500 to 2,499 grams) and very low birthweight (less than 1,500 grams or 3 pounds).1
The classifications of moderate and very PTB/LBW correspond clinically with increasing mortality and morbidity. In the United States, 12.1 percent (one in eight) of live births were preterm and 7.8 percent (one in 13) were LBW. Healthy People 2010 has set objectives for PTB and LBW of 7.6 percent and 5.0 percent respectively.1
Health-care disparities are also evident with the incidence of PTB/LBW infants. In the United States, PTB is highest for African American infants (17.6 percent), followed by Native Americans (12.9 percent), Hispanics (11.4 percent), whites (10.7 percent), and Asians (10.2 percent). Between 2000 and 2002, African American infants were, on average, two times as likely as Hispanic infants to be born with low birthweight; 13.2 percent vs. 6.5 percent respectively.1 Other variables that have been shown or suggested to impact PT/LBW are years of education, socioeconomic status, age, marital status, and frequency of prenatal care.
Facts versus myths
One might think that a developed country such as the United States, with a health-care system that is in the forefront of research and development, would have one of the lowest mortality rates for live births. It may surprise you to know that an international comparison from 1999 showed the U.S. ranked 28th among selected countries. The U.S. infant mortality rate was more than two times higher than the infant mortality rate of Hong Kong (7.1 percent vs. 3.1 percent respectively). Other countries with a lower infant mortality rate include Japan, Sweden, Singapore, Finland, Canada, Czech Republic and Israel.
What is more startling is that from 1992, LBW increased from 7.1 percent to 7.8 percent and PTB from 10.7 percent to 12.1 percent.1
The perio-adverse pregnancy link
Infection and the host immune response as it pertains to periodontal and systemic diseases both collectively and separately have been the focus of the dental and medical literature in recent years. Gram-negative infections and subclinical infections may be important causes of PTB. Specifically, bacteria or their by-products (endotoxins) enter the uterine cavity via the lower genital tract or bloodstream.2,3 These microbes or their by-products can lead to prostaglandin production or directly to uterine muscle contraction mediated through a cytokine cascade.
Studies show there are a number of biochemical markers of infection present with premature labor. Prostaglandins are involved in labor at term and most likely in preterm labor. Additionally, some in vitro studies have shown interleukins (IL) and tumor necrosis factor (TNF) stimulate gestational tissues to produce prostaglandins and metalloproteases, and interleukin-1 (IL-1) and endotoxins stimulate uterine muscle contractions.4 The pathogenesis of periodontal infections is also impacted by the expression of these biochemical markers of the immunoinflammatory response leading to bone loss.
The evidence on the association between periodontal infections and adverse pregnancy is not clear. A recent systematic review identified 660 studies but only 12 studies were included in the analysis based on established inclusion criteria. Several studies implicated periodontal disease as a risk factor for PTB/LBW but only a few assessed the impact of prevention and treatment of periodontal disease on outcomes. Collectively, the reviewer concluded:5
• Periodontal disease may be a risk factor for PTB/LBW.
• It is unclear whether periodontal diseases play a causal role in adverse pregnancy outcomes.
• Preliminary evidence suggests that periodontal intervention may reduce adverse pregnancy outcomes.
• Additional studies, specifically longitudinal and epidemiological, and interventions studies are needed.
Although there are very few, intervention studies have revealed information that will help researchers and practitioners alike. In a 2002 study by Lopez et al.,6 400 pregnant women with periodontal disease between the ages of 18 to 35 were enrolled while receiving prenatal care from a clinic in Chile. The women were from low socioeconomic status and a mixture of Spanish and local aboriginal descent. The mean age was 27.5 and 24.5 percent were single. The subjects were randomly assigned to either the treatment or control group. The treatment group received periodontal therapy before 28 weeks of gestation, and the control group received periodontal therapy after delivery.
Treatment consisted of plaque control instructions and scaling and root planing (SRP) performed under local anesthesia. Subjects were instructed to rinse with 0.12 percent chlorhexidine once a day, and maintenance therapy was provided every two to three weeks until delivery. Subjects with severe aggressive periodontitis (29) were given 250 mg metronidazole and 500 mg of amoxicillin three times a day for seven days in addition to the SRP and self-care instructions.
After receiving periodontal therapy, clinical parameters were comparable to periodontal health and were statistically significantly lower than the control group. The results showed that the control group had more than five times the incidence of PTB and LBW compared to the treatment group. Other risk factors known to contribute to PTB/LBW were identified from the medical history and analyzed. The data revealed that periodontal disease had the strongest factor with an odds ratio of 4.70. The researchers concluded that periodontal disease appears to be an independent risk factor for PTB/LBW and periodontal therapy significantly reduces the rates of PTB/LBW in this population of women.
A more recent, randomized clinical trial of 366 pregnant women was stratified into three treatment groups based on previous spontaneous preterm birth (SPTB) at under 35 weeks and a body mass index less than 19.8 or bacterial vaginosis. Group 1 received supragingival scaling and polishing plus placebo capsule. Group 2 received SRP plus placebo capsule. Group 3 received SRP plus 250 mg metronidazole capsules three times a day for seven days.
The control group (untreated reference group) consisted of 723 pregnant women meeting the same criteria for periodontal disease who were enrolled in a prospective study. Each subject received a manual toothbrush, dental floss, fluoride toothpaste, and verbal self-care instructions. The sample population was 85 percent African American, 13.4 percent married with a mean age of 22.5.
The results indicate that performing SRP in pregnant women with periodontitis may reduce PTB in this population. Interestingly, metronidazole did not improve outcomes with the SRP group demonstrating the lowest PTB of 0.8 percent. It is important to note that all groups had lower rates than the reference group.7
Periodontal management
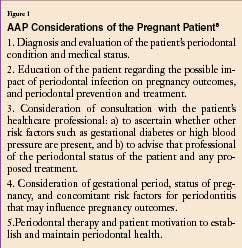
The American Academy of Periodontology (AAP) published a statement in the March issue of the Journal of Periodontology regarding the management of pregnant patients. Not surprisingly, treatment considerations include diagnosis and evaluation of the patient's periodontal condition and medical status. The complete list is shown in Figure 1.
The American Dental Hygienists' Association provides a fact sheet on premature birth on their Web site at www.adha.org/oralhealth/premature_birth.htm. A new, eight-page patient education brochure titled, Healthy Mouth, Healthy Body, is available for a nominal fee. It covers the relationship between systemic health and oral health, including PTB/LBW. It can be purchased via the Internet at www.adha.org/shopping/patient.htm.
Early evidence seems to support the importance of diagnosis and subsequent treatment of periodontal infections for pregnant women. In addition to the traditional medical and dental health history, follow-up questions regarding history of PTB/LBW infants and prenatal care should be documented.
Our current understanding about the possible risk of untreated periodontal infections and adverse pregnancies should be discussed and treatment options to eliminate disease presented.
Self-care options should include all techniques to reduce the bacterial challenge, both supragingivally and subgingivally, by either mechanical or power products such as toothbrushes, floss and interproximal devices, and oral irrigators. Chemotherapeutics for both therapy and prevention should also be considered, provided they are not contraindicated during pregnancy. It is important to be clear about the current evidence and not overstate the results so individuals can make informed decisions about treatment.
Another area of research is the impact of dental radiation exposure and the incidence of PTB/LBW. A recent case-controlled study concluded that dental radiography during pregnancy is associated with LBW, specifically with term low birthweight.9 This study led the American Dental Association to reinforce the proper use of shielding and to recommend postponement of elective dental radiographs.10
Future trends impacting care
If additional intervention studies conclusively show that periodontal therapy and prevention significantly reduce the incidence of adverse pregnancies (PTB/LBW), then dental hygienists will play a significant and necessary part of prenatal care. Dental hygienists are uniquely qualified to provide the therapy and self-care recommendations that early studies have shown to reduce PTB/LBW infants.
It is exciting to think that dental hygienists may contribute to meeting the Healthy People 2010 objectives of reducing PTB/LBW statistics. A key challenge to meeting these objectives is to reduce the health-care disparities among individual ethnic groups who have a higher incidence of adverse pregnancies. This may open up alternative avenues for the dental hygienist in public health and meeting the needs of the underserved populations that certainly include pregnant women. This is an exciting time to be a dental hygienist.
Deborah M. Lyle, RDH, MS, is currently employed by Waterpik Technologies as the manager of professional marketing and education. Her tenure in dental hygiene includes private practice, faculty appointments, and research. Lyle is also chair of the ADHA Council on Education. She may be reached at [email protected].
References1. Perinatal Health in the United States. www.marchofdimes.com/peristats. Accessed July 30, 2004.
2. Gibbs RS. The relationship between infections and adverse pregnancy outcomes: An overview. Ann Periodontol 2001; 1(6): 153-163.
3. Hay PE, et al. Abnormal bacterial colonization of the genital tract and subsequent preterm delivery and late miscarriage. Br Med J 1994; 308:295-298.
4. Gibbs RS, et al. A review of premature birth and subclinical infection. Am J Obstet Gynecol 1992; 166:1515-1528.
5. Scannapieco FA, Bush RB, Paju S. Periodontal disease as a risk factor for adverse pregnancy outcomes. A systematic review. Ann Periodontol 2003; 8(1):70-78.
6. Lopez NJ, Smith PC, Gutierrez J. Periodontal therapy may reduce the risk of preterm low birth weight in women with periodontal disease: A randomized controlled trial. J Periodontol 2002; 73(8):911-924.
7. Jeffcoat M et al. Periodontal disease and preterm birth: Results from a pilot intervention study. J Periodontol 2003; 74(8):1214-1218.
8. Academy Report. American Academy of Periodontology statement regarding periodontal management of the pregnant patient. J Periodontol 2004; 74(3):495.
9. Hufoel PP, et al. Antepartum dental radiography and infant low birth weight. JAMA 2004; 291(16):1987-1993.
10. ADA News Release. www.ada.org/public/media/releases/0404_release03.asp. Accessed April 28, 2004.