Mumps: Back from the past
There have been numerous news reports in recent months of outbreaks of mumps in parts of the U.S. The incidence of this not-so-common virus has prompted many questions about what it is, how it is transmitted, and whether or not dental health professionals are at risk of exposure.
Let’s look at some facts about mumps. It’s an acute infection caused by the mumps virus. Symptoms are headache, muscle aches, fever, fatigue, and loss of appetite. These are followed by swelling of the parotid, sub-lingual and sub-mandibular salivary glands. The mumps infection can cause serious complications, although these are rare. Complications include encephalitis or meningitis, orchitis (inflammation of the testicles), oophoritis or mastitis (inflammation of the ovaries or breasts), spontaneous abortion and permanent deafness.
Because it replicates in the upper respiratory tract, the mumps virus is easily spread through direct or indirect contact with respiratory secretions or saliva. Infections can be caused by close contact with people who are coughing and sneezing, or by touching contaminated things. Individuals infected with the mumps virus can be infectious from three days before their symptoms occur to about nine days after symptoms appear. According to the Centers for Disease Control and Prevention (CDC), the time period between when a person is exposed to the virus to the onset of symptoms ranges from 12 to 25 days.
Diagnosis of mumps should be made by a physician and may require laboratory testing. There is currently no specific treatment for mumps beyond supporting treatments such as rest, fluids, and fever reducing medications.
Because there has been widespread vaccination against mumps for many years, mumps outbreaks have not been commonplace in the U.S. The mumps vaccine was introduced in 1967, and routine vaccination of children was implemented by 1977. Mumps vaccine is part of the MMR (measles, mumps and rubella) vaccine, which is administered in two doses. The first dose is given at 12 to 15 months of age, and the second at 4 to 6 years of age. The vaccine is believed to be 80 percent effective with one dose, and 90 percent effective with two doses.
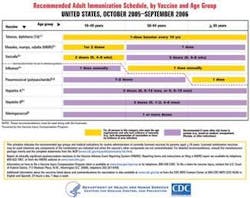
The CDC recommends that people born before 1957 have an additional dose of vaccine. It has been generally accepted that people born before 1957 acquired immunity through exposure to the disease. For additional information about the MMR vaccine, contact a physician, the local health department, or the CDC at www.cdc.gov/nip or 800-232-4636. It is always a good idea to discuss vaccinations with your physician, since dental health professionals have increased risk of exposure to infectious diseases. The CDC issues recommendations for all the vaccines it believes are important for adults. These are listed in the table at left.
Since it has been nearly 40 years since the introduction of the mumps
vaccine, what precipitated this outbreak? According to the CDC, the recent outbreak may have started on a college campus in Iowa. On college campuses, many people live, study and recreate in close proximity, which increases the chances of disease outbreaks. From the college campus, it is believed the disease was spread by infected persons traveling on airplanes, where people are also in close proximity.
Besides the cases identified in Iowa, mumps has been identified in Arkansas, Colorado, Illinois, Kansas, Mississippi, Missouri, Minnesota, Nebraska, New York, Pennsylvania, South Dakota, and Wisconsin.
Dental professionals risk exposure to mumps through contact with secretions from the upper respiratory system or saliva of infected people. Patients who report symptoms of mumps should be rescheduled for treatment. Standard infection control protocols for sterilization of surfaces and instruments should be followed in all dental facilities. It is also important to follow appropriate guidelines for wearing personal protective equipment, particularly facemasks and eye protection. Hand washing is another important preventive technique.
There is no reason to panic about this mumps outbreak. It is prudent, however, to be aware of any new developments or outbreaks in your local area. To find out the most current information on infectious disease developments, regularly check the CDC Web site at www.cdc.gov. If you have questions about your immunity to mumps, check with your physician.