Infection Control and Herpes Simplex
by Noel Brandon Kelsch, RDHAP
Since I was 17 years old there has always been one thing that seems to be the tipping point and stress indicator for me. It is a giant marble-sized herpetic lesion on the center of my lower lip. It always happens at the worst time: when I am going to speak to thousands of people, just before my child's wedding (that he gave me less than a week to prepare for), the same day the battery died, my keys were locked in the car, and someone needed my purse more than I did.
We all know the mucosal lining of the mouth can be a site and a portal for infection. Herpes infection is one of the diseases that love this area. In the dental setting, we need to be very aware of herpes and practice infection control measures to prevent the spread of this disease in the dental environment. Herpes simplex virus (HSV) infection, often called a cold sore, is a disease that few people want to talk about, but everyone needs to know about.
Dispelling myths: What are herpes and where can they occur?
The word "herpes" means "creep." This is a trait that truly belongs to this virus. It creeps along the neural pathway to the dorsal root ganglia, where it can remain inactive for a period of time until the host becomes susceptible. Herpes simplex virus can cause infections of both the mucous membrane and the skin. It is one of a group of viruses that can cause more serious conditions, such as Kaposi's sarcoma and the varicella-zoster virus (commonly called herpes zoster, the mother of chicken pox and shingles).
There are over 80 types of herpesvirus. Years ago, the HSV-1 and -2 viruses were differentiated by the location (-1 in the oral cavity and -2 in the genital area). These viruses are now told apart by the proteins on their surfaces. The location is no longer a determination of the strain of the disease. They can both occur in one person and in both locations.
We are learning a lot about these viruses. In the past, it was thought that HSV-1 occurred in the oral cavity and was not sexually transmitted. Yes, I said it: sexually transmitted. This is something you need to know and need to be able to talk about with your patients. HSV-2 was the bad boy that resulted from sexual activity. Recent studies have dispelled that myth. HSV-1 causes half the genital cases in developed countries. Both types are found in both areas of the body.
How is the disease transmitted?
The chain of infection with this disease is no different than any other disease. You must have the following:
The pathogen: HSV-1 and -2
The source -- Infected individual in the stage of shedding.
Mode -- The herpes simplex virus passes through bodily fluids (such as saliva, semen, or fluid in the female genital tract) or in the fluid from a herpes sore.
Entry -- The virus must have direct access to the uninfected person through their skin or mucous membranes (such as the mouth or genital area).
Susceptible host -- Once HSV enters the body, the virus enters vulnerable cells in the lower layers of skin tissue and tries to reproduce right in the middle of the cell nuclei. At first there are no symptoms. Once the virus starts multiplying, blisters will form and ulcers will start to appear. Over time, the fluid is absorbed by the body and scabs over. Typically, there is no scarring as it heals. It then is carried to the nerve branches and nerve cell ends. It can remain latent there and the host cell and virus will survive in harmony. At unpredictable times, the virus will crop up again. This stage is called the shedding stage. Anytime a person is shedding, the virus can be passed into body fluids and infect other people. Most of the time, the infected person cannot tell if he or she is shedding and is infectious. During shedding, the blisters will come back and most people will have sores. Health, diet, and stress play a major role in the determination of the susceptible host.
Should I see patients who have active oral herpes?
Yes, you can treat patients with herpetic lesions. The important part is that you are rendering the proper treatment. According to the Centers for Disease Control and Prevention (CDC), there are two treatments you should be rendering: emergency treatment for dental conditions and treatment of the lesions. No other treatment should be rendered.
The spreading of this disease in the dental setting is well documented. The vesicular fluid has the most condensed virus and it diminishes as the blisters rupture. Viral shedding continues from the healing lesion. Another issue is that a person who harbors the virus can shed asymptomatically. HSV can cause persistent infection and is shed in saliva. There is also evidence of transmission of HSV to health-care workers from patients and from dental workers to patients. This includes an outbreak of HSV-1 gingivostomatitis in 20 of 46 patients who received treatment from a hygienist who had a herpetic whitlow (lesion on the finger) and did not use gloves. Gloves are not a complete protection against this virus. Pathogens can enter through small defects in the gloves and health-care workers can be contaminated during use or after the removal of gloves.
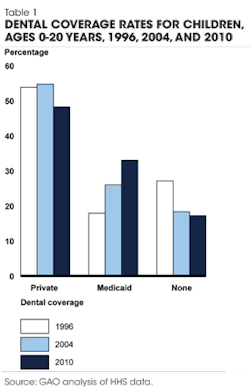
Disease or problem | Work restriction | Duration |
Herpes simplex: genital | No restriction | |
Herpes simplex: hands (herpetic whitlow) | Restrict from patient contact and contact with patient's environment. | Until lesions heal |
Herpes simplex: orofacial | Evaluate need to restrict from care of patients at high risk. | Until lesions heal |
This is also complicated by the fact that HSV can survive for hours in fluids and on environmental surfaces, including counters and dental charts. Dental handpieces have also been found to be a source of possible transmission. Reports of occupationally-acquired HSV have become less frequent with the use of personal protective barriers. The infection control measure that should be practiced most often is to simply not see the patient for elective treatment when there is an active infection.
Treatments that shorten healing time for an active lesion should be considered the treatment of choice for all dental health-care professionals. Those could include laser treatment, topical medicaments, and antiviral medications. Visits to the dentist can trigger lesions in some people. Studies have shown that taking an antiviral before dental treatment can decrease the rate of lesions. Elective treatment should be postponed until the lesion has healed completely. Though the patient may be comfortable after you have applied a topical medication, there is still the risk of spreading the disease to the health-care provider.
Can I see patients if I have active herpes?
The CDC Guidelines for Infection Control in the Dental Setting 2003 gives the following guidelines:
Because herpes is transmittable to patients from dental health-care professionals who have active lesions, there is a risk of spreading this disease. The guidelines from the CDC are clear. Each of us has to keep patient safety and staff safety a priority.
Communication
There is a stigma surrounding this disease and, just like any other disease, we as health-care professionals need to end that stigma. At one point in history, it was thought to be a disease associated with people who live risky lifestyles. The understanding of this disease has evolved and we all know that there are many methods of transmission. Our own prejudices may interfere with talking about this disease with patients. We need to put aside our own biases about this oral disease and talk about it just like dental caries or gingivitis. Openly communicating the risk factors, treatment, and protocols is vital to the health of patients as well as clinicians. Let patients know that if they are developing a lesion or have an active lesion, elective treatment will be postponed – but there is treatment for the disease itself in the dental setting (laser, topical medications, and antivirals).
Three open-ended, nonjudgmental questions?
Question Do you ever get cold sores?
Follow-up If you feel one coming on, please come in. We have methods of treating this disease. We will postpone elective treatment during that time, but we can treat HSV.
Question Have you ever been diagnosed with herpes simplex virus?
Follow-up Cold sores are the common name for herpes simplex virus, which is a transmittable disease. An estimated 57% of the population has oral herpes.
Question Are you aware of how this disease can be spread?
Follow-up Years ago, they thought that this disease was spread through kissing and in intimate moments. There are many ways it can be spread. It is important that you limit your exposure to others when you have an active infection, especially skin-to-skin contact.
Question Do you want information on self-care?
Follow-up Explain the methods of treatment and prevention.
Question Do you want information on preventing the spread of this disease?
Follow-up Give information and resources on preventing the spread of the disease.
I seldom get a full-blown cold sore anymore. I call my dental health-care professional just as soon as I feel one coming on and get my treatment of choice. I am working on the stress that seems to trigger my oral episodes. I know that infection control is necessary, and open-ended, nonjudgmental questions can end the stigma associated with this disease. My patients have taken infection control to another level by calling the office to postpone treatment if they have active lesions. RDH
Consider reading:Disasters happen: Ensuring water safety
Consider reading:Preparing for hazard communication changes in 2013
Consider reading:Dental Laboratories And Infection Control
References
1. Chang TW, Gorbach SL. Primary and recurrent herpetic whitlow. Int J Dermatol 1977; 16:752-4.
2. Epstein JB, Rea G, Sibau L, Sherlock CH, Le ND. Assessing viral retention and elimination in rotary dental instruments. J Am Dent Assoc. 1995; 126:87-92.
3. Centers for Disease Control and Prevention. Guidelines for Infection Control in Dental Health-Care Settings – 2003. www.cdc.gov/mmwr/preview/mmwrhtml/rr5217a1.htm. 2013.
4. Kotilainen HR, Brinker JP, Avato JL, Gantz NM. Latex and vinyl examination gloves. Quality control procedures and implications for health care workers. Arch Intern Med. 1989; 149(12):2749-53.
5. Leimone CA, Marozzi M. The transmission and prevention of hepatitis and herpes in the dental office. Dent Assist. 1984; 53(6):21-5.
6. Lewis MA. Herpes simplex virus: an occupational hazard in dentistry. Int Dent J. 2004; 54(2):103-11.
7. Manzella JP, McConville JH, Valenti W, Menegus MA, Swierkosz EM, Arens M. An outbreak of herpes simplex virus type I gingivostomatitis in a dental hygiene practice. JAMA. 1984; 252:2019-22.
8. Matusow RJ. Acute primary herpetic gingivostomatitis in non-immunocompromised adults and HSV-1 isolation technique. Compendium. 1992; 13:662–666.
9. McCarthy G. Risk of transmission of viruses in the dental office. J Can Dent Assoc. 2000; 66:554-5, 557.
10. McCarthy JP, Browning WD, Teerlink C, Veit G. Treatment of herpes labialis: comparison of two OTC drugs and untreated controls. J Esthet Restor Dent. 2012; 24(2):103-109.
11. Merchant VA. An update on the herpes viruses. J Calif Dent Assoc. 1996; 24(1):38-46.
12. Olsen RJ, Lynch P, Coyle MB, Cummings J, Bokete T, Stamm WE. Examination gloves as barriers to hand contamination in clinical practice. JAMA. 1993; 270(3):350-3.
13. Scully C. Herpes simplex virus (HSV). In: Millard HD, Mason DK, eds. World Workshop on Oral Medicine, 1988 Jun 19-25. Chicago: Year Book Medical Publishers, 1989.
14. Tenorio AR, Badri SM, Sahgal NB, Hota B, et al. Effectiveness of gloves in the prevention of handcarriage of vancomycin-resistant enterococcus species by health care workers after patient care. Clin Infect Dis. 2001; 32(5):826-9.
NOEL BRANDON KELSCH, RDHAP, is a syndicated columnist, writer, speaker, and cartoonist. She serves on the editorial review committee for the Organization for Safety, Asepsis and Prevention newsletter and has received many national awards. Kelsch owns her dental hygiene practice that focuses on access to care for all and helps facilitate the Simi Valley Free Dental Clinic. She has devoted much of her 35 years in dentistry to educating people about the devastating effects of methamphetamines and drug use. She is a past president of the California Dental Hygienists' Association.
Past RDH Issues