Uremic glossitis: A silent clue in the oral cavity of renal patients
In the vast landscape of oral mucosal disease, uremic glossitis—or more broadly, uremic stomatitis—remains an underrecognized manifestation of systemic illness, most notably chronic kidney disease (CKD).1
While the medical community is aware of the systemic consequences of end-stage renal disease, oral signs such as glossitis often go unnoticed or misattributed. For dental professionals committed to systemic-dental integration, understanding uremic mucosal changes offers an opportunity for early identification, patient education, and interdisciplinary care.
What is uremic glossitis?
Uremic glossitis refers to inflammation of the tongue resulting from the accumulation of nitrogenous waste products in patients with impaired renal function. When the kidneys fail to effectively excrete urea, creatinine, and other metabolites, these toxins accumulate in the bloodstream, causing a condition known as uremia. The oral mucosa, especially the highly vascular and rapidly renewing tissues of the tongue, becomes a vulnerable site for these biochemical imbalances to manifest.2
Although often overshadowed by more severe systemic symptoms of uremia, glossitis may present subtly at first, often as burning, soreness, or erythema of the tongue.3 These symptoms may fluctuate throughout the day, with many patients reporting worsening discomfort in the evening, a pattern that may be influenced by circadian toxin accumulation, dehydration, and reduced salivary flow.
Clinical features of uremic glossitis
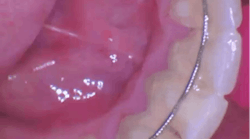
Uremic glossitis can present in several forms, depending on severity and chronicity. The most common findings include:
- Generalized erythema of the dorsum of the tongue
- Burning sensation, often described as dysesthesia
- Smooth, atrophic appearance due to loss of papillae
- Ulcerations or erosions in severe cases, sometimes with a pseudomembranous coating resembling candidiasis
- Halitosis and xerostomia, common in coexisting uremic stomatitis
In broader cases of uremic stomatitis, lesions may extend to the buccal mucosa, gingiva, and palate, occasionally with a characteristic ammonia-like odor due to elevated salivary urea breakdown into ammonia by urease-producing bacteria.4
Pathophysiology and contributing factors of uremic glossitis
The exact pathogenesis of uremic glossitis is multifactorial.5 Elevated urea levels diffuse into salivary secretions, where enzymatic conversion to ammonia may lead to chemical irritation and mucosal breakdown.6 Additionally, chronic inflammation, oxidative stress, and compromised immune function, hallmarks of CKD, contribute to poor mucosal healing.7
Moreover, patients with renal disease are often on complex polypharmacy regimens. Medications such as opioids (e.g., OxyContin) and nonsteroidal anti-inflammatory drugs (NSAIDs) not only induce xerostomia but may contribute to mucosal sensitivity and delayed epithelial regeneration. These drugs, combined with nutritional deficiencies (e.g., vitamin B12, iron, folate) commonly seen in renal patients, create a perfect storm for mucosal vulnerability.
Why dental professionals should pay attention to uremic glossitis
The tongue can serve as a diagnostic canvas for systemic conditions. In renal patients, particularly those undergoing dialysis or with late-stage CKD, oral lesions may be among the earliest signs of metabolic imbalance. Because glossitis is often dismissed as nonspecific or attributed to local irritants, the dental professional’s ability to correlate symptoms with systemic status is essential.
Additionally, glossitis may affect patients' nutrition, speech, and quality of life. Pain or burning may deter eating, further compounding an already fragile health status. Recognizing and documenting these symptoms contributes to comprehensive care.
Diagnostic and management considerations of uremic glossitis
Diagnosis of uremic glossitis is clinical and should be supported by a detailed medical history, including renal function status and medication review. Collaboration with nephrologists can confirm systemic uremia, guide timing of dialysis, and address nutritional support.8
Management is largely supportive and palliative:
- Salivary substitutes and hydration strategies to manage xerostomia
- Topical analgesics or anesthetics for burning
- Vitamin supplementation when deficiencies are suspected
- Referral for systemic evaluation when mucosal signs appear disproportionate to known renal status
What dental professionals should understand about uremic glossitis
Uremic glossitis is more than an oral manifestation—it is a visible signal of systemic dysfunction. For dental professionals, especially those working in hospital settings or with medically complex patients, being attuned to such signs expands our role from localized care providers to critical contributors in holistic health management. Or as I like to put it, in a world where chronic disease is on the rise, the tongue may speak before the kidneys cry out.
References
- Basilicata M, Di Lauro M, Campolattano V, et al. Natural bioactive compounds in the management of oral diseases in nephropathic patients. In J Env Res Publ Health. 2022;19(3):1665. doi:10.3390/ijerph19031665
- Martí ÁlamoS, Gavaldá Esteve C, Sarrión Pérez MG. Dental considerations for the patient with renal disease. J Clin Experiment Dent. 2011;3(2):e112-e119
- Oyetola EO, Owotade FJ, Agbelusi GA, Fatusi OA, Sanusi AA. Oral findings in chronic kidney disease: implications for management in developing countries. BMC Oral Health. 2015;15:24. doi:10.1186/s12903-015-0004-z
- Chuang SF, Sung JM, Kuo SC, Huang JJ, Lee SY. Oral and dental manifestations in diabetic and nondiabetic uremic patients receiving hemodialysis. Oral Surg Oral Med Oral Path Oral Radiol Endo. 2005;99(6):689-695. doi:10.1016/j.tripleo.2004.06.078
- Costantinides F, Castronovo G, Vettori E, et al. Dental care for patients with end-stage renal disease and undergoing hemodialysis. Int J Dent. 2018;2018:9610892. doi:10.1155/2018/9610892
- Davidovich E, Dadiovitz M, Eidelman E, Schwarz Z, Bimstein E. Pathophysiology, therapy, and oral implications of renal failure in children and adolescents. Pediatr Dent. 2005;27(2):98-106.
- Elhusseiny GA, Saleh W. Oral health in children with chronic kidney disease, hemodialysis, and renal transplantation: a comprehensive narrative review of the oral manifestations and dental implications. Clin Med Insight Pediatr. 2024;18(8):11795565241271689. doi:10.1177/11795565241271689
- Proctor R, Kumar N, Stein A, Moles D, Porter S. Oral and dental aspects of chronic renal failure. J Dent Res. 2005;84(3):199-208. doi:10.1177/154405910508400301
About the Author

Andreina Sucre, MSc, RDH
Andreina Sucre, MSc, RDH, is an international dentist, oral pathology, and oral surgery specialist practicing dental hygiene in Miami, Florida. A passionate advocate for early pathological diagnosis, she empowers colleagues through lectures focused on oral pathologies. Andreina spoke on this topic at the 2024 ADHA Annual Conference, 2023 RDH Under One Roof, and she writes about oral pathology for RDH magazine. Committed to community outreach, she educates non-native English-speaking children on oral health and actively volunteers in dental initiatives.