Periodontal Disease and Atherosclerosis
by C. Austin Risbeck, RDH
The scope of dental hygiene is changing as we now enter into a new phase of total health promotion and education. This phase is based on recent evidence linking periodontal disease to cardiovascular disease (CVD). A special report released by Harvard Medical School on preventing heart disease suggests that if you commit yourself to four basic lifestyle changes — not smoking, eating healthfully, exercising regularly, and controlling your blood pressure — you can significantly reduce your chances of having a first heart attack. According to the latest research, reported by the American Dental Hygienists' Association, a healthy lifestyle that includes daily flossing may promote total health as much as diet and exercise.
The Surgeon General's Report titled, "Oral Health in America, May 2000," reported that "oral health is integral to overall health." One the key elements of the report included the advice to "change perceptions regarding oral health and disease so that oral health becomes an accepted component of general health."
Total health promotion includes education on reducing the risk factors for periodontal disease, as well as reducing the major controllable risk factors associated with CVD. Early prevention and intervention can significantly delay the onset of atherosclerosis and cardiovascular disease which may result in disability and death from heart attack and stroke.
Cardiovascular disease ranks as America's number one killer, claiming the lives of over 40 percent of the nearly 2.4 million Americans who die each year. Since 1900, CVD has been the number one killer in the United States every year but 1918.
Information from the American Heart Association's 2002 Heart and Stroke Statistical Update reveals that more than 2,600 Americans die of CVD each day, an average of one death every 33 seconds. About every 29 seconds an American will suffer a coronary event, and about every minute someone will die from one. This year an estimated 1,100,000 Americans will have a new or recurrent coronary attack. About 650,000 of these will be first attacks and 450,000 will be recurrent attacks. Over 45 percent of the people who experience a coronary attack in a given year will die from it. Atherosclerosis is a leading cause of many deaths from heart attack and stroke. It accounts for nearly three-fourths of all deaths from CVD.
The Journal of Periodontology confirms that people with periodontal disease are at a greater risk for CVD. Ongoing studies conducted at the University of North Carolina at Chapel Hill and the State University of New York at Buffalo demonstrate the association between chronic periodontitis and CVD, implicating periodontal disease as a risk factor for the development of cardiovascular disease. Subjects were also assessed for levels of an inflammation marker known as C-reactive protein (CRP).
Moderate elevation of CRP has been found to be a predictor for increased risk for CVD. Elevated CRP levels were found in periodontal patients.
According to the American Academy of Periodontology, periodontal disease needs to be considered as a major contributor to increased levels of CRP by the medical community. A recent study published by The New England Journal of Medicine, suggests that inflammation plays a key role in CVD. Elevated CRP levels were identified as a stronger predictor of heart attacks than elevated cholesterol levels. Inflammation is believed to play a role in atherosclerosis that can lead to a heart attack or stroke. Studies have suggested that infection may also promote atherosclerosis. Periodontal disease is a local inflammatory process triggered by bacterial infection. Porphyromonas gingivalis, according to Boston University, accelerates the progression of atherosclerosis.
Researchers at Harvard Medical School have learned that persistent low-level inflammation in the arteries, triggered by infection, promotes the formation of atherosclerotic plaques and leaves them more vulnerable to the ruptures that cause heart attacks and strokes.
Periodontal disease is now a risk factor for atherosclerosis and its thrombotic complications, according the the Annuals of Periodontology. Atherosclerosis, a major component of CVD, is a gradual process that develops over the course of a lifetime which doesn't manifest itself until later in life when periodontal disease is most prevalent. Heart attacks and stroke are primarily caused by the effects of atherosclerosis.
Atherosclerosis
Atherosclerosis is defined as a disease in which the arteries are hardened and narrowed as a result of plaque, which has built up along the inside of the artery walls. The disease is a chief contributor to CVD. Atherosclerosis involves an unnatural buildup of plaque, which comprises of fats, cholesterol, calcium, and other materials. These masses of plaque may eventually lead to a partial or complete blockage of the blood flow through the artery, leading to the failure of cells and organs throughout the body as they are starved of oxygen.
Atherosclerosis may begin as early as childhood, but it is the advanced stages of this condition that are most dangerous later in life. These advanced stages can cause a narrowing of the artery and speed the rate at which the artery is blocked or closed altogether. If the affected artery is one of the coronary arteries, then a lack of oxygen-rich blood to the heart could cause coronary artery disease and, consequently, increase an individual's risk of heart attack, cardiac arrest, and sudden cardiac death.
The source of the above information is Heart Center Online. It can be found by going to www.heartcenteronline.com.
The Centers for Disease Control and Prevention says that the atherosclerosis process resembles many aspects of chronic inflammation, a response that may be promoted by microorganisms. Studies have shown an infectious etiology and that bacterial and viral agents could contribute to atherogenesis. During the past decade, several reports have suggested a relationship between chronic oral infections, such as periodontitis, and cardiovascular disease.
How periodontitis becomes a factor
According to Dr. Ernesto De Nardin at the University at Buffalo, "Persistent infections such as periodontitis induce inflammatory and immune responses which may contribute to atherogenesis, and in conjunction with other risk factors, may lead to coronary heart disease. Periodontal diseases are bacterial infections associated with bacteremia, inflammation, and a strong immune response, all of which may represent significant risk factors for the development of atherosclerosis, coronary heart disease, and myocardial infarction."
Periodontitis is a local inflammatory process mediating destruction of periodontal tissues triggered by bacterial insult. However, the disease is also characterized by systemic inflammatory host responses that may contribute, in part, to the recently reported higher risk for CVD among patients with periodontitis, according to the Journal of Periodontology.
Elevated levels of CRP explain one reason why periodontitis is a risk factor for CVD. There are elevated levels of CRP associated with infection, with subgingival organisms often associated with periodontal disease, including P. gingivalis. The extent of increase in CRP levels in periodontitis patients depends on the severity of the disease after adjusting for age, smoking, body mass index, triglycerides, and cholesterol. Studies at the University of Texas, Health Science Center at San Antonio have shown a significant decrease in CRP levels following scaling and root planing.
The body releases CRP as part of its response to infection and injury, and the protein is a known marker of inflammation. High levels of CRP in the blood mean that there is inflammation somewhere in the body. During infection, for example, blood CRP levels temporarily soar as the immune system jumps into action. Chronic CRP levels have been linked to an increased risk of CVD.
It has been reported by the University of Western Ontario School of Dentistry that patients with periodontal inflammation, a Streptococcus sanguis protein associated with platelet aggression and bacteremia associated with P. gingivalis may contribute to some acute thromboembolic events. P. gingivalis can multiply within and activate endothelial cells and also expresses a platelet aggression factor. P. gingivalis has been found in the walls of aortic tissue, according to the Journal of Periodontology.
The development of atherosclerosis
Injury to the endothelial cells either by oral infection or cholesterol is the first step toward atherosclerosis. According to Heart Center Online, the toxins present in LDL (bad) cholesterol that damage the endothelial cells and help form lesions on the artery walls. These lesions become sticky and attract other fatty material and a buildup of plaque begins.
As fatty material accumulates, some of the plaque formations acquire a relatively thick covering. These are considered to be stable plaques and are a primary cause of narrowed arteries. Other plaques have a thinner, more volatile coating. These are called unstable plaques, because the coating can be stripped off, releasing small fatty particles into the bloodstream (plaque rupture).
An article published by Jeffrey Porro titled, "Cardiovascular Disease and the Endothelium," best describes the pathogenesis of atherosclerosis. This is part of a series of essays developed to educate the general public about the benefits of biomedical research, and how research leads to scientific progress, and improved health. This article can be found in its entirety at www.faseb.org/ opar/endothelium/endothelium.html.
Fibrous plaque can be a serious health problem, not only because it can narrow the arteries, but also because it can be a source of thrombosis (blood clot). When a fibrous plaque becomes unstable and breaks or tears, thrombi can form on the surface of the plaque. If these clots are large enough, they can block the artery that already has been narrowed by fibrous plaque. If such a clot forms in an artery leading to the heart, the blockage that results can cause a heart attack. When a clot cuts off blood to the brain, the result is a stroke.
Scientists have been searching for causes of atherosclerosis for a long time. They have known for more than a century that people who eat diets high in animal fat tend to have high levels of cholesterol in their bloodstream. And it has been well established that elevated cholesterol in the bloodstream is very likely to lead to atherosclerosis and the health dangers that come with it.
An unsuccessful battle against cholesterol
Blood consists of a liquid (plasma) and several kinds of blood cells, including red cells, white cells, and platelets. Blood plasma also carries a huge variety of different substances from one part of the body to another. One key substance is cholesterol, one of the many lipids found in plasma.
Cholesterol is carried in the blood from place to place on special particles called lipoproteins. One kind of lipoprotein particle, low-density lipoprotein or LDL, carries cholesterol to different parts of the body, including the walls of the arteries, and can lead to problems when it carries more cholesterol than cells require to function normally. Another kind, high-density lipoprotein or HDL, carries cholesterol away from the artery walls and eventually out of the body. There is a direct link between elevated levels of LDL and atherosclerosis, and decreased levels of HDL, which is protective.
Atherosclerosis appears to be a healing response by the body that goes haywire. When any part of the body is damaged whether by infection with bacteria, sports injury, a burn, etc., the body increases the flow of blood to the injured area and puts white blood cells to work there. White blood cells surround the bacteria or the damaged tissue. Then, together with other cells in the damaged tissue, the white blood cells neutralize and remove whatever is causing the injury and repair the damage. Researchers now believe that a similar process occurs in atherosclerosis. But the process of inflammation and healing the injury may be slow and excessive, and the result can be increased risk of stroke and heart attack.
When high levels of LDL are in the blood, a small amount of the LDL that builds up in the artery wall becomes oxidized. This occurs through chemical reactions in the endothelium that changes the LDL by adding extra oxygen atoms to it. This is important because oxidized LDL is one of the triggers that can set off a chain reaction.
It appears that the more LDL there is in the blood, the more oxidized LDL will be produced. Oxidized LDL injures the endothelium and causes the surface of the endothelium to express a special kind of molecular "glue" called ELAMS (endothelial-leukocytes adhesion molecules). These cause certain kinds of white blood cells (monocytes and T-lymphocytes), which are floating by in the bloodstream, to adhere to the endothelium.
Scientists now believe that this phase of atherosclerosis is a form of the body's normal healing process. What the endothelium does during atherosclerosis is what all injured tissue does to a point.
As mentioned, when any part of the body is hurt, white blood cells help neutralize bacteria or other agents that are causing injury and thus help in the process of repairing damaged tissue. It turns out that most injured tissue uses adhesion molecules to make white blood cells adhere to the spots where they are needed. The problem in atherosclerosis is that, after the white blood cells stick to the endothelium, the healing process goes off track.
Specifically, the white blood cells move between and below the endothelium and start to do real damage in two major ways. In a complex chemical reaction, the white blood cells cause some of the muscle cells in the artery wall to grow. The white blood cells also incorporate the particles into the artery wall, consuming oxidized LDL particles.
The result is a fatty streak, which can progress to become a fibrous plaque. These intricate processes occur in the tissues beneath the endothelium and are enhanced by molecules secreted by the blood platelets, macrophages, and smooth muscle cells.
Best therapy? Change lifestyle
In the future, it may be possible to devise new diagnostic tools. For example, current research may well lead to sophisticated blood tests that will detect the molecules, such as adhesion molecules that are produced at each phase of the disease. Such tests could be an even more effective early warning system for atherosclerosis.
Several therapies are being used to treat atherosclerosis. One of them is having the patient make lifestyle changes. Although scientists have not identified the direct physiological link between smoking and atherosclerosis, stopping smoking lowers the risk of the disease dramatically. For at-risk patients with moderately high levels of serum cholesterol, dietary intervention and increased exercise also have proved effective.
As dental hygienists, we can provide enough education so our patients can make informed decisions based on the risk factors identified while taking a medical history. We should assist our patients in identifying the major controllable risk factors associated with CVD to establish risk of atherosclerosis and cardiovascular disease, offer the necessary lifestyle changes to reduce their risk, and, by doing so, possibly preventing disability and death caused from atherosclerosis and cardiovascular disease.
The American Dental Hygienists' Association makes it perfectly clear that "dental hygienists don't make a diagnosis, they explain to the patient what they found and then urge them to see a physician." Dental hygienists, interacting with the medical community, have the power to reduce, eliminate and eventually eradicate the disparities associated with atherosclerosis and cardiovascular disease.
The American Heart Association states all health-care providers have the responsibility to be familiar with the risk factors for cardiovascular disease and stroke. By doing so, we can evaluate our own level of risk and do our best to live a healthy life, educate our families and patients about such a lifestyle, and collect a medical history related to risk factors and refer our patients, if necessary, to an appropriate medical provider for further evaluation.
Pinpointing risk factors
The Journal of the American Dental Association encourages oral health care providers to perform a screening for risk factors for cardiovascular disease, which will help develop a better overall view of a patient's general health.
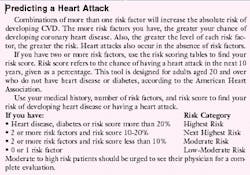
The American Heart Association has identified several risk factors. Some of them can be modified, treated or controlled, and some can't. The more risk factors you have, the greater your chance of developing coronary heart disease. Also, the greater the level of each risk factor, the greater the risk.
Studies have identified several factors that increase the risk of coronary heart disease and heart attack. Major risk factors are those that research has shown significantly increase the risk of cardiovascular disease, according to the American Heart Association.
The American Dental Association recommends that you consider the following major risk factors while taking a medical history: age, cigarette smoking, high blood pressure, elevated cholesterol levels, high-fasting blood sugar level, presence of diabetes, family history of diabetes, presence of heart disease, family history of heart disease, physical inactivity, and excess body weight.
As a dental hygienist I am compelled to include, and consider, diets that are too high in fat as a major controllable risk factor. Dietary intervention, to include education and counseling, should be a vital part of providing dental hygiene services. American diets are too high in fat, especially saturated fat, and cholesterol leading to atherosclerosis, heart attack, and stroke, according to the American Heart Association.
The American Dental Association claims that identifying patients at high risk of developing CVD is paramount to preventing initial coronary events. The ADA says all oral health care providers, including dental hygienists, are in a position to aid with both screening for and monitoring of risk factors associated with CVD, as well as to facilitate and provide patient education. The dental hygienist is in a position to notice these risk factors and symptoms while taking a medical history and conducting a thorough exam, according to the American Dental Hygienists' Association.
"The presence or absence of risk factors will significantly modify the patients cumulative lifetime risk. Risk factors for CVD begin at ages much younger than those at which a disease manifests its first symptom. Therefore, interventions to reduce the risk factors for CVD — such as smoking cessation, lowering blood pressure, reduction of high blood cholesterol, eating properly, and decreasing blood sugar levels — will change a person's lifetime risk of experiencing an adverse coronary event," writes Dr. Michael Glick, author of "Screening for traditional risk factors for cardiovascular disease: A review for oral health care providers," in the March 2002 issue of JADA.
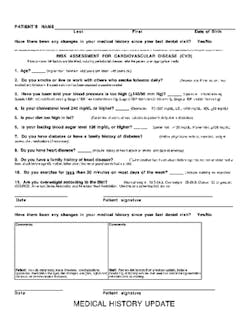
A comprehensive medical history including risk factors associated with CVD should be obtained and updated at every return hygiene visit. The Academy of General Dentistry says it is important that patients keep all members of the health-care team well informed of their medical history, lifestyles, and eating habits, so they can work together to identify any risks.
The medical history update form contains all the questions related to the risk factors associated with cardiovascular disease necessary to perform a risk assessment for cardiovascular disease. An example of these questions appear in the related illustration.
Final thoughts
Cardiovascular disease is one of the most preventable diseases in existence. Yet thousands of Americans are dying each day. It is important to identify the major controllable risk factors associated with cardiovascular disease, determine the level of risk, and inform our patients of the lifestyle to reduce risk of the disease.
Dental hygienists should screen for these risk factors while taking a medical history, and refer to an appropriate medical provider, if the patient is at high risk for developing cardiovascular disease.
Periodontal disease is one of the most common diseases. The disease has emerged as one of the many factors in the development of cardiovascular disease, but it is not considered as a major risk factor. As inflammation emerges as a major risk factor, periodontal disease will soon follow.
Our patients should avoid behaviors that put them at high risk, such as smoking. Smokers, both active and passive, are at significantly higher risk of developing severe early atherosclerosis. Also, our patients should avoid eating a high-fat diet, and should be educated about how to improve their diet and eating patterns.
Dental hygienists should monitor, not diagnose, patients' blood pressure and refer if their blood pressure continues to be elevated. We should also encourage increased physical activity and reductions in body weight.
Adults older than 20 years should have their cholesterol checked at least every five years, as well as their CRP levels. We can intervene with lifestyle changes to reduce the risk of possible disability and death from atherosclerosis and cardiovascular disease. Those with high levels of CRP are at higher risk than those with normal cholesterol levels. The two tests together are a better predictor of future coronary events.
This is a time when many Americans make resolutions and promises of improved lifestyle and health. Now is the time to encourage our patients to floss, and improve their oral health throughout the upcoming year. What an incredible opportunity we have to truly show we care about our patients.
We are concerned about not only their oral health, but their total health. We can ensure that the message of early intervention and disease prevention is brought home to each one of our patients. Total health promotion includes a lifestyle that minimizes the risk of future cardiovascular disease and stroke, which not only has a direct impact on our patients, but extends to their families, our families, and to ourselves.
Periodontal disease, combined with other risk factors, can increase a person's chance of having an adverse coronary event. Medical and dental professionals need to work together to improve health and quality of life. With preventive intervention, medical and dental professionals can do a better job of identifying risk factors — early enough to save lives.
C. Austin Risbeck, RDH, practices in an adult general dentistry office in San Francisco. He has been a CPR instructor with the American Heart Association since 1982 and currently volunteers as a health educator for the California AIDS Hotline. He can be contacted at tasman141414@ earthlink.net.
Recommended Web sites
• American Heart Association — An invaluable web page for identifying risk factors and the lifestyle changes necessary to reduce disability and death from cardiovascular disease and stroke.
http://www.americanheart.org
• Freedom From Smoking — Freedom From Smoking is a smoking cessation program from the American Lung Association providing strategies for maintaining a smoke free lifestyle.
http://www.lungusa.org/ffs
• Your Guide to Lowering High Blood Pressure — This Web page includes easy-to-understand information about high blood pressure, basic tips on how to control high blood pressure, suggested questions to ask your doctor, and heart-healthy recipes.
http://www.nhlbi.nih.gov/hbp/index.html
• Live Healthier, Live Longer — This Web page provides information for those who want to prevent heart disease; information for those with heart disease who want to reduce their risk of having a heart attack; a "how to" step-by-step guide to lowering cholesterol.
http://www.nhlbi.nih.gov/chd
• Heart Profilers — This Web site is a free interactive tool that provides personalized information, based on the latest clinical research, to enable heart disease patients, their families and care givers to manage their disease and make better treatment decisions.
http://www.americanheart.org/heartprofilers
• Food Fit — Food Fit provides personalized tools to make good food and active living easy and enjoyable; an in-depth nutritional analysis; and a fitness section to help get motivated.
http://www.foodfit.com
• American Diabetes Association — This Web page provides basic diabetes information, resources, healthy living, a diabetes risk test, and a section for health care professionals.
http://www.diabetes.org
• Just Move — Just Move has an exercise diary to keep track of your progress online, fitness resources, and information to help you decide which fitness type best describes your lifestyle.
http://www.justmove.org
• Aim for a Healthy Weight — This Web site gives health professionals, patients and the public vital information on clinical guidelines and practical tools for identifying, assessing, and treating overweight and obesity.
http://www.nhlbi.nih.gov/subsites/index.htm
(click on Aim for a Healthy Weight.)
• Heart Center Online — This cardiovascular health-care site provides cardiovascular patients and their families the tools they need to better understand the complex nature of heart-related conditions, treatments, and preventive care.
http://www.heartcenteronline.com
• American Dental Hygienists' Association
http://www.adha.org
• The American Academy of Periodontology
http://www.perio.org
Not just cholesterol
Inflammation is emerging as a major risk factor. Inflammation is believed to play a role in atherosclerosis that can lead to a heart attack or stroke, according to the November 2002 issue of The New England Journal of Medicine. This new study shows that a cholesterol test is not enough. The study found that the CRP test did a better job of predicting cardiovascular events than LDL cholesterol level. Those with high levels of inflammation are twice likely as those with high cholesterol to die from heart attacks and strokes. The CRP test is inexpensive and is already available.
The CRP test should not replace a cholesterol test which measures how much fat is lodged in the blood vessels of the heart; a CRP test shows how likely it is that those plaques will rupture. The study found that a combination of the two tests was the best method of predicting heart risk.
Risk factors: coronary heart disease
Extensive clinical and statistical studies have identified several factors that increase the risk of coronary heart disease and heart attack. Major risk factors are those that research has shown significantly increase the risk of cardiovascular disease.
The American Heart Association has identified several risk factors. Some of them can be modified, treated or controlled, and some cannot. The more risk factors one has, the greater the chance of developing coronary heart disease. Also, the greater the level of each risk factor, the greater the risk.
Major risk factors that cannot be changed
• Increasing age — About four out of five people who die of coronary heart disease are 65 or older.
• Gender — Men have a greater risk of heart attack than do women, and they have attacks earlier in life. Even after menopause, when women's death rate from heart disease increases, it is not as great as men's.
• Heredity — Children of parents with heart disease are more likely to develop it themselves. African Americans have more severe high blood pressure than Caucasians and a higher risk of heart disease. Just as age, sex, and race cannot be controlled, neither can family history. It therefore becomes even more important to treat and control other risk factors.
Major risk factors that can be modified, treated, or controlled
• Cigarette smoking — Smokers' risk of heart attack is more than twice that of nonsmokers. Cigarette smoking is the biggest risk factor for sudden cardiac death. Cigarette smoking also acts with other risk factors to greatly increase the risk for coronary heart disease.
• Lifestyle change: Stop smoking as soon as possible. Join a stop-smoking program such as Freedom From Smoking from the American Lung Association. The program gives many ideas on how to quit and stay off tobacco.
• High blood pressure — High blood pressure increases the heart's workload, causing the heart to enlarge and weaken. When combined with obesity, smoking, high blood cholesterol or diabetes, the risk of heart attack or stroke increases several times.
• Lifestyle change: The American Heart Association recommends the following to maximize the beneficial effects of diet on blood pressure:
• Limit salt intake
• Increase fruits and vegetables, and eat fat-free or low-fat dairy products
• Have blood pressure checked regularly
• Lose weight if you are overweight
• Be more active
• Limit alcohol to no more than two drinks a day
• Take medicine according to doctors' instructions
• Know what blood pressure should be and try to keep it at that level.
• High blood cholesterol — As blood cholesterol rises, so does risk of coronary heart disease. When other risk factors (such as high blood pressure and tobacco smoke) are present, this risk increases even more.
• Lifestyle change: Have cholesterol checked regularly. Take steps to lower it if it is high. Eat healthy foods that are low in saturated fat, cholesterol, and sodium; do not drink too much alcohol.
• Physical inactivity — A sedentary lifestyle is a risk factor for coronary heart disease. Regular, moderate-to-vigorous physical activity helps prevent heart and blood vessel disease.
• Lifestyle change: Talk to physician or nurse about proper activities — start slowly and build up as heart gets stronger; try to exercise at the same time of the day so it becomes a regular part of lifestyle.
• Obesity and excess weight — People with excess body fat, especially in the waist, are more likely to develop heart disease and stroke even without other risk factors. Excess weight increases the strain on the heart. It also raises blood pressure, blood cholesterol, and triglyceride levels, and lowers HDL (good) cholesterol levels.
• Lifestyle change: Talk with physician or nurse for recommendation of the best treatment. Lose weight slowly, following Dietary Guidelines For Americans using the Food Guide Pyramid. Eat less fat, especially saturated fat. Be active for at least 30 minutes each day on most days of the week.
• Heart disease — Heart disease is one of the most preventable diseases in existence. Numerous studies have demonstrated that commitment to basic lifestyle changes significantly reduces the chance of having a first heart attack and can reduce the overall risk for heart disease.
• Lifestyle change: Lowering the risk for heart disease is easier than most people think. Eat a sensible diet low in fat, saturated fat, and cholesterol. Schedule time for physical activity. Stop smoking. Get regular medical check-ups and follow professional advice to control blood pressure, cholesterol, and body weight. Visit dental professionals regularly, practicing thorough oral hygiene every day.
Future risk factor?
• Periodontal disease — Periodontal disease is a threat to oral and general health. Periodontal disease is a bacterial infection, and all infections are cause for concern. Research from the American Academy of Periodontology is suggesting that oral bacteria in the bloodstream may contribute to the development of heart disease; increase the risk of stroke; increase a woman's risk of having a preterm, low birth weight baby; pose a serious threat to people whose health is compromised by diabetes, respiratory diseases, or osteoporosis.
• Lifestyle change: The fundamentals have not changed — brush and floss daily, eat properly, see dental professionals regularly, and avoid tobacco products. It is important to make time for routine daily oral care needed to prevent cavities, periodontal diseases, and CVD.
Other factors that contribute to heart disease risk
• Passive smoking — Inhalation of environmental tobacco smoke has also been shown to be associated with an increased risk of smoking-related disease. All individuals, and especially those with other risk factors, should try to avoid exposure to passive smoke.
• Stress — Individual response to stress may be a contributing factor. Some scientists have noted a relationship between coronary heart disease risk and stress in a person's life, their health behaviors and socioeconomic status.
• Sex hormones — Sex hormones seem to play a role in heart disease. It is well known that men have more heart attacks than women do before women reach the age of menopause.
• Alcohol — Drinking too much alcohol can raise blood pressure, cause heart failure, and lead to stroke. It can contribute to high triglycerides, cancer and other diseases, and produce irregular heartbeats. It contributes to obesity, alcoholism, suicide.
• Chronic depression — Depression has been linked with a higher risk of developing high blood pressure, heart disease and having a heart attack.
• Diabetes — Persons with diabetes may be more likely to develop heart related diseases. Preventative care is crucial to the overall health and heart function of diabetic patients.
null