Vaginal Lichen Planus
by Nancy W. Burkhart, RDH, EdD
[email protected]
Vulvovaginal lichen planus is sometimes referred to as the vulvovaginal-gingival syndrome because of the association with vaginal lichen planus and lichen planus that occurs orally — specifically on the gingiva. Genital lichen planus occurs not only in females but also in males, usually on the head of the penis.
Interestingly, men who are circumcised rarely develop genital lichen planus. The male counterpart is easily diagnosed since the tissue area can be seen more easily. With female genital lichen planus, the patient may have vague symptoms such as chronic yeast infections for some time before lichen planus is ever diagnosed and treated.
Many dental professionals and gynecologist/internal medicine specialists are examining a patient within their own specialty area and may fail to connect the diagnosis of lichen planus as occurring in both the oral, the vaginal, rectal, skin, esophageal, or vulva areas. Many women with the syndrome complain of chronic yeast infections, pain, pruritus, edema, and discomfort for some time prior to discovery. Depending upon the physician rendering care, the patient may be treated for yeast or fungal infections for years without real resolution.
Vulvovaginal lichen planus usually occurs in postmenopausal women. Due to vaginal thinning, hormonal replacement is sometimes used to relieve the discomfort and get the tissue under control. It is thought that low estrogen is instrumental in contributing to vaginal dryness and thinning because of the patient’s age (usually 50-plus). Younger women are diagnosed with vaginal lichen planus as well, but not as frequently.
Vulvodenia is often cited when pain is present, but everything appears normal. So getting the correct diagnosis is crucial. Onset of vaginal lichen planus is gradual and may be intermittent. Complaints may also fall into this category of vulvodenia early on. Although some women have skin lesions of lichen planus and oral lesions simultaneously, the genital lesions are normally only discussed with the gynecologist or in some cases, the primary physician.
Dental professionals often do not know about this problem or its connection with oral lichen planus. That is, unless the patient mentions or asks about any association; otherwise the conversation never takes place. Often, women may have both oral and vaginal lichen planus concurrently and neither the dentist nor the gynecologist asks about any issues related to those outside of their specialty. The physician may treat women for chronic yeast problems for years before a connection is made.
At the same time, a person who is not greatly affected by oral lesions or someone who has not been diagnosed with oral lichen planus — even though the lichen is intermittent and vaguely present — may never connect the two.
Sometimes ulcerative or just “red gingival tissue” may be called “desquamative gingivitis,” and no real cause is diagnosed. Depending upon the appearance of the oral lichen and the symptoms related to the particular patient, signs of the disorder may go undetected for many years. Since lichen planus can be intermittent, lesions may clear only to reappear at a later time, adding even more confusion to the issue.
Also, searching for “trigger” items for each patient is crucial in trying to establish an etiology.
Recently, I had the privilege of interviewing Dr. Elizabeth Edwards, a well-known dermatologist who provided a much needed seminar for our online International Oral Lichen Planus Support Group through Baylor College of Dentistry (http://bcdwp.web.tamhsc.edu/iolpdallas/webinars/recordings/). Dr. Edwards treats many patients who have vulvovaginal lichen planus and, in many cases, oral lichen planus as well. She also performs surgical procedures on some of these patients in order to correct the scarring, closure, and damage to the vulvar/vaginal openings related to lichen planus.
Dr. Edwards has written extensively about the disorder and has published books on the subject. She has been involved in more than 50 clinical trials and research projects related to vaginal lichen planus. The surgical correction for the scarring and closure related to lichen planus is only performed by a select few physicians, and Dr. Edwards is well known for her focus in this surgical arena. Her dermatology practice is in Charlotte, N.C., and she is also board certified in internal medicine.
Lichen planus is a cell-mediated immune response disease. The cutaneous areas are attacked, and the oral, vulva, vagina, and/or esophageal region may be involved. Sometimes only one area may be involved or multiple areas may be of concern at any given episode. Some autoimmune diseases such as pemphigus vulgaris, pemphigoid, discoid lupus, and scleroderma are other autoimmune diseases that may affect the skin.
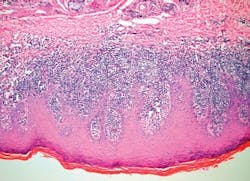
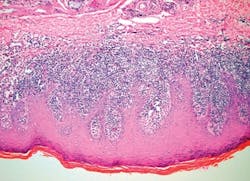
Lichen planus is thought by many to be an autoimmune type disease, but as yet no antigen has been found that would soundly classify it as autoimmune. Since lichen planus is classified as a type IV hypersensitivity reaction, the lymphocytes increase at the basement membrane and ultimately dissolve or liquefy the basement zone (see Figure 1).
Women are affected by the vaginal lichen planus as well as a condition called lichen sclerosis, which has a very similar appearance to lichen planus and may mimic similar characteristics. Lichen sclerosis is rare but does occur in the female genitalia and the perianal skin. A biopsy must be performed to rule out all other alternative skin disease states. Vulvovaginal lichen planus was at one time thought to be rare, but we know that it is much more common and may be misdiagnosed or often missed in evaluations.
Any thick skin that gets wet appears white. The skin may be red in the vaginal area, and some other areas may appear white with the classic striated appearance. Erosions and ulcers may be present in some cases. The rectal area may be affected with or without vaginal changes. Scarring may occur covering the vagina opening and also the clitoris with pruritus and burning. Intercourse is painful with vaginal lichen planus, and this problem is usually one that sends the female to the gynecologist.
Esophageal lichen planus may be missed unless a connection is made regarding other oral or vaginal complaints. The esophageal tissue is very much like the vaginal tissue, and the person may complain of difficulty in swallowing due to the scarring that is occurring. The upper esophagus is affected, and acid from the stomach can reflux and worsen the lichen planus. Erosions of the tissues cause problems with eating and discomfort in general.
If a women has vaginal lichen planus, she is more likely to have oral lichen planus. Esophageal and rectal lichen planus may occur as well.
Dr. Edwards made some key recommendations during the session with the International Oral Lichen Planus Support Group.
She suggests that the patient stop irritants such as lubricants, irritating toothpaste/mouth rinses, and control infections such as yeast. The corticosteroids that are prescribed for vaginal lesions will lower the immune system, allowing the opportunistic candida to increase. She states that it is often working back and forth to control the lichen planus and the candida to promote a balance.
As in the mouth, there is a problem getting the medications to adhere to the vaginal tissues. Both tacrolimus and pimecrolimus ointment may be used for vaginal lichen planus, but are irritating and burn. So options may be limited with some patients. Dr. Edwards commented that sometimes dermatologists must take advantage of currently marketed medications and individualize them for certain disorders such as lichen planus, since there is no specific medication to treat the lichen planus.
Surgical procedures are needed in cases where closure has occurred. Vulva and vaginal scarring can and often do occur and the area may be quickly scarred completely shut. Early intervention is necessary to limit the scarring and to treat the area in order to keep the tissue open. Clobetasol gel injected into the vagina used with a dilator is often recommended to keep the area open and keep the vaginal walls from closing completely.
Methotrexate is used in severe cases and is often used for other autoimmune diseases as well. Medications are often used with trial and error since they do not always react the same with all patients. Tumor necrosis factor alpha inhibitors are sometimes prescribed but are very expensive, especially for patients who do not have insurance coverage and who pay out of pocket. Squamous cell carcinoma of the mouth and vulvavaginal-gingival syndrome can occur, and usually occurs in patients who have had poorly controlled lichen planus in any location. Squamous cell carcinoma of the vaginal tissues does occur as well with poorly controlled tissues.
Why do some people develop lichen planus while others do not? This is a question that has not been answered. What causes lichen planus? Since an antigen has not been found, this has been a mystery and even the classification is uncertain.
Gynecologists have been more aware of vaginal lichen planus in the past few years. However, clinicians who specialize tend to pay attention to their own area of specialty. Linking the dots and making the connection is important in getting early treatment for patients. Dentists, hygienists, physicians, gynecologists, and ENTs need to ask relevant questions in treating the total patient.
Lichenoid drug reactions may occur. Medications may work in combination and include the medications that postmenopausal women may be prescribed. Medications such as cholesterol medications, thyroid medications, and heart medications are often implicated and many may not be able to be substituted.
Even though there may not be a cure, a patient can be made comfortable. Dr. Edwards does not want to hear that a patient has been told to “learn to live with it.” Treatment is available and very necessary to halt progression of scarring and in preventing transformation to squamous cell carcinoma.
Most patients seen by Dr. Edwards who have vaginal lichen planus have gingival lichen planus.
For lip lesions, steroid rosacea and scarring can occur. Protopic is used for treatment usually. This type of lichen planus is visible to others and the patients are very self-conscious in interacting with others.
Dr. Edwards always recommends toothpaste free of strong flavoring agents. Sodium bicarbonate is sometimes tolerated much better. Eliminating any food or product that burns is recommended.
After being involved with so many patients in my work with the International Oral Lichen Planus Support Group, I have gained a lot of knowledge in what works and does not work with this group of patients. Gentle and careful oral cleanings are recommended. Research supports the fact that lower plaque levels reduce the inflammation in the mouth. The tissues are friable and easily stripped.
Finding practitioners who understand the disease process is important for effective treatment. Harsh dental products, air polishers, and high settings on ultrasonic units may cause more damage to the already sensitive oral tissues. Sometimes, hand instruments are best in highly ulcerated lichen planus. Always recommend that patients with oral lichen planus see their physician/gynecologist and let these physicians know that they have been diagnosed with oral lichen planus. The correct diagnosis and early treatment will prevent scarring, closure, future surgery, and possibly cancer for the patient.
As always, keep asking good questions and always listen to your patients!
References
• Burkhart N. Lichenoid reactions. RDH 2009; 29(10): 86-92.
• Burkhart N. Lichen planus of the lip. RDH 2009; 29(5): 66-67.
• Burkhart N. Lichen planus. RDH 2007; 27(2): 65-66
• Jensen R, Worsaae N, Melgaard B. Oral lichen sclerosus et atrophicus: A case report.
• Oral Surg Oral Med Oral Pathol Radiol Endod 2002; 94:702-6.
• Edwards L. Vulvar lichen planus. Arch Dermatol.1989; 125:1677-1680.
• Edwards L. Dermatologic causes of vaginitis: A clinical review. Dermatol Clin 2010: 28:727-735.
• Eisen D. The vulvovaginal-gingival syndrome of lichen planus. The clinical characteristics of 22 patients. Arch Dermatol. 1994; 130(11): 1379-1382.
• Stojanovic L. Lunder T, Rener-Sitar K, Mlakar, B, Maticic M. Thorough clinical evaluation of skin, as well as oral, genital and anal mucosa is beneficial in lichen planus patients. Coll Antropol. 2011; 35(1): 15-20.
• Fox LP, Lightdale CJ, Grossman ME. Lichen planus of the esophagus: what dermatologists need to know. J Am Acad Dermatol. 2011; 65(1): 175-83.
Nancy W. Burkhart, BSDH, EdD, is an adjunct associate professor in the department of periodontics, Baylor College of Dentistry and the Texas A & M Health Science Center, Dallas. Dr. Burkhart is founder and cohost of the International Oral Lichen Planus Support Group (http://bcdwp.web.tamhsc.edu/iolpdallas/) and co-author of General and Oral Pathology for the Dental Hygienist. She was a 2006 Crest/ADHA award winner. Her website for seminars is www.nancywburkhart.com.
Dr. Nancy W. Burkhart established the International Oral Lichen Planus Support Group in 1997 through Baylor College of Dentistry, Department of Periodontics.
It is co-hosted by Dr. Terry Rees and Dr. Burkhart. In addition to the recordings link listed in the article, the site can be accessed at: http://bcdwp.web.tamhsc.edu/iolpdallas/.
Past RDH Issues